OROPHARYNX: MALIGNANT TUMORS
KEY POINTS
- Computed tomography and magnetic resonance imaging are critical to the medical decision-making process in oropharyngeal cancer due to their ability to show the deep soft tissue extent of the primary, bone involvement, perineural spread, carotid fixation, and related retropharyngeal and cervical adenopathy.
- Computed tomography and magnetic resonance imaging, and to some extent, fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET), are useful to detect mucosally nonapparent primary oropharyngeal carcinoma.
- Computed tomography and magnetic resonance imaging are useful in excluding oropharyngeal cancer as a cause of symptoms that might be referable to such a cancer and in patients with parapharyngeal-origin masses that might raise the concern of a submucosal cancer.
- Both anatomic imaging with computed tomography and magnetic resonance imaging and physiologic imaging with FDG-PET might be useful in posttreatment surveillance and detection of recurrence at its most curable state.
- A detailed knowledge of this regional anatomy, including the normal variations of the lymphoid tissue lining this part of the pharynx, is necessary to accomplish these goals.
Ninety-five percent of oropharyngeal malignant tumors are squamous cell carcinoma (SCCA). Some are nonkeratinizing, and this variety of SCCA is occasionally still referred to as lymphoepithelioma. Malignant lymphomas (Chapter 27), minor salivary gland epithelial carcinomas (Chapter 22), plasmacytoma (Chapter 28), and sarcomas (Chapter 35) are all unusual, but they account for the majority of the small group of other cancers that may arise primarily in the oropharynx.
Patients with malignant tumors of the oropharynx usually present with obviously mucosal masses. They also present with submucosal masses or pain (usually throat pain and/or otalgia), trismus, or other functional complaints related to swallowing or mastication without a visible mass (Figs. 195.1 and 195.2). They may also present with cervical adenopathy of uncertain etiology (Figs. 195.1 and 195.2). All of these circumstances make oropharyngeal cancer an important consideration in many, predominantly adult, patients who seek care for such common head and neck region symptoms, signs, and physical findings.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The critical anatomic knowledge necessary for the evaluation of oropharyngeal malignancies is summarized here. The detailed anatomy of this region and the related nasopharynx, oral cavity, larynx and hypopharynx, and related deep tissue spaces, as well as regional lymphatic pathways, are reviewed in chapters indicated below in parentheses. A detailed working knowledge of all of this anatomy is necessary to evaluate images of patients with known or suspected oropharyngeal cancer if the evaluation of the image is expected to contribute measurably to medical decisions.
The general anatomic knowledge necessary to evaluate cancer of the oropharynx includes the following:
- Regional anatomy of the oropharynx, including the tonsillar pillars, palatine tonsils, tongue base, glossotonsillar sulci and valleculae (including the normal variation of lymphoid tissue lining the mucosal surfaces), and the parapharyngeal space (Chapters 142 and 190)
- Related regional anatomy of the structures above and below the oropharynx, including the nasopharynx (Chapter 184), oral cavity (Chapter 196, mainly the anatomy of the floor of the mouth and pterygomandibular raphe), larynx (Chapter 196, tongue base relationship to the pre-epiglottic space [PES]), and hypopharynx
- Bony anatomy, including the hard palate, pterygoid plates, and mandible (Chapter 196)
- Neurovascular bundles, including the lingual and hypoglossal nerves and greater and lesser palatine and posterior superior alveolar neurovascular bundles
- Retropharyngeal and cervical lymph node groups, particularly levels 2 through 5 (Chapter 149)
IMAGING APPROACH
Techniques and Relevant Aspects
General Examination Technique
For computed tomography (CT) acquisitions, section thickness should be 0.5 to 1.0 mm through the area of main interest so that reformations, when necessary, are of adequate spatial resolution. Intravenous contrast is always used except when CT is being done solely to look for bone erosion. Specific CT cancer protocols are presented in Appendix A. No special maneuvers are necessary.1
Magnetic resonance (MR) is done primarily in the axial plane. Others may be added for special circumstances, such as the sagittal plane for subtle spread to the PES or the coronal plane confirmation of spread to the nasopharynx and rarely the skull base.
Fat-suppressed imaging can lose critical information in the anterior oropharynx due to field distortion susceptibility artifacts generated by dental appliances (Chapters 1 and 3). Fat suppression should generally not be the sole T1-weighted postcontrast acquisition unless it can be confirmed that no such artifacts will occur. Specific MR cancer protocols are presented in Appendix B.
The neck should almost always be included when CT and magnetic resonance imaging (MRI) are performed. Imaging for distant metastases includes a chest roentgenogram. A chest CT to include the liver and a bone scan are obtained only if the patient has a clinical picture suggesting the presence of distant metastases. FDG-PET should be used with discernment with regard to its likelihood of having a significant contribution beyond accurate anatomic imaging to medical decision making in any individual case.
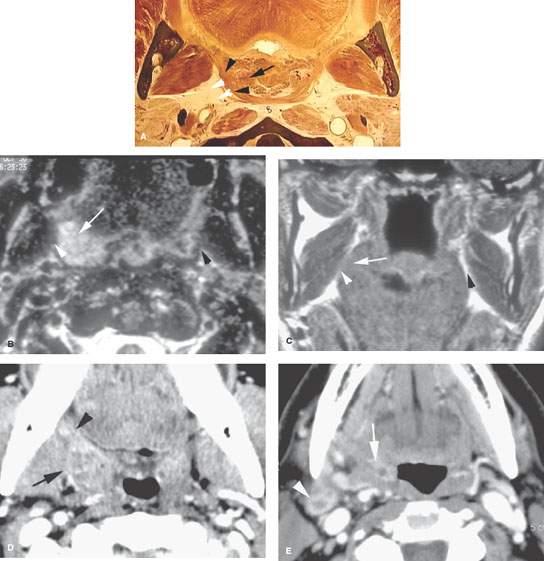
FIGURE 195.1. Two patients presenting with mucosally inapparent primary cancer of the palatine tonsil. A: Anatomic section to show the gross anatomic structures that must be understood in order to detect such submucosal cancers. The important relationship is that between the normal tonsillar tissue within the tonsillar fossa (arrow) and the surrounding constrictor muscle. B, C: Patient 1 magnetic resonance study. The patient presented with a level 2 enlarged lymph node and right-sided otalgia. Physical examination showed no definite primary tumor. The T2-weighted image in (B) shows a mass in the right tonsillar fossa (arrow) invading the constrictor muscle of the pharyngeal wall (arrowhead). The T1-weighted image in (C) shows the mass (arrow) obliterating the fat of the parapharyngeal space (arrowhead) compared to the normal opposite side. D, E: Patient 2 presenting with right-sided otalgia and painful swallowing. Contrast-enhanced computed tomography study in (D) shows enlargement of the right palatine tonsil and infiltration of the adjacent parapharyngeal space (arrows) and thickening of the anterior tonsillar pillar (arrowhead). In (E), there is continued extension into the right glossotonsillar sulcus (arrow). The metastatic level 2 lymph node on the right side was not palpable.
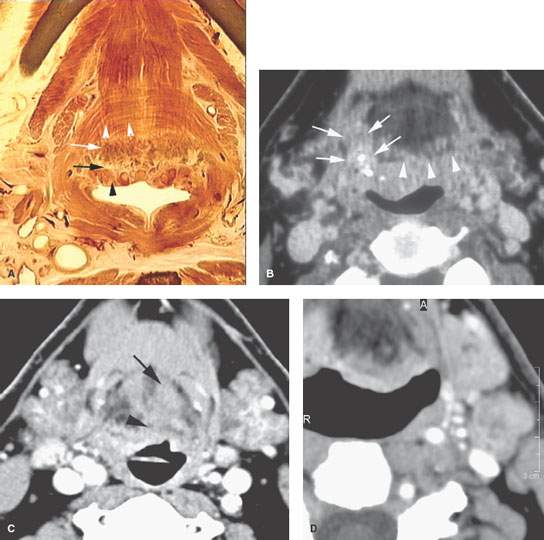
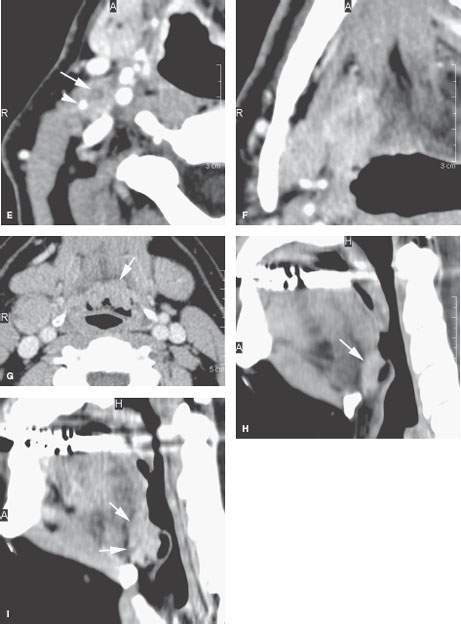
FIGURE 195.2. Four patients with mucosally inapparent cancer of the tongue base. A: Anatomic diagram showing important anatomic features contributing to an accurate diagnosis of such tumors. The lymphoid tissue at the tongue base (black arrowhead) may appear separate from the minor salivary tissue (white arrow) at the tongue base. These are normal layers of tissue that cannot be differentiated from superficial cancers. However, when tumor penetrates from those layers into the intrinsic musculature of the tongue base (white arrowheads), a diagnosis of an infiltrative process, most often cancer, can be made with relatively high degrees of confidence. B: Patient 1. Computed tomography (CT) study of a patient presenting with a right neck mass and otalgia. The arrowheads indicate an interface between what could be normal lingual tonsillar tissue and the other normal layers of lymphoid tissue and minor salivary glands at the tongue base as described in (A). However, the arrows show a penetrating mass beyond those normal anatomic limits due to squamous cell carcinoma (SCCA). C: Patient 2 presenting with otalgia on the left. No mucosal primary was identified. CT study with contrast shows an infiltrating mass at the left tongue base. D–F: Patient 3 presenting with bilateral cervical adenopathy in level 2, with those metastatic nodes (D) and (E) with focal defects likely due to SCCA deposits (arrows) and dense keratin debris or calcification (arrowhead) due to the very infiltrative tumor seen in (F). The aggressive nature of this primary tumor is indicated by its indistinct margins and its travel along the lingual neurovascular bundle (arrow), strongly suggesting perineural spread, which was confirmed in the specimen. G–I: Patient 4 presenting with a right level 2 neck mass visible on the contrast-enhanced CT image in (G). The primary tumor involved the vallecula and was mainly superficially spreading, although a zone of penetration into the tongue base (arrow) is present, with images seen in (H) and (I) confirming that penetration. Compare the interface between the tissue at the tongue base (arrow in H) to be more penetrating cancer that encroaches on the intrinsic tongue base and musculature and fat (arrows in I).
Pros and Cons
CT and MRI are used for the majority of imaging for oropharyngeal malignancies. Plain radiographs, orthopantomography, and occlusal views remain useful adjuncts for studying the teeth and mandible. Dental-related artifacts can seriously degrade both CT and sometimes MRI images through the oral tongue and mid oral cavity in general. The problem is generally worse on CT. The problem is accentuated on MRI when fat suppression is used (Chapter 3). MRI is very frequently significantly degraded by jaw and other motion. CT is the preferred primary study because it is better than MRI for evaluating the presence and extent of metastatic lymphadenopathy and bone detail and provides more consistently higher-quality studies than MRI, mainly related to motion artifacts that plague a significant number of MRI studies below the hard palate. MR is used adjunctively when necessary for medical decision making.
FDG-PET is used selectively and adjunctively when it may aid in medical decision making. Such imaging should only be used with discernment with regard to its likelihood of having a contribution to medical decision making in any individual case. It is not necessary in many cases since it will not influence therapeutic decisions or outcome (Chapter 5).
Ultrasound has no clearly indicated role in the evaluation of the primary site in oropharyngeal cancer. There is some adjunctive use in some practices for staging lymph nodes (Chapters 4 and 157).
Angiography has no primary role in known oropharyngeal cancer. It is used very rarely to assess flap complications. MR angiography and CT angiography are used to assess adequacy of vascular pedicles in planning free tissue transfer such as fibular bone and soft tissue pedicled grafts used in mandibular reconstructions.
Indications for Magnetic Resonance and Computed Tomography Study
Evaluation of Masses of Uncertain Etiology That Could be Due to Oropharyngeal Cancer: Cervical Node Metastases with a Possible Clinically Inapparent Primary and Referred Otalgia
Patients with malignant tumors of the oropharynx usually present with obviously mucosal masses. They occasionally present with submucosal masses or pain (usually otalgia), trismus, or other functional complaints related to swallowing or mastication without a visible mass (Figs. 195.1 and 195.2). They may also present with a cervical nodal mass, usually at level 2, of uncertain etiology. Such a nodal mass should never be considered a cancer arising in a branchial cleft cyst since this notion is an unfortunate concept held over from a time when it was less possible to find the responsible primary tumor.
CT or MRI is indicated for the evaluation of any submucosal oropharyngeal mass or neck mass of uncertain etiology. Such a submucosal mass may be a benign tumor arising from the parapharyngeal space, but it could be a malignancy arising submucosally or deeper. A neck mass might also be inconsequential, but it could be the first sign of a highly curable cancer.
The key element making CT and MR complementary to the clinical evaluation in these situations is their demonstration of the deep anatomy surrounding the oropharynx. Those deep planes and structures are generally symmetric. Loss of a deep fat space such as the parapharyngeal space or invasion of the tongue base and pharyngeal constrictor musculature is a reliable sign of an aggressive process such as, but not limited to, cancer (Chapters 21 and 23). Spread in these areas may not produce signs and symptoms or be detectable by physical examination. The symmetry of the deeper planes is highly reliable in the nasopharynx and as far inferiorly as the palatine tonsils (Chapter 184). However, below the tonsillar fossa, the pharyngeal wall is more tightly surrounded by musculature and the submandibular gland sometimes lessening the utility of parapharyngeal fat infiltration as an early imaging finding in cancer. This makes a diagnosis of deeply infiltrating disease more difficult.
In contrast, the mucosal surfaces of the oropharynx are highly variable, with there being marked variation from side to side and along the anterior and posterior walls bordering the lumen. The lymphoid tissue present throughout the oropharynx is responsible for most of this mucosal surface variation present on CT and MR images. These contour variations on the mucosal surfaces may be mistaken for tumor. They would more properly be ignored or at best used as clues to look for adjacent deep infiltration as a sign of aggressive pathology (Figs. 195.1 and 195.2). The mucosa is evaluated by physical examination. The only finding that can potentially distinguish lymphoid tissue and other benign mucosal findings from cancer is infiltration of the tongue base musculature, other muscles such as the relatively thin pharyngeal constrictors, and parapharyngeal space (Figs. 195.1 and 195.2). However, infections and rarely other benign inflammatory conditions (Chapter 192) such as amyloidosis (Fig. 192.15) can also infiltrate these structures deep to the mucosa and related lymphoid tissue.
Known Cancers
Early cancer or superficially spreading lesions of the oropharynx may be studied to evaluate the neck and exclude a deeply infiltrating component. Cancer with a clinical suspicion for deep infiltration should be studied for several purposes.
The specific observations to be made on CT and MRI in oropharyngeal cancer include the evaluation of the deep extent of primary tumors at all specific sites of origin relative to spread patterns summarized in the diagrams in Figure 195.3 and described in the subsequent Pathophysiology and Patterns of Disease section and in Appendix C and as follows:
- Submucosal spread confined to the visceral compartment that may extend in a clinically occult fashion to the nasopharynx and hypopharynx; also for spread across the midline, especially in tongue base cancer that may then threaten both lingual neurovascular bundles and spread to the PES (Figs. 195.4–195.12)
- To evaluate anterior spread along the lingual alveolar sulcus, within the floor of the mouth, and to the oral tongue that may not be anticipated by physical examination (Fig. 195.6)
- To determine the proximity of tumor to the lingual neurovascular bundle, especially when tumor breaches the midline to threaten both lingual neurovascular bundles (Fig. 195.7)
- Spread to and within the prestyloid parapharyngeal space that also may extend as high as the nasopharynx and central skull base and as low as the hypopharynx (Figs. 195.4 and 195.5)
- To detect spread along the styloid musculature to the hyoid bone and below involving the deep neck soft tissues (Fig. 195.8)
- Spread to the styloid musculature and retrostyloid parapharyngeal space that can result in carotid encasement and rarely lower cranial nerve involvement (Fig. 195.9)
- To detect spread out of the floor of the mouth along the lingual neurovascular bundle to involve the external carotid perhaps to the carotid bifurcation (Fig. 195.10)
- Spread to the infratemporal fossa, the masticator space, and deep neck (Fig. 195.11)
- To detect occasional remote perineural spread along the hypoglossal nerve, mandibular division of the trigeminal nerve, greater and lesser palatine nerves, and posterior superior alveolar nerves (Fig. 195.11)
- Bone involvement that is unusual in early primary lesions of the oropharynx, except for anterior tonsillar pillar cancer (Fig. 195.11)
- Evaluation of cervical and retropharyngeal nodes (Figs. 195.12 and 195.13)
Posttreatment Surveillance
Baseline anatomic imaging studies for planned surveillance are done about 3 to 4 months after treatment or earlier if risk of failure is high and a planned salvage strategy is in place. FDG-PET may also be used for posttreatment surveillance, but its accuracy is not acceptable earlier than 3 months following completion of radiotherapy or chemoradiation treatment plans (Figs. 5.5, 5.6, and 195.15).
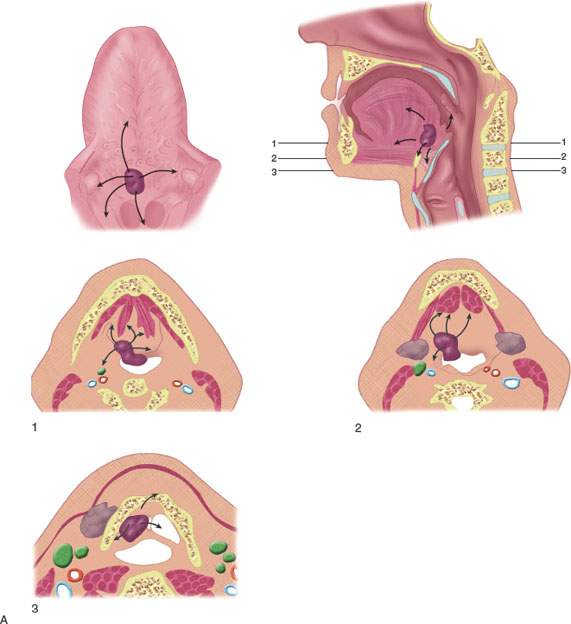
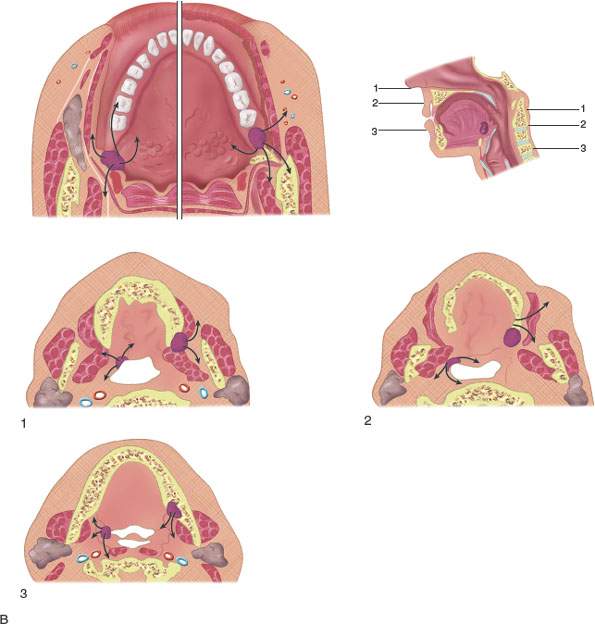
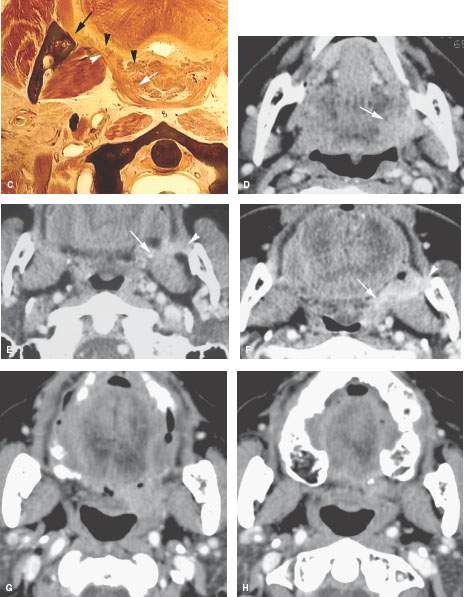
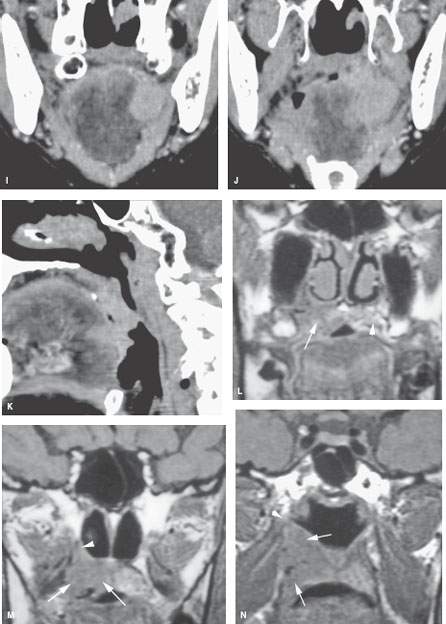
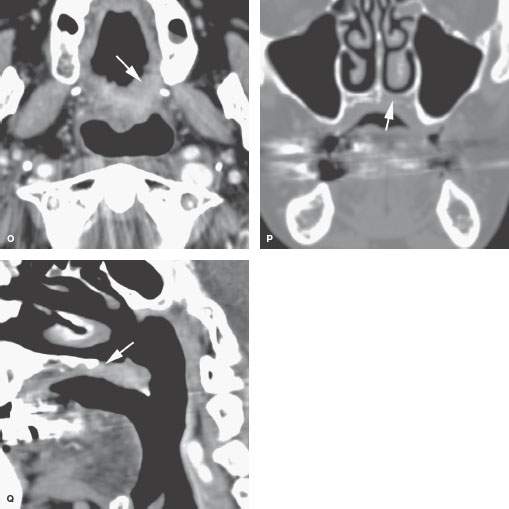
FIGURE 195.3. The patterns of oropharyngeal cancer extension shown by line diagrams. In this figure, the border zone and the junction of the oral cavity and oropharynx at the anterior tonsillar pillar is emphasized. A: Diagram of general spread patterns of tongue base cancer. B: Diagram of spread patterns of oropharyngeal cancer contrasted with those arising along the posterior alveolar ridge and in the retromolar trigone. Anterior tonsillar pillar cancers are, in their growth patterns, often akin to oral cavity cancers, producing the same tendency to be less curable by radiotherapy than oropharyngeal carcinoma. C: Anatomic section showing the important area of border zone relationships between the anterior aspect of the oropharynx and the posterior aspect of the oral cavity. This is reviewed in more detail in Chapters 190 and 196. The important anatomic structures include the relationship of the palatine tonsillar tissue (white arrow) to the anterior tonsillar pillar (white arrowhead) and the attachment of pharyngeal musculature along the pterygomandibular raphe (black arrow). This diagram also shows minor salivary glands located submucosal within the anterior tonsillar pillar and soft palate (black arrowheads) that explain the occasional non–squamous cell carcinoma arising in this location frequently beneath intact mucosa. D–F: Patient 1. Computed tomography (CT) study showing anterior tonsillar pillar carcinoma extending from the posterior oral tongue (arrow in D) to the anterior tonsillar pillar (arrow in E) and then to the pterygomandibular raphe (arrowheads in E and F). This is a typical spread pattern of a relatively limited anterior tonsillar pillar cancer that might be expected to behave more like an oral cavity cancer when considering treatment strategy. G–K: Patient 2. Contrast-enhanced CT study showing the primary tumor centered along the anterior tonsillar pillar (arrow in G) spreading to the junction of the tonsillar pillar and soft palate (arrow in H). In (J) and (K) are coronal and sagittal reformations, respectively, that show the tumor superior extent at the soft palate (arrows). This is an example of an anterior tonsillar pillar cancer behaving more as an oropharyngeal cancer than an oral cavity primary. L–N: Patient 3 had a magnetic resonance study showing the primary soft palate carcinoma (arrow) replacing the fat and glandular tissue within the soft palate tissue as seen on the opposite side (arrowhead). In (M), the tumor (arrows) extends into the inferior aspect of the greater palatine canal (arrowhead) but does not extend to the pterygopalatine fossa on other sections. In (N), the tumor can be seen growing along the levator muscle of the soft palate to just below the eustachian tube orifice (arrows). O–Q: Patient 4 (O) had a contrast-enhanced CT study showing a soft palate cancer that extends anteriorly to invade the hard palate (arrows), as confirmed in (P) and (Q).
Controversies
The justification for standard or “routine” use of FDG-PET in head and neck cancer remains unsubstantiated. The proper role of FDG-PET is just becoming tempered by an evidence base, although in practice its use is common, often with no benefit to the patient or the medical decision-making process (Figs. 5.2–5.9, 195.14, and 195.15). This assumes that a general survey for other cancers in this population that generally has considerable tobacco and alcohol mucosal exposure (lung and gastrointestinal included) is not the justification of the FDG-PET study; this sort of screening argument for its use is beyond the scope of this resource. FDG-PET should only be used with discernment with regard to its likelihood of contribution to medical decision making beyond that available from optimal anatomic data, perhaps augmented by perfusion data in the near future, in any individual case.
Some2–4 consider FDG-PET useful and potentially better than MRI and CT for finding a mucosally inapparent primary. These authors believe that such a benefit is marginal in light of the false-positive rate of FDG-PET in the Waldeyer ring lymphoid tissue (Fig. 5.3 and Chapter 5).
There are some practices wherein MRI is the preferred initial imaging tool for oropharyngeal cancer. This is not recommended by these authors.
There have been recent suggestions that perfusion imaging by CT or MRI can help select patients who are more suitable for chemoradiation protocols than radiotherapy alone. The theory is based on possibly greater angiogenesis in more aggressive tumors and/or relative radioresistance in low-perfusion tumors with possible lowered levels of tissue oxygenation.5–7 This remains a speculative but promising thesis.
There has also been some speculation that standard uptake values (SUVs) may be useful in a manner similar to perfusion data for treatment decision making.8,9 There is no reasonable accumulation of evidence to support this idea and variability of SUV calculations between institutions makes broad application of such theories problematic.
SPECIFIC DISEASE/CONDITION
Oropharyngeal Squamous and Other Carcinomas
Etiology
Carcinoma of the oropharynx typically arises at one site but may spread to others. Tobacco use is the main etiologic factor, with alcohol use acting as a synergistic factor.10 Human immunodeficiency virus infection may also be a risk factor associated with occurrence earlier in life. Papillomavirus is a clearly contributing etiologic agent in patients without the aforementioned risk factors.11 Other carcinomas are of predominantly glandular origin and are sporadic and not necessarily linked to known predisposing factors.
Prevalence and Epidemiology
Oropharyngeal carcinoma is typically a disease of those over 50 years of age and is more common in males. Ninety-five percent of oropharyngeal malignant tumors are SCCA. Some are nonkeratinizing, and this variety of SCCA is occasionally still referred to as lymphoepithelioma.
Clinical Presentation
Tongue base, glossotonsillar sulcus, and tonsillar cancer often presents as a level 2A mass due to cervical metastatic disease. Throat pain, odynophagia, dysphagia, “globus sensation,” and referred otalgia are also common presenting complaints.
Only a submucosal mass may be appreciated at physical examination in these primary sites. In such a situation, the likelihood of a minor salivary gland tumor and lymphoma goes up slightly, although many of the entirely submucosal cancers turn out to be SCCA (Figs. 195.1, 195.2, and 195.16). Other tumors are truly very uncommon and normally cannot be anticipated prebiopsy on the basis of their imaging appearance in all but the rarest circumstances. The tongue base is a common site of clinically mucosally nonapparent primary tumors that present with cervical adenopathy. Only the tonsillar fossa is a more common site of such “unknown primaries.” About half of these clinically nonapparent primaries will be detected by CT and/or MRI by an experienced observer, and this detection rate may very marginally increase with FDG-PET (Figs. 5.2 and 195.14).
Anterior tonsillar pillar lesions may present as incidentally discovered masses or in a search for a cause of sore throat and ear pain. Advanced lesions can cause trismus, dysphagia, and pain referred to the temple area (Fig. 195.3).
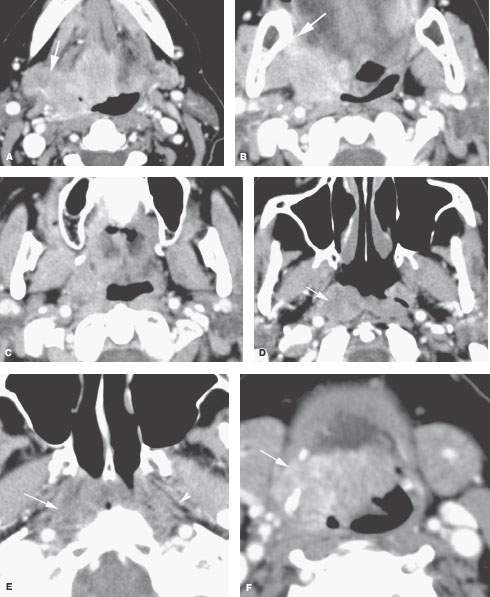
FIGURE 195.4. Contrast-enhanced computed tomography study of a patient with extensive tongue base cancer spreading to involve the tonsil and nasopharynx. In (A), the primary is visible in the tongue base and shows direct extension into the soft tissues of the neck to invade the submandibular gland (arrow). In (B), the tumor grows superiorly to invade the anterior and posterior tonsillar pillars and spreads toward the pterygomandibular raphe (arrow). In (C), there is spread to the level of the soft palate, so continued extension to the nasopharynx must be suspected. In (D), that spread to the nasopharynx along the fossa of Rosenmüller is confirmed; in (E), the spread in the nasopharynx can be seen to continue to the roof of the nasopharynx obliterating the parapharyngeal soft tissues (arrow) on the right compared to the normal soft tissue planes on the left. This spread is nearly to the skull base. In (F), the inferior extent of the tumor can be seen continuing to the attachment of the hyoglossus on the hyoid bone (arrow).
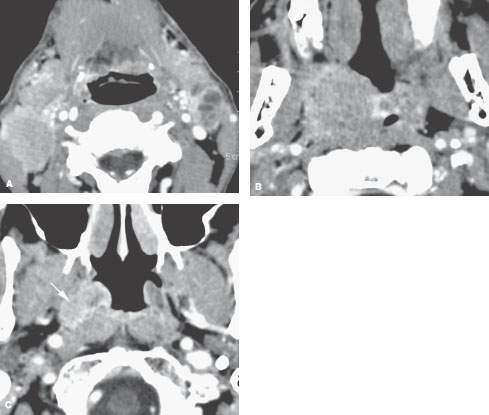
FIGURE 195.5. Tonsillar cancer presenting with bilateral level 2 adenopathy. On computed tomography study, the level 2 lymph nodes showing features suggestive of a poorly differentiated tumor are easily identified. The primarily submucosal tonsillar cancer involves the entire tonsillar fossa on the right. The clinically unsuspected spread to the level of the eustachian tube (arrow) and higher (not shown) seen in (C) was not expected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








