Outline
Safety of Ultrasound Examination, 3
Indications for Obstetric Ultrasound Examination, 4
Who Should Perform the Ultrasound Examination and How Should It Be Performed?, 5
Nonmedical Use of Ultrasonography, 5
Terminology, 5
Ultrasound Lexicon, 6
The American Institute of Ultrasound in Medicine Guidelines, 6
Ultrasound Equipment and Documentation, 6
The First Trimester Ultrasound Examination, 6
Identification of an Intrauterine Pregnancy, 6
Embryonic/Fetal Number, 12
Estimating Gestational Age, 12
Morphologic Abnormalities, 12
Placenta, 12
Uterus and Adnexa, 13
The Second and Third Trimester Ultrasound Examinations, 13
Fetal Number and Fetal Life, 13
Fetal Position, 13
Assigning Gestational Age and Weight, 13
Amniotic Fluid Volume, 15
Amniotic Fluid Volume in Multiple Gestations, 16
Placenta, 16
Fetal Malformations, 17
Uterus and Adnexa, 17
Verbiage Used in the AIUM/ACR/ACOG Guidelines, 17
Interpretation of the Ultrasound Examination, 18
Reporting of Ultrasound Results, 18
Discussing the Examination With the Patient, 19
Evaluating the Obstetric-Gynecologic Ultrasound Literature, 20
Malpractice and the Obstetric Ultrasound Examination, 20
Conclusion, 21
Summary of Key Points
- •
Recent years have seen dramatic advances in ultrasound technology, including improved spatial and contrast resolution, routine use of three-dimensional (3D) and four-dimensional (4D) imaging, volumetric scanning, expanded indications for color and spectral Doppler, new and improved ultrasound scanning probes, and improved digital review workstations.
- •
With improved imaging comes the complicating corollary as to what minor findings should be reported to the patient and which merely lead to unnecessary anxiety.
- •
Although there is high-quality evidence that ultrasound is safe for the fetus when used appropriately, consensus statements conclude that Doppler examination of fetal vessels in early pregnancy should not be performed without a clinical indication.
- •
The nonmedical use of ultrasound for psychosocial or entertainment purposes is strongly discouraged by professional organizations such as the American Institute of Ultrasound in Medicine (AIUM).
- •
Only those with adequate training in a conventional training program should be performing and interpreting ultrasound examinations.
- •
Consensus guidelines and criteria for transvaginal sonographic diagnosis of pregnancy failure in a woman with an intrauterine pregnancy of uncertain viability have been established and should be followed.
- •
Although early detection of a morphologic abnormality is useful, the confident unequivocal detection of an abnormality is even more important. Unless one is extremely confident of the existence of an abnormality in the first trimester, a follow-up examination should be performed.
- •
Measurements made early in pregnancy, for the most part, are more accurate than those made near term.
- •
Although a diagnosis of oligohydramnios and polyhydramnios can be made subjectively, the extremes of amniotic fluid volume should also be assessed objectively using either the deepest vertical pocket (DVP) or amniotic fluid index (AFI).
- •
It is preferable to report the distance from the inferior edge of the placenta to the internal cervical os rather than relying on terms that may have differing meanings (e.g., marginal placenta).
- •
If a single obstetric ultrasound or a targeted examination is performed, it should be done at a gestational age of 18 to 20 weeks.
- •
Obstetric ultrasound examinations represented the majority of medical malpractice cases involving ultrasound.
- •
Ultrasound examination is a noninvasive, safe procedure that has a high degree of patient acceptance and can yield a wealth of information.
It has now been over 4 decades since sonography was first used to evaluate the obstetric patient. At first, the questions this modality sought to answer were very basic: Is there a pregnancy? Is the fetus alive? Is there a singleton or a twin gestation? What is the location of the placenta? What is the gestational age? Probably, few envisioned the day when ultrasonography would be used to identify subtle anatomic defects such as cleft lip or palate, to predict obstetric complications such as placenta accreta, or to accurately detect the presence of fetal anemia. It is hard to believe that, at its inception, it was difficult to convince clinicians as to the usefulness of this new diagnostic modality in obstetric management. Now, it is routine for a patient to have at least one, and often several, ultrasound examinations during her pregnancy. The technologic advances in ultrasound imaging, including 3D/4D and volumetric measurements, the use of high-frequency transvaginal probes, and the utility for chromosomal screening in early pregnancy (e.g., nuchal translucency) have only expanded the indications for sonographic imaging in the obstetric patient.
