OROPHARYNX: INFECTIOUS AND NONINFECTIOUS INFLAMMATORY CONDITIONS
KEY POINTS
- Imaging, especially computed tomography, is often useful in the management of acute pyogenic oropharyngeal infections and in the identification of potentially lethal although uncommon complications.
- Computed tomography can provide a safe and rapid assessment of the airway in a patient who is stable and under the control of the treating physician for airway management decisions.
- Imaging in noninfectious inflammatory diseases is generally nonspecific for diagnostic purposes.
- Atypical clinical and imaging features of oropharyngeal pathology should raise the possibility of an inflammatory process.
- Relatively few people undergo imaging for the latter group of noninfectious inflammatory diseases.
Most acute infections of the oropharynx present an obvious clinical picture, so imaging is reserved for establishing the extent rather than the cause of the disease, such as whether pyogenic tonsillitis is associated with an abscess that is tonsillar or peritonsillar. After physical examination, it may be difficult to decide whether an area of oropharyngeal swelling is inflammatory or infectious as opposed to neoplastic under less clear clinical circumstances. For instance, in a low-grade inflammatory process, this distinction might remain unclear even after biopsy, so watchful waiting might sometimes become the default strategy with imaging surveillance as an aid (Fig. 192.1).
Much inflammatory swelling in the oropharynx will have a nonspecific imaging appearance when considered independent of the clinical setting. Taken with clinical setting, the findings are often specific enough to confirm the suspected clinical etiology. Computed tomography (CT) and occasionally magnetic resonance imaging (MRI) are then used for their primary function of mapping the extent of the most commonly pyogenic, infectious inflammatory process.
For simplicity, this chapter is divided in two sections: one dealing with infections and one with the much less common noninfectious inflammatory conditions.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
Occasionally, a developmental lesion such as a thyroglossal duct cyst (Chapter 170) or branchial apparatus cyst (Chapter 153) will become infected and present as a primary oropharyngeal infection (Fig. 192.2). The embryology of those types of anomalies is discussed in chapters just shown in parentheses and elsewhere.
Applied Anatomy
The critical anatomic knowledge necessary for the evaluation of inflammatory oropharyngeal processes is summarized here. The detailed anatomy of this region and the adjacent nasopharynx, oral cavity, larynx and hypopharynx, and related deep tissue spaces are reviewed in chapters indicated in parentheses.
- Regional anatomy of the oropharynx including the tonsillar pillars, palatine tonsils, tongue base, glossotonsillar sulci, and valleculae (including the normal variation of lymphoid tissue lining the mucosal surfaces) and that of the parapharyngeal space (Chapters 142 and 190)
- Related regional anatomy of the structures above and below the oropharynx, including the nasopharynx (Chapter 184), oral cavity (Chapter 196, mainly the anatomy of the floor of the mouth), larynx (Chapter 196, tongue base relationship to the pre-epiglottic space), and hypopharynx
- Bony anatomy: Hard palate, pterygoid plates, and mandible (Chapter 196)
- Neurovascular bundles: lingual and hypoglossal nerve and greater and lesser palatine and posterior superior alveolar neurovascular bundles
IMAGING APPROACH
Techniques and Relevant Aspects
Computed Tomography and Magnetic Resonance Imaging
Inflammatory conditions of the oropharynx are studied with CT and MRI in essentially the same manner as benign and malignant oropharyngeal tumors, except the entire neck may not be included. The specifics and relative value of using these studies in this anatomic region are reviewed in Chapter 190. Problem-driven protocols for CT and MRI are presented in Appendixes A and B. In general, CT is more definitive than magnetic resonance (MR) in the evaluation of the oropharyngeal and deep space, primarily pyogenic, infectious processes.
Other
Ultrasound has only a limited role in the evaluation of these conditions. Intraoral ultrasound has been reported as useful for detecting possible peritonsillar abscess.1 Radionuclide studies used to evaluate infectious disease (Chapter 5) have little or no diagnostic use in the evaluation of oropharyngeal conditions but may be used occasionally to monitor the response to therapy of a chronic infection. The normal anatomic variations in this region seen on fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) studies and its lack of specificity significantly limit any potential diagnostic value of that study.
Plain film soft tissue views of the neck, while often done, are typically not definitive or cost effective and may add delay to the diagnostic process except when done to confirm possible croup or epiglottis in children (Chapter 204).
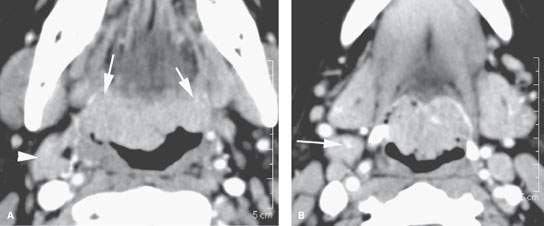
FIGURE 192.1. Contrast-enhanced computed tomography study (A, B) of a patient presenting with dysphagia and otalgia. The study showed marked hypertrophy of the lingual tonsillar tissue along the tongue base and reactive adenopathy at level 2 (arrowheads). There was some concern over early infiltrative behavior of this tissue at its margins with the tongue base musculature (arrows), so biopsies were done. The biopsies returned chronic inflammation. The cause for the chronic inflammation was never established. The patient was followed, and both the symptoms and tonsillar hypertrophy eventually improved.
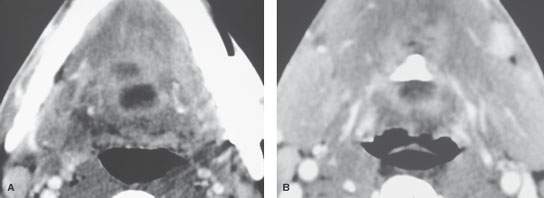
FIGURE 192.2. Contrast-enhanced computed tomography study of an infected thyroglossal duct cyst. The abscess extends into the tongue base (A) and along the tract from the suprahyoid neck at the level of the hyoid bone in (B).
Pros and Cons
Infections of the oropharynx may involve or arise in bone, predominantly the mandible; therefore, CT becomes immediately preferable to MR. The patients are often very uncomfortable, and MRI will be motion degraded. A definitive CT study providing all necessary information can be accomplished in about 5 to 10 minutes, making it a more sensible first choice. MRI can be used for problem solving, such as in chronic conditions where it might help to choose the most productive biopsy site when it is difficult to differentiate tumor from a chronic inflammatory process.
SPECIFIC DISEASE/CONDITION
Acute and Subacute Pyogenic Bacterial Infections, Viral Infections, and Chronic Infections
Etiology
The vast majority of infections of the oropharynx that come to imaging are acute or subacute pyogenic bacterial infections, being mainly due to pharyngeal infections complicated by abscess formation and a few due to extension of dental infections (Figs. 192.3–192.11). Fungal infection occurs predominantly in the immune-compromised population and typically does not come to imaging except for an occasional case of candidiasis that might be initially mistaken clinically for a complicated bacterial infection in a critically ill patient. Some sporadic and relatively rare infections due to fungi may present in the oropharynx, usually from a site of origin in the jaw (Fig. 192.12). Tuberculosis (TB) may involve the Waldeyer ring (Fig. 192.13). Syphilis may cause an atrophic glossitis, and a mucosal gumma may mimic tumor until it is biopsied.
Viral infections are usually not so severe that they clinically mimic pyogenic infection enough to trigger imaging with CT or MRI. Epstein-Barr virus infection, including posttransplant lymphoproliferative disease (PTLD) (Fig. 192.14), may mimic lymphoma, and the related adenopathy may trigger imaging. Human immunodeficiency virus (HIV) infection can manifest in the lymphoid tissue of the Waldeyer ring.
Prevalence and Epidemiology
Pyogenic bacterial infections occur sporadically, primarily in the pediatric and young adult populations. In the older age group, diabetes—especially when poorly controlled—is a predisposing factor. HIV and other immune-compromising conditions will predispose to fungal infections and TB.
Clinical Presentation
In infants, acute and subacute bacterial infections will present with fever and poor feeding and possibly lymphadenopathy. In older children and adults, these infections will cause fever, usually a very intense sore throat and altered voice, and lymphadenopathy. In the more indolent infections and in immune-compromised patients, there may be little if any fever, and local symptoms such as odynophagia may be less prevalent.
Pathophysiology and Patterns of Disease
The morphology of infectious and inflammatory disease and related bone and vascular complications are discussed in detail in Chapters 13 through 16.
Manifestations and Findings
Plain Film and Fluoroscopy
Plain films may show pharyngeal swelling, especially along the posterior pharyngeal wall, or extraluminal gas. Such study may rarely reveal an otherwise unsuspected causative radiodense foreign body. In general, this is a superfluous first step in a patient who requires a definitive imaging evaluation.
Computed Tomography and Magnetic Resonance Imaging
The details of how these inflammatory conditions spread and tend to generally appear on CECT are discussed in Chapters 13 through 16.
Contrast-enhanced CT and contrast-enhanced MR will show a pyogenic process that has a typical cellulitis pattern and may show an associated contained or spreading abscess (Chapter 13). Both modalities should almost always be able to differentiate “drainable” from “nondrainable” infectious processes.1,2 These findings will often have spread into the deep planes around the oropharynx and adjacent regions. Bone erosion (Chapter 14) and vascular complications (Chapter 15) may be present. The most well known vascular complication is Lemierre syndrome in acute pyogenic tonsillitis. Cortical bone erosion may not be as evident on MR as compared to CT. More indolent infections may show a similar morphology but are less likely to show frank abscess cavities (Chapter 16). Most of these infections will enhance more than muscle. They replace fat and may spread along paths of least resistance. It is important to understand differentiating features of the following conditions in this category.
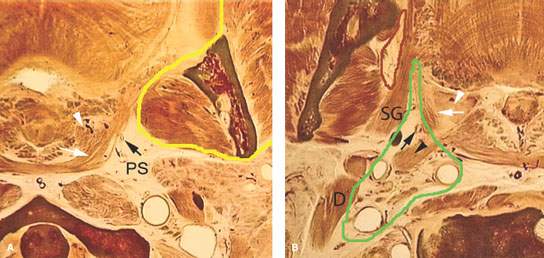

FIGURE 192.3. A series of anatomic line diagrams to emphasize the regional anatomic basis for the potential spread patterns of tonsillar and peritonsillar infections, including abscess, and some of their complications. A: At the level of the palatine tonsil atrophic tonsillar tissue (arrowhead) lines the airway inside the fibers of the constrictor musculature at that level. A potential space is present between that tonsillar tissue and muscle bundles (white arrow). It is within that space that pus can spread outside the tonsillar crypts and around the tonsil pseudocapsule within the peritonsillar “space.” Small vessels (black arrow) are seen within the parapharyngeal space (PS). It is likely along these vessels that thrombophlebitis can spread to the jugular vein, causing Lemierre syndrome. The yellow outlines the relatively tight fascia around the masticator space that considerably restricts tonsillar-related abscesses from spreading to the masticator space. Masticator space abscesses are typically of dental and not tonsillar origin. B: A section somewhat inferior to that seen in (A). The green line outlines the retrostyloid parapharyngeal space. The red line outlines the prestyloid parapharyngeal space. The atrophic tonsillar tissue is shown by the white arrow, and the potential space between that tonsillar tissue and the pharyngeal musculature is shown by the white arrow. It is in the space shown by the white arrow that peritonsillar abscesses spread. The black arrowhead indicates the juxtaposition of the styloid musculature with the pharyngeal wall that makes it possible for infections to travel along the styloid musculature in a matter similar to tumors to reach the retrostyloid parapharyngeal space. The black arrows show small vessels that might penetrate the muscular wall, which are another potential route for spread of pus into the parapharyngeal space and thrombophlebitis to reach the jugular vein. C: Anatomic section at the tongue base showing retention cysts or atrophic lingual tonsillar tissue at its interface with the minor salivary glands lining the tongue base (white arrows). At this level, pus generally spreads within the lingual tonsillar tissue, with there being no plane such as that around the palatine tonsils present except at the interface of the tongue base and tonsillar tissue. The arrowheads show the vessels within the parapharyngeal space that might transmit purulent material to the jugular vein (black arrow) and result in Lemierre syndrome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree