Chapter 18 Ocular Ultrasound Guided Anesthesia
Introduction
Retrobulbar block
Until recently, the RBB has been the most common regional ophthalmic anesthetic technique. Its roots date to the late 1800s and it was formally described by Atkinson in the early twentieth century.1 Advantages of RBBs include rapid onset of profound akinesia and analgesia while using a minimal volume of local anesthetic. However, complications have been associated with this technique including brainstem anesthesia, globe puncture, and retrobulbar hemorrhage. Therefore, this modality has been largely superseded by other methods.
Peribulbar block
Peribulbar blocks which are placed into the extraconal space may provide a superior safety profile since needles are intentionally guided outside of the orbits’ muscle cone with less depth and angulation.2 Disadvantages of the PBB technique include a longer latency of onset for total block, and the need for greater volumes of local anesthetic agents. Unfortunately, the potential for serious sequelae remain.3
Sub-Tenon’s block
While STBs, using cannulae instead of needles, have been touted by some as being less prone to major complications such as globe puncture and serious hemorrhage, minor complications including conjunctival bleeding and chemosis are more commonly observed. Notably, as more and more STBs are performed, the number of these aforementioned serious complications have been increasingly reported in the literature.4,5
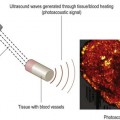
Rationale for USG-guided anesthesia
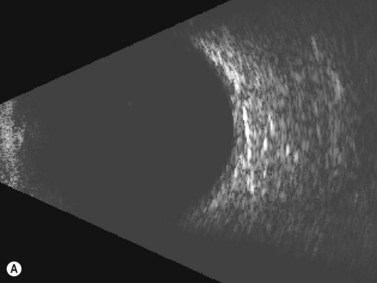
Needle misadventure and penetration or perforation of the globe, leading to potential long-term visual compromise, are arguably the most feared complications of ophthalmic anesthesia. Fortunately, in the hands of trained and experienced physicians, such complications are exceedingly rare.6 Needle-based eye blocks are “blind” techniques that are dependent upon surface anatomy landmarks in order to position the needle correctly. An office-based ultrasound A- or B-scan may provide information as to the globe’s axial length and morphology of the eye in order to detect an atypically long or asymmetric, possibly staphylomatous eye.7 Fundamentally, a RBB is conducted by intentionally angling the needle steeply and deeply within the orbit behind the globe. If the globe is longer than anticipated, or a staphyloma is prominent, greater risk of needle injury to the eye’s posterior portion exists.8 Using ultrasound to visualize important anatomy during the procedure may be of utility (Figure 18.1). Training and experience is of paramount importance in order to use this method with skill.
Purportedly, there is less likelihood to puncture or perforate the globe when one is using a PBB, which entails shallower needle placement with less angulation towards the orbital apex. However, longer globes have greater volume and increased superior/inferior girth, thus exposing the inferior aspect to needle trauma. Therefore, the risk of globe puncture remains.8
Published studies
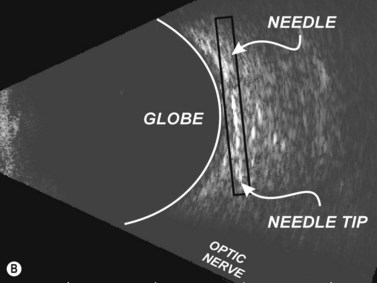
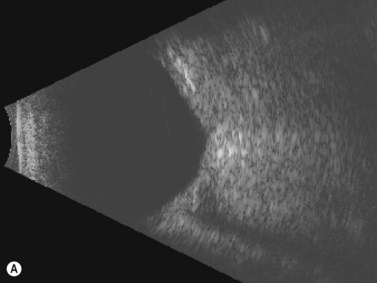
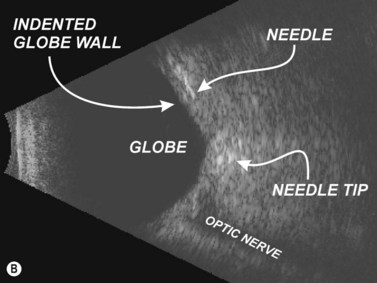
In 1995, Birch et al described the use of ultrasound block to localize 25 gauge 38 mm needles during RBB.9 Initially, each ophthalmologist performing a RBB estimated the distance between needle tip and the posterior globe as being greater than 5 mm. Sonographic images were obtained prior to needle placement, with the needle in situ, and upon injection of local anesthetic. In each block, the needle tip, according to ultrasonographic interpretation, was noted to be significantly closer to the globe than each ophthalmologist had estimated. True needle tip distances were found to be as little as 0.2 mm behind the globe’s posterior pole. The greatest distance was 3.3 mm! While no globe perforations or penetrations were encountered, the needle shaft was observed to indent the globe in over half of the RBBs in this series. (Others have not reproduced this finding.)10 Probe tension on the eye can deform the globe by causing it to be balloted against the needle shaft (Figure 18.2). Releasing pressure from the array allows the eye to revert to its usual position. Ultimately, Birch et al concluded that the use of external anatomic landmarks alone might be insufficient.9
Winder et al studied both the RBB and PBB ultrasound-guided techniques.10 Ultrasonography was performed prior to, during and 10 minutes after injection of local anesthetics. As expected, anechoic local anesthetic was initially seen within the muscle cone for RBBs, and outside of the cone for PBBs. Ten minutes after PBB, sonography demonstrated that the local anesthetics, placed extraconally, had travelled into the intraconal space thus confirming the mechanism of achieving orbital anesthesia with peribulbar injection. In contrast to Birch et al, there were no cases of needle contact with sclera.
Luyet et al performed a series of ultrasound-guided needle-based eye blocks on cadaveric specimens.11 They found that key structures within the orbit, notably the globe’s rim and optic nerve, as well as the needle and injected fluids were readily visualized. Notably, visualization was facilitated due to use of needles that were considerably larger than those typically used on live patients. Nonetheless, ultrasound-guided procedure feasibility was demonstrated. The need for additional research in this arena is warranted.