Since the last edition of this textbook, there have been dramatic advances in ultrasound technology, including improved spatial and contrast resolution, routine use of 3D and 4D imaging, volumetric scanning, expanded indications for color and spectral Doppler, new and improved ultrasound scanning probes, and improved digital review workstations, to name a few. Likewise, our knowledge of normal fetal anatomy and pathology, and the pathophysiology of disease in general, has increased substantially. The Internet has made communication among and between researchers and clinicians easier. In addition, there have been many collaborative studies and refinements of the guidelines for the performance of the obstetric ultrasound examination. However, there are still differences in the approach to the obstetric ultrasound examination from one group to the next. Although guidelines have improved consistency in the conduct and reporting of obstetric examinations, several issues are often hotly debated: for example, what constitutes a basic ultrasound examination, what structures should be evaluated, what is the ideal timing of the examination, what is the appropriate role of the first trimester anatomic survey, who should perform and interpret the examination, how safe is ultrasound, how should it be recorded and documented, how should it be reported, and last, how should the patient be told the results of the examination? With improved images comes the complicating corollary as to what minor findings should be reported to the patient and which merely lead to unnecessary anxiety. These issues are addressed later in the text and some of them are discussed here.
Safety of Ultrasound Examination
It was not long after the inception of ultrasound imaging that questions were raised as to the safety of this new modality. Despite numerous claims for the safety of ultrasound to the mother and fetus, a number of studies have noted possible adverse effects of diagnostic ultrasound to the developing fetus. These studies have focused primarily on thermal and cavitation mechanisms leading to possible injuries to the developing fetus.
Absorption of the ultrasound wave’s energy by soft tissue and bone, and its conversion to heat, are measured by the thermal index (TI). A TI of 1 means an increase of 1° C. Several studies have suggested a general threshold of temperature elevation of 1.5° to 2° C above maternal core temperature before any evidence of a developmental effect occurs. With modern ultrasound machines, there is only a negligible rise in temperature, usually less than 1° C. The World Federation for Ultrasound in Medicine and Biology has stated that “a diagnostic exposure that produces a maximum in situ temperature rise of not more than 1.5° C above normal physiological levels may be used without reservation on thermal grounds.” However, this organization further stated that “a diagnostic exposure that elevates embryonic and fetal in situ temperature above 41° C for 5 minutes should be considered potentially hazardous.” The conclusion overall is that it is unlikely that there is a deleterious effect of ultrasound in the first trimester during embryogenesis with routine gray-scale ultrasound.
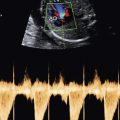
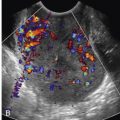
However, when Doppler ultrasound is used during the first trimester, it is likely that temperature increases of over 1.5° C may occur. Studies of the effect of Doppler on soft tissues adjacent to bone and nerve conductance demonstrated a significant rise in temperature when the ultrasound Doppler beam was held for more than 30 seconds. The European Federation for Societies in Medicine and Biology in 1998 concluded that “until further scientific information is available, investigations using pulsed or color Doppler should be carried out with careful control for output levels.” It is recommended that when performing Doppler imaging in early pregnancy, the displayed TI should be 1.0 or less and exposure time should be kept as short as possible, usually no longer than 5 to 10 minutes and not exceeding 60 minutes. A thermal index for soft tissue (TIs) should be used at earlier than 10 weeks’ gestation, and a thermal index for bone (TIb) should be used at 10 weeks’ gestation or later when bone ossification is evident. In keeping with the ALARA (As Low As Reasonably Achievable) principle of prudent scanning, M-mode imaging should be used instead of spectral Doppler imaging to document embryonic/fetal heart rate. Transvaginal ultrasound is not more harmful than transabdominal scanning; again, the risk is dependent on the TI.
Although the potential for embryonic effects from Doppler imaging exists, there is little evidence that ultrasound is teratogenic. As stated in one editorial on the subject, “Many of the studies to date have shown the embryo to be remarkably resilient to ultrasound exposure. Logic would suggest that Doppler techniques should not affect the embryo if the pulses are applied at a low level.” In one study, Zhu and associates insonated pregnant rats with diagnostic levels of color Doppler ultrasound energy and studied the cell cycles of newborn rats by flow cytometry and factorial analysis. They found that the deoxyribonucleic acid content was not affected in any phase of the cell cycle in newborn rats by any of the different insonation times and frequencies. In another animal study, Pellicer and colleagues examined cellular damage in rats following exposure to low-intensity ultrasound for as long as 10 minutes. These investigators found that the longer the exposure time, the greater the liver cell damage that was observed. Other animal studies have likewise demonstrated a relationship between the length of exposure to Doppler ultrasound and potential effects on the developing brain. Although such studies support caution and minimizing unnecessary exposure, it is unclear whether such animal models can be extrapolated to humans and if such findings are important. However, at the present time, consensus statements conclude that Doppler examination of fetal vessels in early pregnancy should not be performed without a clinical indication.
Cavitation involves the occurrence of gaseous bubble formation in an air-water interface. One concern is that stress from the fluid adjacent to the gaseous body during the process of cavitation may disrupt cell membranes. Cavitation has been difficult to document in mammalian fetuses, because, for the most part, there is not an air-water interface, which is needed for the cavitation mechanism. The mechanical index (MI) is an onscreen indicator that provides a rough guide to the likelihood that ultrasound will induce an adverse biologic effect by a nonthermal mechanism, including cavitation. For all practical purposes, this index is probably not relevant for obstetric scanning owing to the relative absence of gas bubbles (air) in the fetus.
A number of studies have evaluated the effect of prenatal ultrasound on neonatal and infant outcome in animal models. Although some studies have documented lower birth weights, shorter heights, and lowered white blood cell counts in neonates who were scanned in utero compared with control subjects, the size differences disappeared when studied after 3 months. In addition, hematologic parameters normalized by this time. Neurodevelopmental studies revealed no significant differences in motor or cognitive tasks, or in learning skills. Studies evaluating the human fetus and neonate have reached similar conclusions. Studies have found either no difference in birth weights between exposed and nonexposed fetuses, or a difference that, although present at birth, was not present at 6 to 7 years of age.
The information on an association between ultrasound and congenital malformations is limited. Studies evaluating chromosomal aberration and ultrasound exposure have demonstrated little or no change.
The major difficulties with the studies investigating a possible deleterious effect of diagnostic ultrasound evaluation are threefold: (1) experimental ultrasound exposure levels or time of exposure often far exceeded those that are normally used diagnostically; (2) the systems used to show ultrasound effect (plants, cell culture, laboratory animals) may not be applicable to humans; and (3) many studies that have demonstrated adverse effects in vitro have not been reproducible.
One study evaluating the effect of diagnostic ultrasound on neuronal migration in mice raised much attention in the media. Although this is an interesting study in mice, for the reasons stated earlier, it has little to no applicability in humans. There are two major criticisms of this study. Although the study did use commercially available equipment in which only slightly greater ultrasound frequency than normal was used (6.7 MHz vs. 3.5-5.0 MHz), the fixed duration of exposure far exceeded what would normally be used in humans. The study did not demonstrate statistically significant abnormal results until 30 minutes of exposure. More than 10 years ago, when a sonologist wished to determine whether an embryo was nonviable, the recommended evaluation of the embryo was 3 minutes of observation, demonstrating no evidence of embryonic or cardiac activity. Two minutes of evaluation, let alone 3 minutes, seemed like an eternity, and most examiners, in our experience, stopped after 1 minute. In the slightly older embryo and early fetus, greater than 5 to 10 minutes of sustained evaluation of the fetal brain would be excessive. In most cases, the transducer would be moving around the brain rather than being in a fixed position during the examination.
The second criticism relates to the timing of embryology and the relative sizes of the mouse and human brains. As stated by the authors of this study: “The duration of neuronal production and the migratory phase of cortical neurons in the human fetus lasts approximately 18 times longer than in mice (between 6 and 24 weeks of gestation in humans, with the peak occurring between 11 and 15 weeks, compared with the duration of only approximately 1 week (between E11 and E18) in a mouse). Thus an exposure of 30 minutes represents a much smaller time dedicated to the development of the cerebral cortex in the human than in the mouse, and thus could have a lesser overall effect, making human corticogenesis less vulnerable to ultrasound waves.”
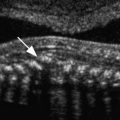
The AIUM statement on the clinical safety of diagnostic ultrasound reiterates previous findings that no confirmed bioeffects caused by exposure at intensities typical of present diagnostic instruments have ever been reported in patients or instrument operators. This statement acknowledges the possibility that bioeffects may be identified in the future but emphasizes the current data indicating that the benefits of the prudent use of diagnostic sonography outweigh the risks, if any. At a recent consensus conference on fetal imaging, it was concluded that there is high-quality evidence that ultrasound is safe for the fetus when used appropriately. However, as stated by Kremkau, “even if this risk is so minimal that it is difficult to identify, prudent practice dictates that routine measures be implemented to minimize the risk while obtaining the necessary information to achieve the diagnostic benefit. This is the ALARA (as low as reasonably achievable) principle of prudent scanning” ( Fig. 1-1 ).

The sonographer’s knowledge of ultrasound and its safety is crucial to the safe implementation of this modality. Merritt, in an editorial, summarized it best: “In view of the rapid growth of sonography and its proliferation into the hands of minimally trained clinicians, it is likely that more patients are harmed each day by misdiagnosis resulting from improper indications, poor examination technique, and errors in interpretation than from all bioeffects.”
Indications for Obstetric Ultrasound Examination
National guidelines from many organizations in the United States and elsewhere, including the American College of Obstetricians and Gynecologists (ACOG), the Royal College of Obstetricians and Gynaecologists, and the Society of Obstetricians and Gynaecologists of Canada, highlight the benefits of obstetric ultrasound examination, including accurate determination of gestational age, fetal number, cardiac activity, placental localization, and diagnosis of major fetal anomalies. Because of these benefits, and because most congenital anomalies occur in patients with no known risk factors, these organizations agree that second trimester ultrasonography should be offered routinely to all pregnant women and should follow specific guidelines. In addition, ACOG recommends that all pregnant women should be offered first trimester screening for aneuploidy, which may include nuchal translucency sonography.
The benefit of routine sonography in the detection of fetal anomalies has been debated. Large studies and systematic reviews report detection rates of 16% to 44% of anomalies prior to 24 weeks of gestation. Higher detection rates of major and lethal anomalies, as high as 84%, have been reported. The sensitivity of anomaly detection has been noted to vary with respect to the type of abnormality, patient factors, gestational age, and expertise of the imager. Possible explanations for the variance in the detection rate of anomalous fetuses may include (1) differences in neonatal assessment, (2) differences in the definition of a major anomaly, (3) a differing risk status of the population, (4) differences in what is considered a routine or standard sonogram, and (5) the expertise of the examiner.
Who Should Perform the Ultrasound Examination and How Should It Be Performed?
Theoretically, the answer to who should perform the ultrasound examination should be extremely easy. In fact, it is one of the most controversial issues relating to the ultrasound examination. The answer should be that only those persons who have had adequate training (including didactic as well as supervised “hands-on” experience) should perform and interpret an ultrasound examination.
