Functions
• Special afferent (SA) for vision.
Retina
• Divided into four quadrants by horizontal and vertical meridians (superior/inferior and nasal/temporal)
• Phototransduction occurs by photoreceptors (rods and cones), which contain light-sensitive pigments. Rods are absent from macula and optic disc (blind spot). Cones (color vision, three types: R, G, B) (~7 million cones) are tightly packed in the macula (100,000), which is at the posterior pole 4 mm lateral to optic disc and accounts for most visual acuity.
• Flow of information in retina is from photoreceptors to bipolar cells to ganglion cells. Other cell types in retina include horizontal cells (neurons), amacrine cells (neurons) and Müller cells (glial cells) that are thought to modulate the signal (e.g., surround inhibition).
• The axons of retinal ganglion cells form the optic nerve at the optic disc. Note that, like the olfactory nerve and unlike other cranial nerves, the optic nerve is really a CNS tract.
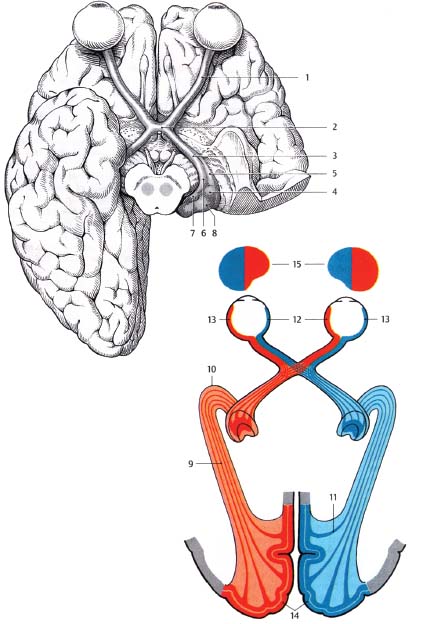
Fig. 2.1 Visual pathway and adjacent structures. 1, optic nerve; 2, optic chiasm; 3, optic tract; 4, lateral geniculate nucleus [LGN]; 5, lateral root of optic tract [to LGN]; 6, medial root of optic tract [to superior colliculus and pretectum]; 7, medial geniculate nucleus [part of auditory pathway]; 8, pulvinar [thalamic nucleus]; 9, optic radiation; 10, temporal genu; 11, occipital genu; 12, nasal retina [fibers cross at chiasm]; 13, temporal retina [fibers remain ipsilateral]; 14, striate cortex [primary visual cortex]; 15, visual fields.
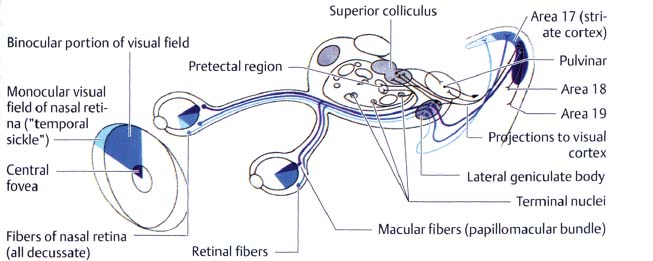
Fig. 2.2 Slightly more detailed view of visual pathway demonstrates the retinocollicular and retinopretectal tracts as well as the retinogeniculate pathway. Not shown is the retinohypothalamic tract (to suprachiasmatic nucleus (SCN) of hypothalamus) (see text).
Optic Nerves and Optic Chiasm
• Optic nerve (Figs. 2.3, 2.4) contains 1 million fibers (comparison: cochlear nerve 50,000 fibers). Macular fibers are on the temporal side of the optic disc and the adjacent optic nerve and move to the central part of the nerve as the papillomacular bundle for most of the distal pathway. The larger nonmacular fibers are on the periphery.
• Optic nerve is 50 mm long and has four portions:
1. Intraocular (1 mm) (also called optic nerve head). Axons become myelinated.
2. Intraorbital (25 mm). From back of globe to optic canal.
3. Intracanalicular (9 mm). Traverses optic canal with ophthalmic artery and sympathetic plexus.
4. Intracranial (4 to 16 mm). Lies superior to the internal carotid artery (ICA) as ICA exits cavernous sinus and gives off ophthalmic artery. The sphenoid sinus is inferomedial, whereas the anterior cerebral artery (ACA) (A1 segment), gyrus rectus, olfactory tract, and anterior perforated substance lie superior.
• See Table 2.1 for a summary of vascular supply of the visual pathway.
• The two optic nerves converge at the optic chiasm where the nasal axons from the nasal retina decussate and the axons from the temporal retina remain ipsilateral.
• Positioning of the optic chiasm: The prefixed chiasm (9%) lies over the tuberculum sellae, 80% over the sella turcica (L., “Turkish saddle”); the postfixed chiasm (11%) lies over the dorsum sellae.
• The optic chiasm (Fig. 2.5) is located below the suprachiasmatic recess of the third ventricle, lamina terminalis, and anterior commissure; the pituitary stalk is immediately posterior.
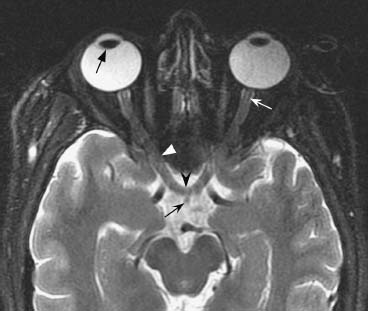
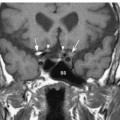
Fig. 2.3 Axial T2-weighted image demonstrates high signal intensity fluid within the ocular globes. The right lens is well seen (black straight arrow). Normal optic nerve (white concave arrow) is seen surrounded by perioptic fluid in the optic sheath. More posteriorly, the nerves traverse the optic canal (white arrowhead) to meet at the optic chiasm (black arrowhead) in the midline. Note that the pituitary stalk (small black curved arrow) is located just posterior to the optic chiasm.
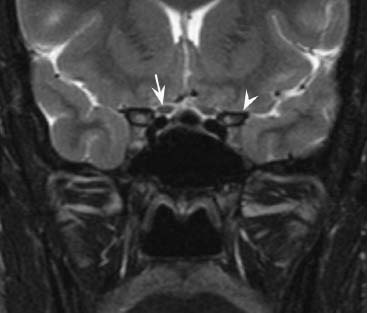
Fig. 2.4 Coronal T2-weighted image shows normal optic nerves entering the optic canals. The right optic nerve is indicated (arrow). The nerves lie medial to the anterior clinoid processes (arrowhead) and just above the flow void of the internal carotid artery.
Abbreviations: ACA, anterior cerebral artery; ACommA, anterior communicating artery; CN, cranial nerve; CRA, central retinal artery; ICA, internal carotid artery; MCA, middle cerebral artery; PCA, posterior cerebral artery; PCommA, posterior communicating artery.
Retinal Targets
• There are four brain regions that directly receive visual information from the retina (Fig. 2.2):
1. Retinogeniculate pathway. Primary pathway for visual information; to lateral geniculate nucleus (LGN) of thalamus for conscious vision
2. Retinopretectal tract. Retina to pretectal area of midbrain for pupillary light reflex (see Appendix B)
3. Retinocollicular tract. To superior colliculus for eye movement reflexes (e.g., conjugate eye movements in response to head movements)
4. Retinohypothalamic tract. To bilateral suprachiasmatic nuclei (SCN) of hypothalamus for circadian rhythms and neuroendocrine function
Optic Tracts
• Extend from chiasm posterolaterally around hypothalamus, around cerebral peduncles to lateral geniculate nuclei
• Vascular relationships: Posterior communicating artery (PCommA) located inferior to optic tracts in suprasellar cistern, posterior cerebral artery (PCA) and basal vein of Rosenthal apposed to optic tracts in perimesencephalic cistern
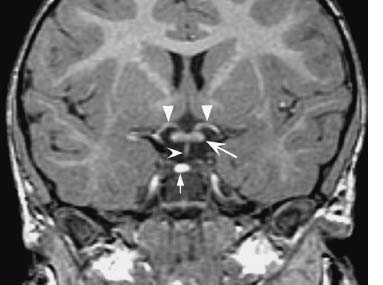
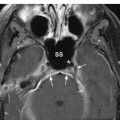
Fig. 2.5 Coronal thin-section spoiled gradient echo (SPGR) image demonstrates a normal optic chiasm (concave arrow) beneath the anterior cerebral arteries (straight arrowheads) and above the pituitary stalk (concave arrowhead). Note the posterior pituitary “bright spot” (small straight arrow).
Lateral Geniculate Nucleus (Fig. 2.6)
• In the inferolateral thalamus lateral to the upper midbrain
• Contains tertiary neurons that form the optic radiations to the primary visual cortex surrounding the calcarine fissure
• Contains six laminae (I–VI). I, IV, VI from contralateral eye; II, III, V from ipsilateral eye
Optic Radiations (Geniculocalcarine Tracts) (Figs. 2.1, 2.2, 2.7)
• Formed by axons of LGN neurons projecting to calcarine cortex of occipital lobe.
• Sweep posteriorly around lateral and posterior portion of lateral ventricles.
• Parietal lobe optic radiations start in the medial LGN and take a direct, nonlooping course over the top of the inferior horn of the lateral ventricle and then travel posteriorly through the parietal white matter to the superior calcarine cortex (subserve inferior visual fields).
• Temporal lobe optic radiations start in the lateral LGN, course anteriorly toward the temporal pole before turning posteriorly in a sharp loop (Meyer’s loop) to course around the lateral wall of the inferior horn of the lateral ventricle then posteriorly to the inferior calcarine cortex (subserve superior visual fields). They account for contralateral superior quadrantanopsia following temporal lobectomy.
• Ventral optic radiations are closely associated with the posterior limb of the internal capsule.
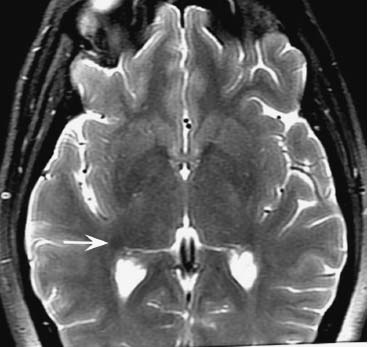
Fig. 2.6 Axial T2-weighted image at the level of the third ventricle shows the lateral geniculate nucleus (arrow) as a faint, relatively low signal focus at the lateral margin of the posterior thalamus.
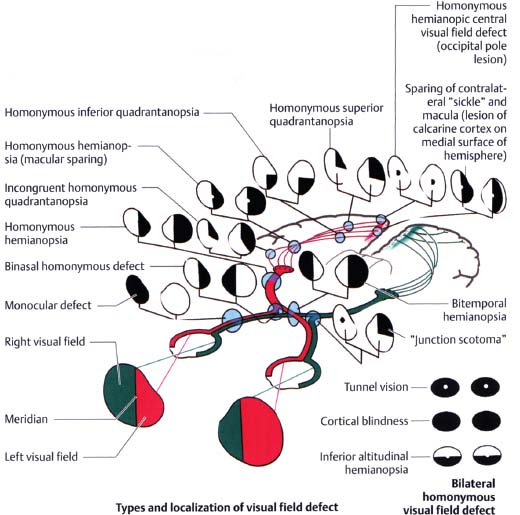
Fig. 2.7 Sites of lesions in the visual pathway and their associated visual field deficits.
Visual Cortex and Visual Association Areas
• Primary visual cortex (area 17) in walls and floor of calcarine sulcus in medial occipital lobe.
• Geniculocalcarine afferent input to layer IV of six-layered neocortex.
• On cross-section, white matter stria (stria of Gennari, thick white matter band in layer IV) can be seen with naked eye (thus striate cortex).
• Macula projects to posterior one third of the calcarine cortex (occipital pole). Macula represented posteriorly, peripheral retina anteriorly (fovea at occipital pole), upper field inferior, right field on left.
• Primary visual cortex projects to secondary visual areas (peristriate cortex) V2 (area 18) and V3 (area 19) in adjacent occipital lobe cortex.
Optic Nerve: Normal Images (Figs. 2.3, 2.4, 2.5, 2.6)
Optic Pathway Lesions
• The most common visual disorders are pathologies of the globe and vary by age:
 Children: nearsightedness (myopia)
Children: nearsightedness (myopia)
 Adults: farsightedness (hyperopia)
Adults: farsightedness (hyperopia)
 Elderly: cataracts, glaucoma, retinal hemorrhages/detachment, macular degeneration
Elderly: cataracts, glaucoma, retinal hemorrhages/detachment, macular degeneration
• Episodic visual loss in early adulthood is usually caused by migraines and in late adulthood by transient ischemic attacks (TIAs).
Nonneurologic Causes of Visual Loss (related to abnormal light transmission through the eye)
• Cornea. Scarring, deposits, infection, ulceration, and trauma.
• Anterior chamber. Hemorrhage, infection, open-angle glaucoma (90% of glaucoma cases; drainage pathway is partially open, there is gradual visual loss, and the eye looks normal), closed-angle glaucoma (increased intraocular pressure, red and painful eye).
• Lens. Cataracts, traumatic dislocation, diabetes (sorbitol accumulation), Wilson disease, Down syndrome, and spinocerebellar ataxia.
• Vitreous humor. Hemorrhage from retinal or ciliary vessels due to trauma, arteriovenous malformation (AVM), or aneurysm (Terson syndrome, usually from ruptured anterior communicating artery (ACommA) aneurysm). “Floaters” are opacities in the vitreous humor. A sudden increase in floaters with a flash of light occurs with retinal detachment.
• Uveitis. Inflammation of the uvea (consists of iris, ciliary body, and choroid layer); accounts for ~10 to 15% of all cases of total blindness in the United States and has many causes, including inflammatory disease (e.g., systemic lupus erythematosis, sarcoidosis, rheumatoid arthritis, ulcerative colitis, Behcet disease), infection (e.g., cytomegalovirus [CMV], tuberculosis [TB], Toxoplasma, Histoplasma), and autoimmune disease (e.g., multiple sclerosis [MS]).
Types
Retinal Pathologies
• Diabetic retinopathy. Associated with microaneurysms, arteriovenous (A-V) nicking, “dot and blot” hemorrhages, exudates, and neovascularization. Leading cause of blindness in the United States.
• Hypertensive retinopathy. Associated with arteriolar narrowing, A-V nicking, hemorrhage and “cotton wool” exudates, and copper- or silver-wiring.
• Senile macular degeneration. Leading cause of blindness in the elderly. The hereditary form may also occur in children and young adults. Usually spares the peripheral retina.
• Retinal detachment. Fluid collects between the sensory retina and the retinal pigment epithelium.
• Amaurosis fugax. Sudden onset of transient monocular blindness usually from a small fibrin embolus.
• Retinitis pigmentosa. Begins in childhood and adolescence, male preponderance. Autosomal recessive (AR) or autosomal dominant (AD) inheritance on chromosome 3. Degeneration of all retinal layers (neuroepithelium and pigment epithelium) with foveal sparing. Starts with impairment of twilight vision (nyctalopia) progressing to blindness.
 Usher syndrome. AR, retinitis pigmentosa with congenital hearing loss as well.
Usher syndrome. AR, retinitis pigmentosa with congenital hearing loss as well.
 Lawrence-Moon-Biedl syndrome. AR, retinitis pigmentosa, obesity, congenital heart disease, developmental delay, polydactyly, renal disease, diabetes insipidus.
Lawrence-Moon-Biedl syndrome. AR, retinitis pigmentosa, obesity, congenital heart disease, developmental delay, polydactyly, renal disease, diabetes insipidus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree