Fig. 1
Left femoral pseudoaneurysm
Catheterization of Cerebral Vessels
Dissection
Arterial dissection can occur during catheterization of the cerebral vessels with the guiding catheter.
Patients with atherosclerotic plaques are prone to this.
Patients with tortuous vessels where distal access is needed are also at a higher risk.
To reduce the risk, a soft-tip guiding catheter should be used.
For distal access (e.g., to position the tip of the guiding catheter in the petrous segment of the internal carotid artery (ICA)):
The guide catheter can be pushed over the microcatheter/guidewire combination rather than over a Terumo wire.
Another technique is to push the guide catheter over a softer (125 cm) vertebral or SIM catheter or catheters such as the Chaperon.
Management
Small dissection does not usually require any further management.
If dissection is large enough to cause distal flow compromise, the dissected segment can be crossed with a microcatheter/guidewire combination.
Stenting the affected segment should then be considered.
Precaution with anticoagulants has to be considered if the patient subsequently needs treatment of ruptured aneurysm (Fig. 2a–d).
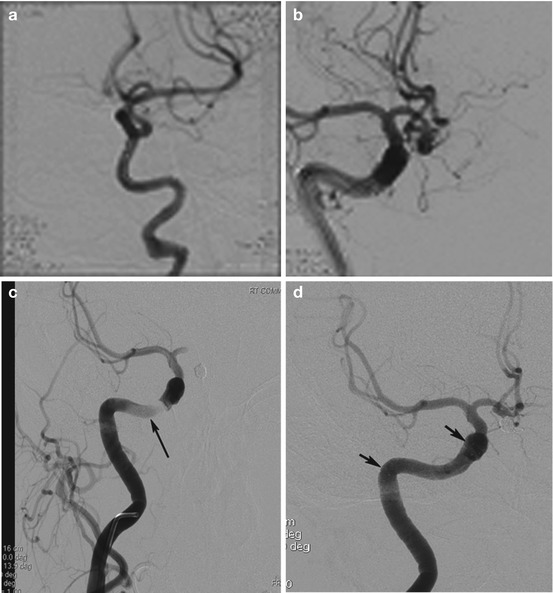
Fig. 2
(a) Left ICA injection demonstrates small dissections which occurred during microcatheterization in patient with Ehlers-Danlos connective tissue disorder. (b) Guide catheter placed in the petrous segment of ICA in order to get stability for balloon-assisted coiling of ACOM aneurysm. (c) Angiogram post-coiling shows dissection caused by guide catheter. (d) Angiogram in same patient shows post-stenting
Thromboembolic Complications
These types of complications can occur while positioning the guide catheter or performing precoiling cerebral angiogram.
Thrombus can build up within the guide catheter if adequate heparinized saline flush is not maintained. Always check the pressure and flow in the heparinized saline infusion bags to maintain a steady flow.
Embolic thrombus can be a problem when passing guide catheters past atherosclerotic lesions at the ICA origin. In this scenario:
(a)
Place a self-expanding or balloon expandable stent at the stenosis.
(b)
Position the guide catheter in the common carotid artery (CCA), preferably with additional support with a long sheath (i.e., Destination or Arrow long sheath).
Treat the thrombus with IV aspirin and full-dose heparin once the aneurysm is secure. Occasionally, mechanical thrombectomy may be required in large clots.
Small embolic thrombus can cause distal vessel occlusion during angiogram. This is extremely rare if proper technique and care is used during catheter angiogram (Fig. 3a, b).
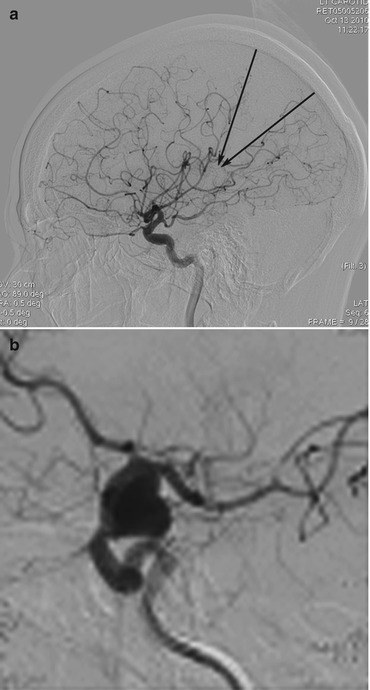
Fig. 3
(a) Demonstrates parietal hypoperfusion during precoiling angiogram. (b) Small embolus in M2 branch during placement of guide catheter and angiogram
Iatrogenic Vasospasm
Induced mainly while catheterizing the intracranial vessels using guide catheter. To reduce the risk:
Use soft-tip guide catheters like the Neuron with Terumo wire if vasospasm is expected.
If distal access with the guide catheter is required, advance the catheter over microcatheter/guidewire combination rather than Terumo wire (Fig. 4a–c).

Fig. 4
(a) Demonstrates extreme vasospasm caused while trying to achieve distal guide catheter access in tortuous vessel. (b) Severe vasospasm of ICA post-catheterization with a guide catheter (different case). (c) Increasing the dose of nimodipine and 30 min wait restored normal vessel architecture, and the aneurysm was coiled
Aneurysm Coiling
Most feared complications are intraprocedural iatrogenic aneurysm rupture and thromboembolic complications.
Studies report 2–5 % intraprocedural rupture rate while coiling aneurysms post subarachnoid hemorrhage.
Large series have reported procedural thromboembolic complications leading to mortality or morbidity of around 6 % in ruptured aneurysm and 1–3 % in treatment of unruptured aneurysm.
Incidence of silent thromboembolic events is higher and is in the region of 15–30 %.
Can be detected while performing diffusion-weighted magnetic resonance imaging (MRI).