More than 30 years ago, the Joint Task Group on Training for Diagnosis in Obstetrical and Gynecologic Ultrasound developed guidelines for the post-resident physician who had completed residency programs in either radiology or obstetrics and gynecology that did not provide formal training in obstetric and gynecologic ultrasound evaluation. These guidelines have been continuously updated, most recently in 2014, and include a recommendation of a minimum experience in obstetric and gynecologic ultrasound evaluation as well as training that includes basic physics, technique, performance, and interpretation. In addition, the physician should obtain practical and supervised experience (at least 300 examinations) before offering services as a physician competent in diagnostic ultrasound examination. Ongoing experience with at least 170 examinations per year is also recommended.
The “turf” battles between radiologists and obstetricians as to who should perform the examination are unfortunate. As long as the examining physician is adequately trained and performs the minimum standard obstetric ultrasound examination, as per the guidelines of the American College of Radiology (ACR), AIUM, and ACOG, the specialty of the examiner does not matter. However, we do not believe in the practice of self-referral. Self-referral examinations tend to be performed more and more frequently and are often less “complete” and of a lower quality than when they are performed by a dedicated ultrasound practitioner. Except in localities where there are no diagnostic ultrasound specialists, patients should be referred to practitioners whose major practice is ultrasonography.
Guidelines for the performance of obstetric ultrasound examinations have been published by ACR, ACOG, and AIUM, and components of the standard fetal examination at 18 to 20 weeks of gestation were published in a consensus report by National Institute of Child Health and Human Development (NICHD), Society for Maternal-Fetal Medicine (SMFM), ACOG, ACR, AIUM, Society of Pediatric Radiology (SPR), and Society of Radiologists in Ultrasound (SRU) in 2014. AIUM has likewise published guidelines for performance of a detailed fetal anatomic survey, referred to by the billing code 76811. Although there may be sonologists who exceed these guidelines, the guidelines serve as a minimum standard for practitioners of basic and detailed obstetric ultrasonography.
Nonmedical Use of Ultrasonography
The AIUM has published a ‘‘prudent use’’ statement, which was also endorsed by ACOG. The AIUM advocates the responsible use of diagnostic ultrasonography and strongly discourages its nonmedical use for psychosocial or entertainment purposes. The use of either 2D or 3D ultrasound imaging only to view the fetus, obtain a picture of the fetus, or determine the fetal sex without a medical indication is inappropriate and contrary to responsible medical practice. Although there are no confirmed biologic effects on patients caused by exposures from present diagnostic ultrasound instruments, the possibility exists that such biologic effects may be identified in the future. Thus, ultrasound imaging should be used in a prudent manner to provide medical benefit to the patient. This position has been ethically defended.
Terminology
The latest classification of fetal sonographic examinations by the AIUM, ACR, and ACOG groups the examinations into four major categories: (A) the first trimester ultrasound examination, (B) the standard second or third trimester examination, (C) the limited examination, and (D) specialized examinations. The standard second and third trimester obstetric examination is often referred to as a routine examination, basic examination, Level 1 examination, or complete ultrasound examination. Specialized examinations might include a detailed anatomic examination, as well as fetal Doppler ultrasound, a biophysical profile, a fetal echocardiogram, and additional biometric measurements. A detailed anatomic examination is generally performed when a patient is at high risk for a fetal anomaly, or when an anomaly is suspected on the basis of the history, biochemical abnormalities or abnormal results on other screening tests, or the results of either the limited or standard scan.
It is important to note that although those individuals performing detailed anatomic examinations must be proficient in evaluating patients for congenital anomalies, it is not acceptable for the Level 1 examiner to be unskilled. In an excellent editorial on the subject, Filly notes that unfortunately some examiners have chosen to use the term “Level 1” as a shield for incompetency. As he states, the Level 1 sonogram is not defined by the technical capability of the examiner, nor by the cost of the sonographic instrumentation employed. In fact, the Level 1 examination “requires a high degree of competency” and should follow the standard second or third trimester obstetric sonographic examination as described in the AIUM/ACR/ACOG guidelines.
The specialized examination (CPT 76811) has been referred to as the Level 2 examination, survey examination, or targeted examination. As the AIUM/ACR/ACOG guidelines state, this is a detailed anatomic examination that is performed when an anomaly is suspected on the basis of history, abnormalities detected on prenatal screening tests, or the results of either a limited or standard examination previously performed.
The individuals performing the sonographic examination are referred to as either sonographers or sonologists. Traditionally, the technical component and initial production of images has been the responsibility of the sonographer (nonphysician), and the professional component and interpretation of images has been the responsibility of the sonologist (physician). The degree of collaboration between the two and their degree of involvement in the ultrasound examination vary from locality to locality. In many parts of the world, examinations are performed predominantly by physicians. Although the contribution of sonographers to the ultrasound examination is invaluable, it should be remembered, as stated by the AIUM, that “Ultrasound studies shall be supervised and interpreted by a physician with training and experience in the specific area of sonography. Findings must be recorded and results communicated in a timely fashion to the health care provider responsible for care. Although a sonographer may play a critical role in extracting the information essential to deriving a diagnosis, the rendering of the final diagnosis of ultrasound studies represents the practice of medicine, and, therefore, is the responsibility of the supervising physician.”
Perhaps the least controversial aspect of this discussion should be who should interpret the ultrasound examination. This, we believe, is straightforward. Only those with adequate training in a conventional training programs (e.g., residency) in which there are didactic lectures, hands-on scanning, and physician supervision in the performance and interpretation of cases should be performing and interpreting ultrasound findings. Training by manufacturer’s training specialists or 1- to 2-week mini-courses do not constitute adequate training in ultrasound.
Ultrasound Lexicon
Undoubtedly, hundreds of terms are used in obstetrics and ultrasonography that are either incorrect or confusing. Many of these terms are addressed later in this chapter and in other chapters in this text. Two areas in which terminology is often either misused or misunderstood in obstetric ultrasonography are fetal life and age. The term viability is defined as the ability to survive in the extrauterine environment. Even in cases of very late third trimester examinations, this statement cannot be used with complete certainty. We prefer to state that the embryo or fetus is living, if that is the case, and use the term nonviable for those embryos or fetuses that either are dead or are not capable of living in the extrauterine environment. Early pregnancy failure is another, perhaps even better, way of communicating this information.
The second often-confused term is gestational age. Taken as it sounds, this term would seem to imply the actual age of the fetus from conception to the present. In fact, this term, which is widely used by obstetricians and sonologists, is most often meant to be synonymous with menstrual age. Menstrual age refers to the length of time calculated from the first day of the last normal menstrual period to the point at which the pregnancy is being assessed. The true age of the embryo or fetus, fetal age , is rarely known accurately unless the patient has had assisted fertilization or has extremely regular menstrual periods and the day of conception is known. In general, the fetal age is 2 weeks less than the menstrual age.
In this text, the terms gestational age and menstrual age are used interchangeably. The important point for any examiner to remember is not which term is necessarily preferable but rather that the person interpreting the examination and the physician who ordered the examination both use the same terminology.
Another often-misused term is fetal pole . This term should be abandoned. It is most often used to describe the presence of the embryo in the early first trimester sonogram. The embryonic period lasts until the end of the 10th menstrual week; during this time the developing conceptus should be referred to as the embryo. Thereafter, the conceptus should be referred to as a fetus.
The American Institute of Ultrasound in Medicine Guidelines
In 2013 the Practice Guideline for the Performance of an Antepartum Obstetric Ultrasound Examination was updated by the AIUM in collaboration with the ACR, the SRU, and ACOG. It is a modification of previously developed guidelines that were first published in 1986. The actual ACR/AIUM/ACOG guidelines are presented in Table 1-1 . What follows is our own bias as to what constitutes an appropriate ultrasound examination. In some respects, this discussion is an expansion of the guidelines previously mentioned. Because this multiauthor text is essentially a detailed review of the obstetric ultrasound examination, we recognize that our viewpoint in this chapter and those of the authors of the subsequent chapters may differ.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree