Functions
• General somatic efferent (GSE). Somatic motor innervation to
 Inferior rectus (IR). Depresses eye.
Inferior rectus (IR). Depresses eye.
 Superior rectus (SR). Elevates eye.
Superior rectus (SR). Elevates eye.
 Medial rectus (MR). Adducts eye.
Medial rectus (MR). Adducts eye.
 Inferior oblique (IO). Elevates eye when eye adducted; extorts (laterally rotates) eye when eye abducted.
Inferior oblique (IO). Elevates eye when eye adducted; extorts (laterally rotates) eye when eye abducted.
 Levator palpebrae superioris (LPS). Raises eyelid.
Levator palpebrae superioris (LPS). Raises eyelid.
• General visceral efferent (GVE). Parasympathetic innervation to
 Sphincter pupillae. Constricts pupil (miosis).
Sphincter pupillae. Constricts pupil (miosis).
 Ciliary muscles. Contraction causes lens to bulge (accommodation).
Ciliary muscles. Contraction causes lens to bulge (accommodation).
Anatomy
• The oculomotor nuclear complex is in the midbrain at the level of the superior colliculus, ventral to the cerebral aqueduct (separated by periaqueductal gray matter, PAG) and dorsal to the medial longitudinal fasciculus (MLF) (Figs. 3.1, 3.2, 3.3).
• Subnuclei supply individual muscles. Lateral subnuclei supply the ipsilateral IR, IO, and MR muscles. Medial subnucleus supplies contralateral SR (via decussating axons). Central subnucleus in the midline supplies the LPS bilaterally.
• The Edinger-Westphal nucleus is in the rostral portion of the oculomotor nuclear complex and supplies preganglionic parasympathetic innervation.
Nerve Course
• Fascicular portion. Lower motor nerve (LMN) axons (with parasympathetic fibers located dorsal and superficial to somatic motor axons) course through the tegmentum of the midbrain, traversing the MLF and decussating fibers of the superior cerebellar peduncle (SCP), the red nucleus (RN), and the medial aspect of the cerebral peduncles to exit the midbrain and enter the interpeduncular cistern at the midbrain—pons junction.
• Subarachnoid portion (in cistern). Nerve passes between posterior cerebral artery (PCA) and superior cerebellar artery (SCA), courses forward inferolateral to the posterior communicating artery (PCommA) and medial to the uncus, pierces the dura lateral to posterior clinoid process, and enters the “oculomotor triangle” (formed by dural folds from tentorium cerebelli attachments) in the posterior roof of the cavernous sinus to wind up in the superolateral wall of the cavernous sinus (superior to cranial nerve [CN] IV) (Fig. 3.4).
• After traversing the cavernous sinus, CN III reaches the superior orbital fissure (SOF), where it divides into superior and inferior divisions, both of which pass into the orbit through the annulus of Zinn. The superior division ascends lateral to the optic nerve to supply SR and LPS; the inferior division supplies IR, IO, MR, and the presynaptic parasympathetics (Fig. 3.5).
• Presynaptic parasympathetic fibers terminate in the ciliary ganglion near the apex of the extraocular muscle cone. Postganglionic fibers form six to 10 short ciliary nerves that travel with nasociliary nerve (of CN V1) forward between the choroid and sclera to reach the ciliary body and iris. These control sphincter pupillae muscle to cause pupillary constriction and ciliary muscles to cause lens accommodation (Fig. 3.5).
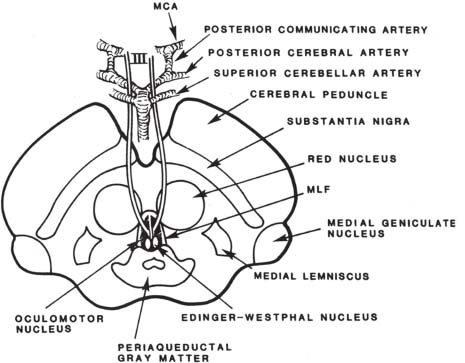
Fig. 3.1 Cross-section of midbrain at the level of the superior colliculus demonstrating oculomotor nucleus, Edinger-Westphal nucleus, and course of CN III (see text). (MCA, middle cerebral artery.) (MLF, medial longitudinal fasciculus.) (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.] St. Louis, MO: Mosby, 1995. Reprinted with permission.)
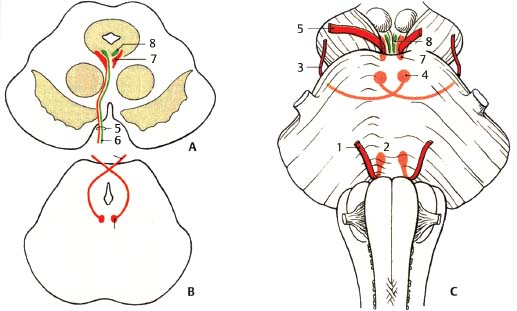
Fig. 3.2 Comparison of nuclear regions and exits of oculomotor, trochlear, and abducens nerves. (A) Midbrain at the level of the superior colliculus. ( B) Midbrain at the level of the inferior colliculus. (C) Ventral view of brainstem. (1, abducens nerve; 2, abducens nucleus; 3, trochlear nerve; 4, trochlear nucleus; 5, oculomotor nerve; 6, visceromotor (parasympathetic) fibers; 7, oculomotor nucleus; 8, Edinger-Westphal nucleus.)
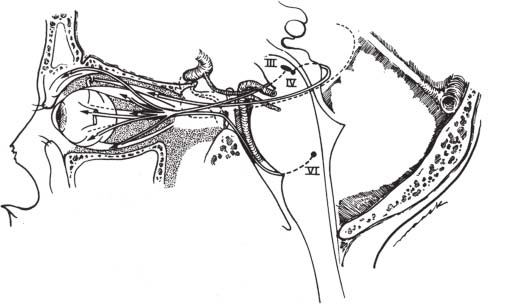
Fig. 3.3 Comparison of origins and courses of oculomotor, trochlear, and abducens nerves. The oculomotor and trochlear nerves originate in the midbrain, whereas the abducens nerve originates in the lower pons. All three nerves ultimately exit the cranial base into the eye via the superior orbital fissure (see text for details). (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.] St. Louis, MO: Mosby, 1995. Reprinted with permission.)
Oculomotor Nerve: Normal Images (Figs. 3.6, 3.7, 3.8, 3.9, 3.10, 3.11, 3.12, 3.13)
Oculomotor Nerve Lesions
• Oculomotor palsies may be categorized as isolated (only CN III affected) or complex (multiple cranial neuropathies including CN III).
• Most common causes of isolated CN III palsies in adult are ischemia, mass effect due to aneurysm, uncal herniation, and neoplasm.
• Complex palsies affecting CN III are usually due to brainstem lesions affecting other tracts/nerves or meningeal or skull base pathologies that affect adjacent CNs (e.g., cavernous sinus, SOF, orbital apex).
• CN III palsy may be complete or incomplete, with the pupil variably involved or spared.
• In complete oculomotor palsy, the eye is depressed and abducted (“down-and-out”) due to unopposed action of the SO and LR muscles.
• Pupillomotor (parasympathetic) fibers are situated peripherally in the nerve, so ischemia is thought to preferentially affect somatic motor fibers in the interior of the nerve (supplied by the vasa nervorum), whereas compressive lesions preferentially (or first) affect the more superficial pupillomotor fibers. If parasympathetic fibers are involved, the pupil is “fixed and dilated” (mydriatic and unresponsive to light due to dysfunction of pupillary sphincter) and there is paralysis of lens accommodation (ciliary muscle dysfunction).
• Imaging evaluation of patients with nuclear CN III lesions should include magnetic resonance imaging (MRI) (brainstem to orbit) and MR angiography (MRA) (to evaluate the posterior circulation).
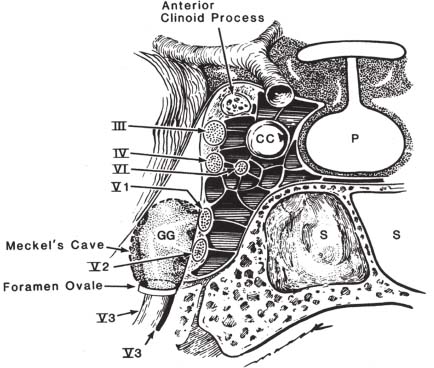
Fig. 3.4 Coronal view through the cavernous sinus demonstrates CN III, IV, VI, and V1 and V2 in the lateral wall of the cavernous sinus and CN VI within the cavernous sinus adjacent to the cavernous portion of the internal carotid artery. Note that CN V3 does not enter the cavernous sinus but rather leaves the cranial base through the foramen ovale. (CC, cavernous segment of internal carotid artery; GG, Gasserian ganglion; P, pituitary gland; S, sphenoid sinus.) (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.] St. Louis, MO: Mosby, 1995. Reprinted with permission.)
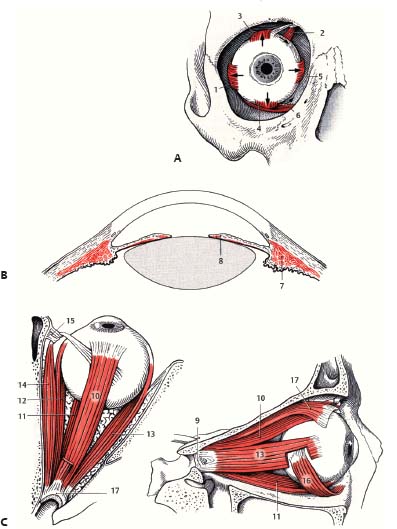
Fig. 3.5 Schematic of extraocular and intraocular muscles. (A) Anterior view. (1, LR muscle; 2, SO muscle; 3, SR muscle; 4, IR muscle; 5, MR muscle; 6, IO muscle.) (B) Intraocular muscles. (7, ciliary muscle; 8, sphincter pupillae muscle.) (C) Superior (left) and lateral (right) views. (9, common annular tendon [annulus of Zinn]; 10, SR muscle; 11, IR muscle; 12, MR muscle; 13, LR muscle; 14, SO muscle; 15, trochlea; 16, IO muscle; 17, LPS muscle.)
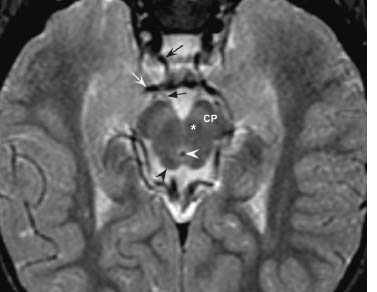
Fig. 3.6 Axial fast spin echo T2 at the level of the midbrain demonstrates normal cerebral peduncles (CP) and red nuclei (asterisk) and superior colliculi (black arrowhead). The oculomotor nuclei are located just anterior to the cerebral aqueduct of Sylvius (white arrowhead). Note both CN III exiting anteriorly into the interpeduncular fossa. The right CN III (black straight arrow) passes adjacent to the right PCA (white curved arrow) and PCommA (black concave arrow).
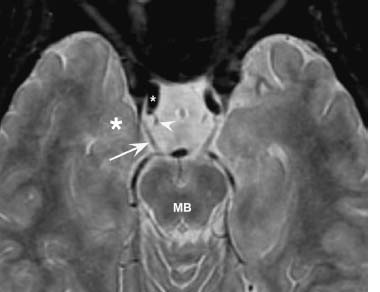
Fig. 3.7 Axial fast spin echo T2-weighted image demonstrates both CN III (arrow on right CN III) exiting the midbrain (MB) and traversing the subarachnoid space to the posterior margin of the cavernous sinus. CN III passes lateral to the PCommA (arrowhead) as it exits the right supraclinoid carotid artery (white asterisk) and medial to the adjacent uncus of the temporal lobe (black asterisk).

Fig. 3.8 Axial image from a CT cisternogram at the level of the midbrain shows the cisternal segment of CN III (concave arrow) traversing the subarachnoid space. In addition, there is subarachnoid contrast within the optic sheath (straight arrow) along the left optic nerve. Note the (B) basilar artery and (C) carotid canal.
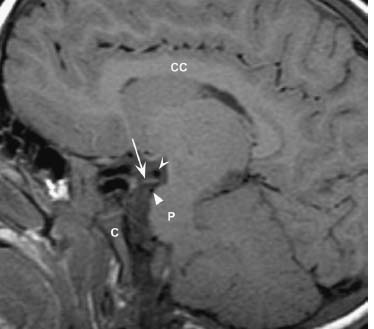
Fig. 3.9 Sagittal T1-weighted image demonstrates CN III (arrow) passing between the PCA (concave arrowhead) and SCA (straight arrowhead) as it exits the midbrain. Note the pons (P), clivus (C) and corpus callosum (CC) on this midsagittal image.
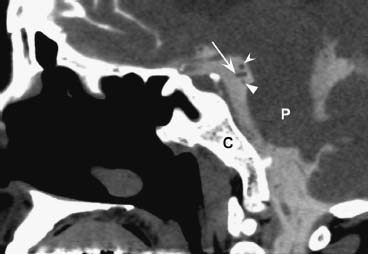
Fig. 3.10 Reconstructed sagittal image from a CT cisternogram shows CN III (arrow) passing between the PCA (concave arrowhead) and SCA (straight arrowhead) nicely ouT1ined by contrast within the subarachoid space. Note the pons (P) and clivus (C).
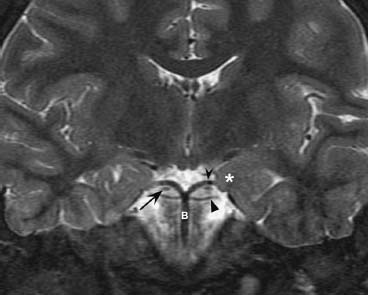
Fig. 3.11 Coronal fast spin echo T2-weighted image demonstrates CN III (arrow) passing between the PCA (concave arrowhead) and SCA (straight arrowhead), distal branches of the basilar artery (B). Note the close relationship of the uncus (asterisk) to CN III.

Fig. 3.12 Axial CT image of the orbits with soft tissue window shows a normal superior orbital fissure (arrow). Note the thin mural calcifications along the cavernous segment of the internal carotid artery (arrowhead). Note the normal MR and LR muscles, and optic nerve-sheath complex (ON). Normal aeration is seen within the sphenoid sinus (S) and ethmoid air cells (E).
Types
Brainstem Lesions (Nucleus or Fascicular Segment of Nerve)
• Congenital CN III palsies are rare but make up 20 to 43% of oculomotor palsies in children (secondary to maldevelopment, birth trauma, or intrauterine insult).
• Ischemia.
• Neoplasm.
• Infectious/inflammatory.
• Demyelinating disease.
• A pure nuclear lesion is rare but characteristically results in unilateral oculomotor palsy with weakness of the ipsilateral and contralateral SR and LPS (with bilateral incomplete ptosis due to bilateral innervation of the SR and LPS).
• Nuclear CN III lesion associated with ataxia, nystagmus, and altered mental status should prompt consideration of Wernicke encephalopathy (thiamine deficiency with neuronal loss and gliosis in ocular motor nuclei, usually with bilateral ophthalmoparesis).
• Specific named midbrain syndromes:
1. Weber syndrome. Ventral midbrain lesion affecting CN III (ipsilateral oculomotor palsy) and cerebral peduncle (contralateral hemiparesis/hemiplegia).
2. Claude syndrome. Lesion of midbrain tegmentum affecting CN III (ipsilateral oculomotor palsy), RN (contralateral tremor), and SCP (ipsilateral ataxia).
3. Benedikt syndrome. Lesion of midbrain tegmentum affecting CN III (ipsilateral oculomotor palsy), RN (contralateral tremor), SCP (ipsilateral ataxia), and the cerebral peduncle (contralateral hemiparesis/hemiplegia) .
4. Nothnagel syndrome. Lesion of midbrain tectum affecting CN III and SCP, causing unilateral or bilateral oculomotor palsy, gaze paralysis, and ipsilateral ataxia.

Fig. 3.13 Coronal postcontrast fat-saturated T1-weighted image shows the normal orbital anatomy. Note the normal enhancement of the extraocular muscles including the SR/LPS (levator palpebrae superioris) complex, MR, LR, IR, and SO. Enhancement of the right superior ophthalmic vein (SOV, arrow) is seen just inferior to the SR muscle. The normal optic nerve-sheath complex (ON) does not significanT1y enhance.
Lesions in the Subarachnoid Space (Cisternal Segment of Nerve)
• Ischemia. Isolated oculomotor palsy with pupillary sparing is usually indicative of ischemic oculomotor palsy (caused by diabetes, hypertension, atherosclerosis). Diabetic third nerve palsy is usually painful, develops over a few hours, and has a good prognosis for recovery. Imaging is not indicated in the clinical setting of a classic diabetic oculomotor palsy.
• Compression by aneurysm (see Table 3.1). Usually due to PCommA aneurysm. Extrinsic compression preferentially affects outer pupillomotor (parasympathetic) fibers early, resulting in a fixed and dilated (mydriatic) pupil.
• Uncal herniation. As with aneurysmal compression, compression of CN III by the uncus leads to an ipsilateral fixed and dilated pupil.
• Compression by tumor (typically schwannoma or meningioma).
• Leptomeningeal spread of tumor.
• Demyelinating disease (Miller-Fisher variant of Guillain-Barré syndrome includes ophthalmoplegia, ataxia, and areflexia).
• Inflammation/meningitis with secondary neuritis.
• Ophthalmoplegic migraine.
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree