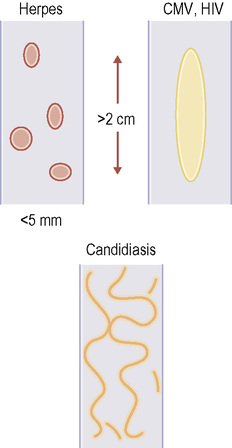
• Protrusion of part of the stomach through the diaphragmatic oesophageal opening • Schatski or B ring: a ring of mucosal tissue at the lower border of the phrenic ampulla marking the junction between the squamous and columnar epithelium (the ‘Z line’) • The ‘A’ ring or inferior oesophageal sphincter: about 2-4cm proximal to the B ring is a thicker ring produced by active muscular contraction • The Schatski ring is always associated with a small sliding hiatus hernia • The Schatski ring is usually no more than 2–3 mm in thickness • If the B ring is incomplete, part of it can sometimes be demonstrated as the incisural notch (which is inevitably seen on the greater curve aspect of the stomach) • GORD follows lower oesophageal sphincter dysfunction • Reflux: this may be demonstrated but alone is of questionable significance – minor amounts can occur in the normal population • Reflux oesophagitis: this can demonstrate mucosal oedema, erosive disease or frank ulceration • Long-term sequelae: stricture formation (typically a short stricture above a hiatus hernia with smooth tapered margins) • Oesophageal inflammation (± subsequent smooth benign stricture formation) can be caused by the following: • Candidiasis: initially there is dysmotility and atony of the oesophagus • HSV: vesicles in the upper and mid-oesophagus appear as sessile filling defects • CMV/HIV: presents with giant oesophageal ulcers • Drugs: potassium chloride causes deep ulceration leading to stricture formation • Radiation: > 20 Gy results in a transient oesophagitis with aperistalsis or tertiary contractions • Crohn’s disease: this can present with aphthoid ulcers or frank ulceration • Nasogastric tube: this renders the lower oesophageal sphincter incompetent, resulting in a reflux oesophagitis and a long tapered stricture within the lower oesophagus • Caustic ingestion: this can lead to mucosal necrosis with ulceration and mucosal sloughing • The excretory ducts of the oesophageal deep mucous glands dilate and fill with barium • Fistulation may occur between these pseudodiverticula • It is associated with oesophagitis (usually due to reflux) • Papilloma: these are usually small (2–5mm) • Leiomyoma: these are usually found within the lower 1/3 of the oesophagus • Neurofibroma/lipoma: these may be difficult to distinguish from a leiomyoma and are extremely rare • Fibrovascular polyp: these are usually found within the proximal oesophagus • Malignant tumours arising from the oesophageal mucosa or submucosa – It begins as a submucosal lesion (usually in the distal 1/3 of the oesophagus) resulting in a smooth luminal narrowing with an intact overlying mucosa – Secondary involvement by contiguous spread from adjacent nodal disease is more common but rarely results in dysphagia
Oesophagus
HIATUS HERNIA AND REFLUX
HIATUS HERNIA
DEFINITION
 Sliding hernia (the commonest type): the gastro-oesophageal junction (GOJ) slides proximally through the diaphragmatic hiatus to assume an intrathoracic position
Sliding hernia (the commonest type): the gastro-oesophageal junction (GOJ) slides proximally through the diaphragmatic hiatus to assume an intrathoracic position  it is accompanied by reflux and oesophagitis
it is accompanied by reflux and oesophagitis
 Rolling hernia: the GOJ is in a normal position below the diaphragm – the proximal stomach (usually the fundus) herniates through the hiatus
Rolling hernia: the GOJ is in a normal position below the diaphragm – the proximal stomach (usually the fundus) herniates through the hiatus  this is more prone to incarceration and obstruction, and it may undergo torsion, resulting in strangulation, infarction or perforation
this is more prone to incarceration and obstruction, and it may undergo torsion, resulting in strangulation, infarction or perforation
PEARLS
 it can be congenital or secondary to gastro-oesophageal reflux (with associated inflammation and fibrosis)
it can be congenital or secondary to gastro-oesophageal reflux (with associated inflammation and fibrosis)
 despite being mucosal it can be symptomatic (requiring dilatation)
despite being mucosal it can be symptomatic (requiring dilatation)
GASTRO-OESOPHAGEAL REFLUX DISEASE (GORD)
DEFINITION
 this initially leads to reflux (with minor irritation and inflammation) but can then proceed to ulceration, fibrosis and stricture formation
this initially leads to reflux (with minor irritation and inflammation) but can then proceed to ulceration, fibrosis and stricture formation  it may also be associated with a hiatus hernia
it may also be associated with a hiatus hernia
RADIOLOGICAL FEATURES
Barium swallow
 gross reflux (up to the level of the aortic knuckle or above and not cleared by a stripping wave passing down the oesophagus) is likely to be symptomatic
gross reflux (up to the level of the aortic knuckle or above and not cleared by a stripping wave passing down the oesophagus) is likely to be symptomatic
 Associated features: a wide gastro-oesophageal junction (> ⅔ of the maximally distended thoracic oesophagus)
Associated features: a wide gastro-oesophageal junction (> ⅔ of the maximally distended thoracic oesophagus)  an inflammatory gastro-oesophageal polyp (seen as a single linear polyp straddling the GOJ)
an inflammatory gastro-oesophageal polyp (seen as a single linear polyp straddling the GOJ)
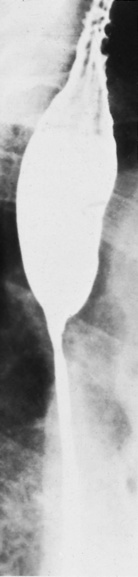
 initially the collapsed oesophagus shows thickened longitudinal folds (>3mm)
initially the collapsed oesophagus shows thickened longitudinal folds (>3mm)  multiple fine ulcers give the mucosa a punctate or granular appearance
multiple fine ulcers give the mucosa a punctate or granular appearance  larger discrete punched-out ulcers can develop
larger discrete punched-out ulcers can develop  ulceration is most pronounced immediately above the GOJ and local circular muscle spasm may produce transverse folds
ulceration is most pronounced immediately above the GOJ and local circular muscle spasm may produce transverse folds  scarring produces permanent folds that radiate from the ulcer margins
scarring produces permanent folds that radiate from the ulcer margins
 the development of Barrett’s oesophagus (in 10% of cases)
the development of Barrett’s oesophagus (in 10% of cases)
OESOPHAGITIS AND BENIGN STRICTURES
OESOPHAGITIS AND BENIGN STRICTURES
DEFINITION
 Infection: especially in the immunocompromised patient Candida albicans
Infection: especially in the immunocompromised patient Candida albicans  herpes simplex virus (HSV)
herpes simplex virus (HSV)  cytomegalovirus (CMV)
cytomegalovirus (CMV)  human immunodeficiency virus (HIV)
human immunodeficiency virus (HIV)  tuberculosis
tuberculosis
 Drugs: potassium chloride tablets
Drugs: potassium chloride tablets  tetracycline
tetracycline  clindamycin
clindamycin  doxycycline
doxycycline  NSAIDs
NSAIDs
 Radiation: this is often self-limiting
Radiation: this is often self-limiting
 Crohn’s disease: this is very rare and usually accompanied by extensive GI disease elsewhere
Crohn’s disease: this is very rare and usually accompanied by extensive GI disease elsewhere
 Iatrogenic: following prolonged placement of a nasogastric tube (NGT)
Iatrogenic: following prolonged placement of a nasogastric tube (NGT)
RADIOLOGICAL FEATURES
Barium swallow
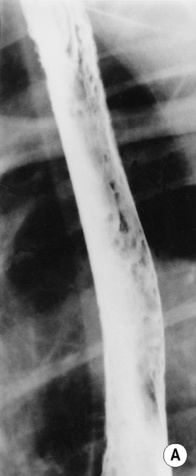
 eventually classic plaque-like filling defects with ulceration and pseudomembrane formation are seen (there are also irregular and thickened mucosal folds)
eventually classic plaque-like filling defects with ulceration and pseudomembrane formation are seen (there are also irregular and thickened mucosal folds)  occasionally pseudo-ulcerations may appear as aphthous ulcers
occasionally pseudo-ulcerations may appear as aphthous ulcers
