Oral Cavity, Oropharynx
The oral cavity includes the anterior two-thirds of the tongue, the lingual and buccal mucosa, the sublingual space (which houses the sublingual gland, and the neurovascular pedicle of the tongue), the deep lobe of the submandibular gland, and the mylohyoid muscle (the sling that forms the floor of the mouth). Extrinsic muscles of the tongue include the genioglossus, hyoglossus, styloglossus, and palatoglossus muscles while intrinsic muscles include vertical, horizontal, and oblique fibers. All muscles are innervated by CN XII. The anterior digastric muscles lie outside of the oral cavity proper, below the mylohyoid muscle and above the platysma muscle. The anterior digastric and mylohyoid muscles are innervated by the mylohyoid nerve, a distal branch of CN V3. The oropharynx includes the posterior one-third of tongue (the tongue base), the palatine tonsils, lymphoid tissue at base of tongue (lingual tonsils), the soft palate, and the oropharyngeal mucosa, held in place by the constrictor muscles.
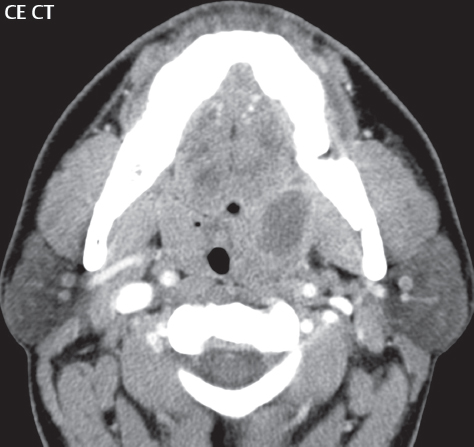
Infections in this area usually involve the mandible (due to dental caries), salivary glands (with an obstructive calculus), or tonsils ( Fig. 2.86 ). Extensive infection involving the sublingual and submandibular spaces, typically bilateral (Ludwig angina), is a serious, potentially life-threatening infection, usually occurring in adults ( Fig. 2.87 ). It is the result of dental caries and, if untreated, can lead to airway obstruction.

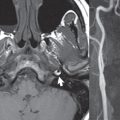
More than 90% of malignant tumors involving the oral cavity and oropharynx are squamous cell carcinomas. These are associated with alcohol and tobacco use, and some are associated with the human papilloma virus (HPV). Other much less common malignant lesions include non-Hodgkin lymphoma and minor salivary gland tumors. Half of all minor salivary gland tumors in this region are malignant. In regard to the tongue, squamous cell carcinoma easily spreads along the intrinsic muscles. In image interpretation, it is important to assess spread in relation to the midline. Without midline extension, hemiglossectomy is a surgical option ( Fig. 2.88 ). The most common oral cavity tumor is squamous carcinoma of the lower lip. Other common sites include the tongue, floor of the mouth, retromolar trigone, and hard palate.

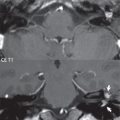
Within the oropharynx, tonsil carcinoma is the most common squamous cell carcinoma, with a strong HPV association ( Fig. 2.89 ). In this location in particular, there is a very high incidence of nodal metastases at presentation (60–75%, usually level II). Regardless of specific location, bilateral lymph node involvement at presentation is common. Squamous cell carcinoma is well visualized on MR in the oral cavity and oropharynx, with slight high signal intensity on T2-weighted scans and enhancement on postcontrast scans, which should be both performed using fat saturation.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree