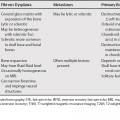
30 Lymphoproliferative disorders can involve the orbit, and can be suggested by certain imaging characteristics. It can be difficult to separate benign (orbital pseudotumor, reactive lymphoid hyperplasia) from malignant (lymphoma) lymphoproliferative disorders based on imaging features, as they share many features in common (Table 30.1).
Orbital Lymphoproliferative and Inflammatory Disorders
Orbital Pseudotumor
| Lymphoma | Pseudotumor | |
|---|---|---|
| Sites of Involvement | Commonly, the lacrimal gland, extraconal space (anterior and superior), extraocular muscles | Can involve any or all orbital structures Lacrimal gland most common site; extraocular muscles common |
| CT | Non-contrast: Isodense to slightly hyperdense to muscle/brain Mild to moderate diffuse enhancement | Soft tissue mass with no specific density values Variable, but often moderate contrast enhancement |
| MRI | T1WI: Isointense to mildly hyperintense to muscle T2WI: Isointense to hyperintense to muscle T1 +C Moderate to marked enhancement | T1WI: Hypointense to muscle T2WI: Isointense; may be hypointense if fibrotic T1 +C Moderate diffuse enhancement |
| Margins | May be well-defined mass, but may be infiltrative where lesion abuts orbital fat | Depends on site of involvement – well defined if involving lacrimal gland or muscles, or poorly defined and infiltrative |
| Bony Changes | Lesions tend to mold to bone and orbital structures without destruction; destruction generally only in aggressive lesions | Bony remodeling and foraminal expansion |
| Atypical Features | Infiltrative appearance to fat May appear inflammatory | May extend through foramen, especially to cavernous sinus or temporal fossa |