 when they burst they leave punched-out superficial ulcers on a background of normal mucosa
when they burst they leave punched-out superficial ulcers on a background of normal mucosa  in advanced disease there can be diffuse ulceration
in advanced disease there can be diffuse ulceration
 NSAIDs can cause contact oesophagitis
NSAIDs can cause contact oesophagitis
 >45 Gy results in obliterative endarteritis after 6 months with severe oesophagitis and smooth strictures – deep ulcers can also form (which may fistulate to the trachea)
>45 Gy results in obliterative endarteritis after 6 months with severe oesophagitis and smooth strictures – deep ulcers can also form (which may fistulate to the trachea)
 this may occur only 48 h post placement
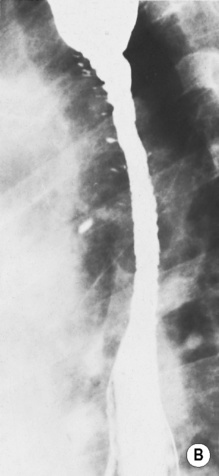
this may occur only 48 h post placement  the strictures are often long and extensive
the strictures are often long and extensive
 the oesophagus may perforate within the 1st 2 weeks or result in fistulation to the pleural cavity or pericaridium
the oesophagus may perforate within the 1st 2 weeks or result in fistulation to the pleural cavity or pericaridium  it heals with fibrosis and stricture formation
it heals with fibrosis and stricture formation  strictures occur at the normal sites of oesophageal compression (e.g. at the level of the aorta, left main bronchus or diaphragmatic hiatus)
strictures occur at the normal sites of oesophageal compression (e.g. at the level of the aorta, left main bronchus or diaphragmatic hiatus)
PEARLS
Intramural pseudodiverticulosis
 they are seen on barium studies as multiple, flask-shaped mucosal outpouchings
they are seen on barium studies as multiple, flask-shaped mucosal outpouchings  this disease is usually diffuse, but may be localized if it is associated with peptic stricture formation or an oesophageal carcinoma
this disease is usually diffuse, but may be localized if it is associated with peptic stricture formation or an oesophageal carcinoma
 intramural abscesses may develop which can rarely perforate through the oesophageal wall
intramural abscesses may develop which can rarely perforate through the oesophageal wall  long tapered strictures may arise
long tapered strictures may arise
 other underlying disorders include diabetes, candidiasis and alcoholism
other underlying disorders include diabetes, candidiasis and alcoholism
BENIGN AND MALIGNANT OESOPHAGEAL TUMOURS
BENIGN TUMOURS
DEFINITION
RADIOLOGICAL FEATURES
Barium swallow
 larger papillomas may trap barium within the interlacing fronds that cover their surface
larger papillomas may trap barium within the interlacing fronds that cover their surface
 they appear as a smooth wide-based filling defect covered by an intact mucosa
they appear as a smooth wide-based filling defect covered by an intact mucosa  they may calcify and can be multiple
they may calcify and can be multiple
 they are pedunculated (the stalk forms due to repeated passage of food with peristalsis)
they are pedunculated (the stalk forms due to repeated passage of food with peristalsis)  they may expand the oesophageal lumen but rarely cause significant barium hold-up (due to their very pliable nature)
they may expand the oesophageal lumen but rarely cause significant barium hold-up (due to their very pliable nature)
MALIGNANT TUMOURS
DEFINITION
 Oesophageal carcinoma: the commonest malignant tumour (see separate section)
Oesophageal carcinoma: the commonest malignant tumour (see separate section)
 Leiomyosarcoma (1%): these arise from the smooth muscle within the oesophageal wall – therefore they are found only within the distal oesophagus (striated muscle is found within the proximal 1/3 of the oesophagus)
Leiomyosarcoma (1%): these arise from the smooth muscle within the oesophageal wall – therefore they are found only within the distal oesophagus (striated muscle is found within the proximal 1/3 of the oesophagus)  they can grow to an extraordinary size before symptoms present due to their failure to cause obstruction
they can grow to an extraordinary size before symptoms present due to their failure to cause obstruction  they are relatively indolent and metastasize late
they are relatively indolent and metastasize late
 Melanoma (1%): these are rare tumours (melanoblasts are uncommon within the oesophagus)
Melanoma (1%): these are rare tumours (melanoblasts are uncommon within the oesophagus)  they metastasize early with a very poor prognosis
they metastasize early with a very poor prognosis
 Lymphoma (1%): oesophageal involvement is very rare
Lymphoma (1%): oesophageal involvement is very rare  it is usually of the non-Hodgkin’s type and is usually associated with lymphomatous disease elsewhere
it is usually of the non-Hodgkin’s type and is usually associated with lymphomatous disease elsewhere
 later ulceration can develop
later ulceration can develop
 Spindle cell carcinoma: a rare tumour containing both carcinomatous and spindle cell elements
Spindle cell carcinoma: a rare tumour containing both carcinomatous and spindle cell elements
 Metastases: these are usually due to direct extension from tumours within the thoracic cavity (notably carcinoma of the bronchus)
Metastases: these are usually due to direct extension from tumours within the thoracic cavity (notably carcinoma of the bronchus)  involved nodes may also infiltrate the oesophagus causing displacement and occasionally fistula formation between the oesophageal lumen and the adjacent bronchus
involved nodes may also infiltrate the oesophagus causing displacement and occasionally fistula formation between the oesophageal lumen and the adjacent bronchus  carcinoma of the pancreas (particularly the tail) may involve the distal oesophagus or gastro-oesophageal junction
carcinoma of the pancreas (particularly the tail) may involve the distal oesophagus or gastro-oesophageal junction


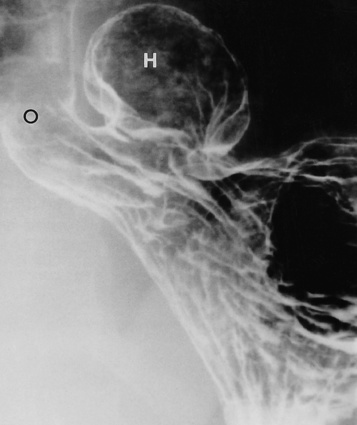
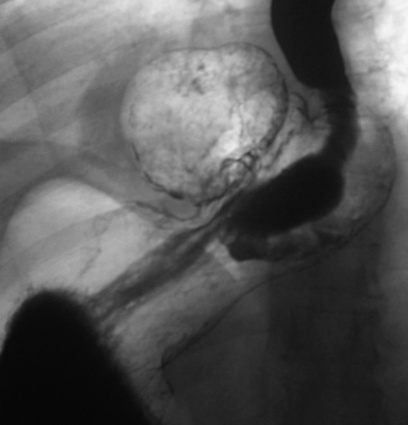
 symptoms are more commonly seen with a sliding hernia
symptoms are more commonly seen with a sliding hernia the major long-term complications are peptic oesophagitis (± stricture formation or Barrett’s oesophagus)
the major long-term complications are peptic oesophagitis (± stricture formation or Barrett’s oesophagus)

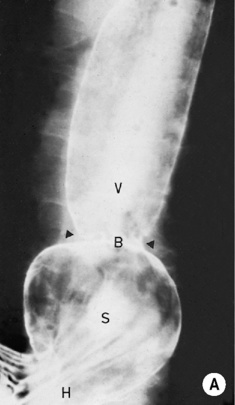
 S = stomach forming the hernia
S = stomach forming the hernia  B = B ring, the gastro-oesophageal junction
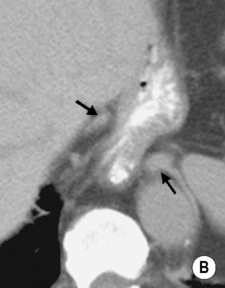
B = B ring, the gastro-oesophageal junction  V = vestibule. The A ring is not visible. (B) CT scan showing the crura of the diaphragm (arrows) separated by 28mm (normal is <15mm). The fundus of the stomach is seen herniating through the diaphragmatic hiatus.†
V = vestibule. The A ring is not visible. (B) CT scan showing the crura of the diaphragm (arrows) separated by 28mm (normal is <15mm). The fundus of the stomach is seen herniating through the diaphragmatic hiatus.†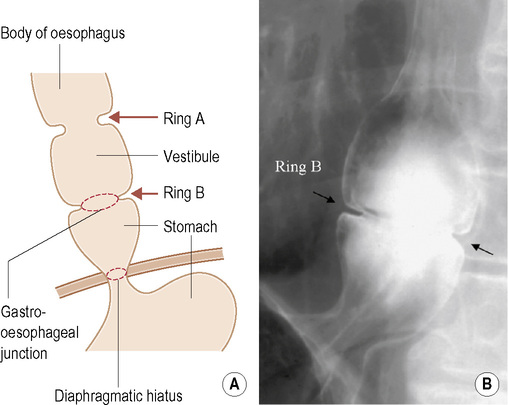


 dysphagia
dysphagia  haematemesis
haematemesis the oesophagus may be involved (leading to stricture formation)
the oesophagus may be involved (leading to stricture formation) the upper oesophageal mucosa may be involved with ulcers, webs and stricture formation
the upper oesophageal mucosa may be involved with ulcers, webs and stricture formation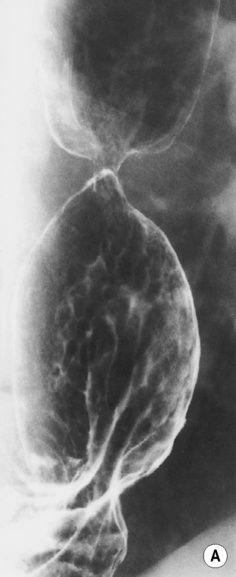






 neurofibroma
neurofibroma  lipoma
lipoma  fibrovascular polyp
fibrovascular polyp
 its aetiology is unclear (but possibly age related)
its aetiology is unclear (but possibly age related)  it demonstrates no malignant potential
it demonstrates no malignant potential
 there can be a large exophytic component which may be seen on a CXR as a mediastinal mass
there can be a large exophytic component which may be seen on a CXR as a mediastinal mass





