How to Image Osseous Trauma
- •
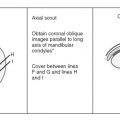
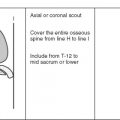
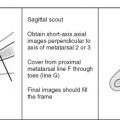
Coils and patient position: The patient should be placed in a comfortable position with passive restraints, such as tape or Velcro straps, applied to the region of interest to minimize motion. Pain medication also may be required in cases of acute trauma to improve patient comfort. Although the body coil may be used in cases where a large field of view is needed, whenever possible a smaller coil, such as a phased array pelvic coil or an appropriate surface coil, should be used.
- •
Image orientation: Images should be obtained in the axial plane and the sagittal or coronal planes, depending on the area of interest. The coronal plane is best for imaging the hips and proximal femora; sagittal images are most useful for the spine.
- •
Pulse sequences: Inversion recovery (STIR) sequences are the most sensitive for detecting abnormal marrow signal intensity that results from skeletal trauma and should be used in all cases. A fast spin echo–T2W sequence with fat saturation also is quite sensitive, but the incomplete fat saturation that sometimes occurs with this technique can produce areas of artifactually increased signal intensity, which can mimic marrow edema when none is present. T1W images should be obtained in at least one plane because they provide an excellent depiction of overall anatomy, and are reasonably sensitive for detecting osseous injuries, although they are less sensitive than STIR sequences. Gradient echo sequences should not be used when imaging osseous trauma with a high field strength magnet (>1T), because marrow pathology is obscured by susceptibility artifacts related to trabecular bone. With mid and low field strength magnets, however, some gradient echo sequences are quite sensitive for detecting traumatic injuries because susceptibility artifacts are less pronounced at these field strengths. Because of the exquisite sensitivity of MRI for detecting osseous injuries, a streamlined screening protocol may be used to provide a rapid diagnosis, minimize costs, and enhance patient throughput. For this purpose, we employ a three-sequence trauma protocol using T1 and STIR sequences to show osseous abnormalities optimally.
- •
Contrast: We do not use intravenous contrast material in cases of trauma.
ANATOMY
A familiarity with basic skeletal anatomy helps in understanding the MRI findings in osseous trauma. Cortical (compact) bone is found along the periphery of flat and tubular bones. The subchondral plate, the layer of cortical bone at the articular end of a long bone, plays an important role in providing support for the overlying articular cartilage.
Trabecular (cancellous) bone is composed of a meshwork of osseous struts that support the overlying cortex. Trabecular bone is found primarily in the axial skeleton and near the ends of long bones, where it plays an important role in absorbing dynamic stresses. Because of its elastic compliance, cancellous bone has a load-bearing capacity 10 times that of compact, cortical bone. This shock-absorbing capability is especially important around joints, where the trabecular bone dissipates axial forces away from the subchondral plate and overlying articular cartilage.
In a developing long bone, the physis (growth plate) allows for lengthening of the bone through enchondral ossification. Before closure, the growth plate constitutes the weak link in the muscle-tendon-bone and bone-ligament-bone units. As such, it is particularly vulnerable to traumatic injuries at epiphyses (at the ends of long bones) and apophyses (growth centers not involved in longitudinal bone growth, such as the trochanter of the hip.)
OVERVIEW OF OSSEOUS TRAUMA
Osseous injury may result from a single traumatic event, or may occur over time as a result of repetitive stresses that lead to the gradual breakdown and ultimate mechanical failure of the bone. Acute trauma may result in impaction injuries (ranging from bone contusions to complete fractures) or avulsion fractures in which a tendon or ligament pulls off a piece of bone, cartilage, or both. Chronic injuries, resulting from less intense, repetitive trauma, range from a focal stress reaction to a frank fatigue or insufficiency fracture.
IMAGING OPTIONS
Conventional radiographs should be the first modality used for evaluating osseous trauma, but many acute and chronic osseous injuries are not detectable on radiographs. Most of these radiographically occult injuries can be detected with radionuclide bone scanning, but this technique has several limitations. The examination requires 4 to 6 hours, delaying diagnosis in these patients, who often are awaiting triage in the emergency department and the scan may be falsely negative for 24 to 72 hours after the injury, especially in elderly patients. Finally, a positive scan is nonspecific because the images are of extremely low spatial resolution, and a wide variety of osseous pathology can result in abnormal uptake. This can be especially problematic in older patients, in whom insufficiency fractures and neoplasms are common.
MRI is exquisitely sensitive for detecting osseous injuries that result from either acute or chronic repetitive trauma. By using streamlined protocols, MRI can be cost-competitive with a bone scan, while providing a more rapid and specific diagnosis. As a result, we use MRI as the next study in a patient who has normal radiographs and a suspected osseous injury. A normal MR image essentially excludes the presence of an osseous injury. An additional strength of MRI is its ability to show soft tissue injuries that may mimic a fracture clinically in cases in which no osseous injury is present ( Fig. 8-1 ).

Acute Osseous Trauma
IMPACTION INJURIES
Contusion
Trabecular injuries that result from impaction forces are known as bone contusions, bone bruises , or microtrabecular fractures . Pathologic studies of these injuries reveal trabecular fractures and edema and hemorrhage in the adjacent marrow fat. MRI findings become evident within hours of the injury, and their detection is important for several reasons. An isolated bone contusion on an MR image may explain a patient’s symptoms and avoid an unnecessary arthroscopic procedure. The sites of contusion also may provide clues about the mechanism of injury and associated soft tissue abnormalities that may be present.
Additionally, although most contusions resolve without complications, there is evidence that focal contusions involving the subchondral bone are associated with damage to the overlying cartilage. Some investigators believe that this may place the patient at increased risk for collapse of the articular surface in the short term, or the development of osteoarthritis later. Detection of a subchondral contusion may result in a more conservative treatment plan, including a longer delay before returning to a normal activity level, to allow for trabecular healing and to minimize the potential for collapse of the overlying articular surface.
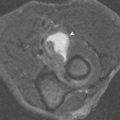
Bone contusions are most conspicuous on STIR or fat-saturated T2W images, where they appear as focal areas of increased signal intensity, usually with poorly defined margins, presumably secondary to the hemorrhage and edema related to the trabecular fractures ( Fig. 8-2 ). , Contusions are typically of intermediate signal intensity on T1W images (lower than fat, higher than muscle) because marrow fat is intermixed with the hemorrhage and edema. Contusions are easily missed on non–fat-saturated fast spin echo–T2W images because the trauma-related edema and surrounding marrow fat display similar signal intensities.

Contusion Patterns
By analyzing the locations of osseous contusions, the mechanism of injury often can be inferred, and associated soft tissue abnormalities can be predicted and carefully searched for. Two commonly encountered patterns are discussed here ( Box 8-1 ).
Anterior Cruciate Ligament Tear
Lateral Compartment
- •
Mid anterior lateral femoral condyle
- •
Posterior lateral tibial plateau
Medial Compartment
- •
Mid anterior medial femoral condyle
- •
Posterior medial tibial plateau
Patellar Dislocation
- •
Medial facet of the patella
- •
Anterior lateral femoral condyle
Anterior Cruciate Ligament Tear.
Osseous contusions are evident on MRI studies in approximately 80% of patients with acute anterior cruciate ligament tears. The most common mechanism of injury that results in a complete tear of the anterior cruciate ligament involves a twisting force combined with a valgus stress. The ensuing impaction of the mid to anterior aspect of the lateral femoral condyle against the posterolateral tibial plateau results in typical contusions at these sites ( Fig. 8-3 ). Another contusion pattern often is seen concurrently in the medial compartment of the knee after an anterior cruciate ligament tear. These contusions involve the mid to anterior medial femoral condyle and posteromedial tibial plateau. These contusions probably arise from a medial impaction force that results from the unstable knee rebounding after the anterior cruciate ligament tear and lateral injuries have occurred (see Fig. 8-3 ).

Lateral Patellar Dislocation.
The typical contusions that result from patellar dislocation involve the medial patellar facet and the lateral femoral condyle, and are explained by the mechanism of injury. The patella dislocates in a lateral direction. As it relocates, the medial facet of the patella impacts against the anterolateral margin of the lateral femoral condyle, resulting in contusions at these sites ( Fig. 8-4 ). Common associated findings include a tear of the medial patellar retinaculum, a large joint effusion, and a chondral or osteochondral injury to the medial patella or lateral trochlear groove. Less commonly, the osteochondral injury may involve the weight-bearing surface of the lateral femoral condyle. ,

Radiographically Occult Fracture
In the case of a radiographically occult fracture, in addition to marrow edema, a fracture line is present. The fracture line occasionally may be obscured by adjacent marrow edema, but usually is identified as a linear or curvilinear focus of low signal intensity on T1W images that may show either low or high signal intensity on STIR images ( Figs. 8-5 to 8-7 ). Marrow signal intensity returns to normal with healing.



It has been well established that MRI is able to show radiographically occult fractures in a rapid, cost-effective manner, allowing for optimal patient management. , This is possible because the associated marrow edema and hemorrhage are present on MR images from the time of injury. Even if a fracture is evident on conventional radiographs, MRI may provide additional useful information regarding the true extent of the fracture, the presence of additional fractures or contusions, and associated soft tissue injuries.
AVULSION INJURIES
Avulsion fractures occur when excessive tensile forces result in a piece of bone or cartilage being pulled away from the host bone by ligament, tendon, or capsular structures. These injuries may occur with a single, acute event or may result from repetitive avulsive stresses.
Although these injuries can occur at any age, they are most common in the developing skeleton (children and especially adolescents) because of the imbalance between muscle strength and the weak, unfused apophysis. Avulsion fractures occur less frequently in adults, in whom the musculotendinous junction is the site that is most vulnerable to injuries from excessive tensile forces.
Common Sites ( Table 8-1 )
Avulsion fractures are most common in the pelvis. Frequent sites include the anterior superior iliac spine (sartorius and tensor fascia lata tendons), the anterior inferior iliac spine (rectus femoris tendon) ( Fig. 8-8 ), ischial tuberosity (hamstring tendon), iliac crest (abdominal muscles), symphysis pubis, and inferior pubic rami (adductor muscles and gracilis tendon). In the proximal femur, the greater trochanter may be affected (hip rotators, including the gluteus minimus and medius tendons). The lesser trochanter may rarely avulse in a young patient (iliopsoas tendon), but in an adult this injury is virtually always secondary to metastatic disease in the trochanter.
| Site | Tendon or Ligament | |
|---|---|---|
| Pelvis | Ischial tuberosity | Hamstrings |
| Anterior superior iliac spine | Sartorius/tensor fascia lata | |
| Anterior inferior iliac spine | Rectus femoris | |
| Symphysis/inferior pubic ramus | Adductors/gracilis | |
| Femur | Greater trochanter | Gluteus medius, minimus/hip rotators |
| Lesser trochanter | Iliopsoas (young person) (older patient = metastasis) | |
| Knee | Lateral tibial plateau (Segond fracture) | Lateral capsular ligament (mid third) |
| Fibular head |
| |
| Tibial eminence | Anterior cruciate ligament | |
| Posterior tibial plateau | Posterior cruciate ligament | |
| Inferior pole of patella | Patellar tendon (Sinding-Larsen-Johansson syndrome) | |
| Tibial tubercle | Patellar tendon (Osgood-Schlatter disease) | |
| Ankle/foot | Calcaneus | Achilles |
| Posterior margin—distal tibia | Posterior ankle joint capsule | |
| Dorsal margin, neck of talus | Anterior ankle joint capsule | |
| Base fifth metatarsal | Peroneus brevis | |
| Humerus | Greater tubercle | Supraspinatus, infraspinatus, teres minor |
| Lesser tubercle | Subscapularis | |
| Proximal shaft | Pectoralis major or latissimus dorsi | |
| Elbow | Medial epicondyle | Flexor/pronator tendon |
| Ulnar (sublime) tubercle | Ulnar collateral ligament |

Common sites for avulsion fractures around the knee include the lateral tibial plateau (Segond fracture at the attachment of the lateral capsular ligament) ( Fig. 8-9 ), the fibular head (biceps femoris tendon, lateral collateral ligament), the tibial eminence (anterior cruciate ligament), posterior tibial plateau (posterior cruciate ligament) and tibial tubercle (patellar tendon) ( Fig. 8-10 ). Avulsion of the inferior pole of the patella can occur in children secondary to chronic avulsive forces (Sinding-Larsen-Johansson syndrome), or as an acute cartilaginous avulsion fracture (patellar sleeve fracture).


Avulsion of the posterior tuberosity of the calcaneus by the Achilles tendon (calcaneal insufficiency avulsion fracture) is seen almost exclusively in diabetics. Avulsion fractures also may be seen along the dorsal surface of the neck of the talus or posterior margin of the distal tibia secondary to pull of the anterior and posterior portions of the ankle joint capsule. The base of the fifth metatarsal is another common site for an avulsion fracture (peroneus brevis tendon).
The most common avulsion fracture in the upper limb involves the medial epicondyle apophysis (common flexor/pronator tendon) in children. The avulsed fragment may become entrapped in the humeral–ulnar joint space. Other sites in the upper extremity include the greater and lesser tuberosities (rotator cuff tendons), deltoid insertion on the lateral humeral shaft, and the insertion sites of the pectoralis major and latissimus dorsi tendons along the intertubercular sulcus.
MRI Appearance
Avulsion fractures typically show abnormal marrow signal at the site of the injury, but the extent of the marrow abnormality generally is limited, and significantly less than what is seen with an impaction mechanism of injury. Prominent signal abnormality often is seen in the adjacent soft tissues, and the appearance may mimic a neoplasm or infection if a history of trauma is not obtained. In these cases, correlation with conventional radiographs generally is useful because the injuries often have a typical radiographic appearance.
Repetitive Trauma
Stress injuries of bone typically are divided into two categories: insufficiency and fatigue fractures. Insufficiency fractures result from normal stresses applied to abnormal bone, whereas fatigue fractures occur when abnormal or unaccustomed stresses are applied to normal bone ( Box 8-2 ).
Insufficiency Fracture
- •
Normal stresses → abnormal bone
- •
Causes
- •
Osteoporosis
- •
Osteomalacia
- •
Steroids
- •
Paget’s disease
- •
Hyperparathyroidism
- •
Rheumatoid arthritis
- •
Radiation
- •
Fatigue Fracture
- •
Abnormal stresses → normal bone
- •
Causes
- •
New activity
- •
↑ Activity level (↑ exertion or duration)
- •
Poor equipment (eg, worn-out shoes)
- •
Abnormal biomechanics (eg, excessive pronation)
- •
INSUFFICIENCY FRACTURES
Several conditions weaken the elastic resistance of bone and predispose it to insufficiency fractures. The most common is osteoporosis, but others include Paget’s disease, osteomalacia, and irradiation. Clinical diagnosis often is challenging because the onset of symptoms may be insidious.
MRI Appearance
Radiographic findings of insufficiency fractures often are subtle and difficult to appreciate because of the osteopenia associated with most of these conditions ( Fig. 8-11 ). MRI is able to detect these injuries with a very high degree of sensitivity, however. Insufficiency fractures appear as amorphous or linear foci of decreased signal intensity on T1W images. High signal intensity edema is seen on STIR sequences, classically surrounding a low signal intensity fracture line. Their appearance may mimic neoplasm, but a specific diagnosis of insufficiency fracture usually can be provided based on the MRI morphology and location of the lesions.