Drug-Induced Esophagitis
Since its original description in 1970, drug-induced esophagitis has been recognized as a relatively common condition in today’s pill-oriented society. The medications implicated most frequently include tetracycline, doxycycline, potassium chloride, quinidine, aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), and alendronate sodium. These patients may have severe esophageal symptoms, but drug-induced esophagitis usually resolves after withdrawal of the offending agent. Although conventional single-contrast barium studies have limited value in detecting mucosal abnormalities associated with drug-induced esophagitis, double-contrast esophagography is a valuable technique for diagnosing this condition.
Pathogenesis
The type and degree of injury that occurs in drug-induced esophagitis depend not only on the properties of the offending medication but also on the manner in which it is taken. Many patients have a history of ingesting the medication with little or no water before going to bed. As a result, the tablets or capsules may become lodged in the midesophagus, where they are compressed by the adjacent aortic arch or left main bronchus. Drug-induced esophagitis is therefore believed to represent a focal contact esophagitis, with injury to the adjacent mucosa by the dissolving pills. Less frequently, prolonged retention of the medication may result from esophageal compression by an enlarged heart. Occasionally, drug-induced esophagitis may be caused by abnormal motility or preexisting strictures that delay transit of pills from the esophagus.
Causative Agents
Tetracycline and Doxycycline
Tetracycline and doxycycline, two widely used antibiotics, are responsible for at least 50% of all cases of drug-induced esophagitis. Because these medications are given in the form of capsules that are relatively acidic, prolonged retention of the capsules in the upper or midesophagus may cause superficial ulceration of the adjacent mucosa. Although doxycycline (pH 3.0) is slightly less acidic than tetracycline (pH 2.3), it dissolves more slowly and forms an adherent gel, presumably accounting for the high frequency of esophagitis in patients taking this agent. Affected individuals almost never develop strictures, however, because the ulcers caused by tetracycline and doxycycline are so small and superficial that they rarely cause enough scarring and fibrosis to produce a stricture.
Potassium Chloride
Potassium chloride tablets may produce a severe form of drug-induced esophagitis. These patients often have mitral valvular disease with an enlarged left atrium compressing the distal esophagus, so passage of the potassium chloride tablets is impeded at this level. Subsequent release of potassium chloride over a localized area of esophageal mucosa may cause severe chemical injury with focal ulceration and stricture formation. As a result, potassium supplements are sometimes given in liquid form to patients with known cardiomegaly to prevent this complication. Even liquid potassium, however, has been described as a cause of drug-induced esophagitis.
Quinidine
Because oral quinidine is often given for cardiac arrhythmias, these patients may have associated cardiomegaly, with compression of the distal esophagus by an enlarged left atrium or ventricle. Retained quinidine above this level may have a corrosive effect on the adjacent mucosa, causing ulceration and strictures.
Nonsteroidal Anti-inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) have been implicated with increasing frequency in the development of esophagitis. Major offending agents include aspirin, phenylbutazone, indomethacin (Indocin), ibuprofen (Motrin), naproxen (Naprosyn), piroxicam (Feldene), and sulindac (Clinoril). These NSAIDs not only may cause a focal contact esophagitis, but sometimes may lead to stricture formation.
Alendronate
Alendronate sodium (Fosamax) is an aminobisphosphonate, a selective inhibitor of osteoclast-mediated bone resorption, that has been used with increasing frequency in the nonhormonal treatment of postmenopausal osteoporosis. This agent may be associated with the development of a severe form of ulcerative esophagitis and stricture formation in the distal esophagus. The mechanism of injury is uncertain. Topical corrosive injury may be a contributing factor, but the high frequency of ulceration in the distal esophagus suggests that there is a reflux-mediated component in these patients.
Other Drugs
Other oral medications that have been implicated in the development of drug-induced esophagitis include emepronium bromide, ferrous sulfate, alprenolol chloride, ascorbic acid, theophylline, cromolyn sodium, and antibiotics such as clindamycin and lincomycin.
Clinical Findings
Patients with drug-induced esophagitis typically present with odynophagia or unremitting chest pain accentuated by swallowing. Others may present with signs of upper gastrointestinal (GI) bleeding. Symptoms usually develop within several hours to days after taking the medication. The symptoms of drug-induced esophagitis also tend to resolve rapidly after withdrawal of the offending agent, so most patients are asymptomatic within 7 to 10 days after stopping the medication. Occasional patients may have progressive dysphagia because of the development of strictures.
Radiographic Findings
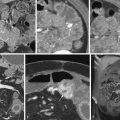
The radiographic findings in drug-induced esophagitis depend on the nature of the offending medication. Tetracycline, doxycycline and, less commonly, other medications cause superficial ulceration in the esophagus without permanent sequelae. Double-contrast esophagography is a useful technique for detecting shallow ulcers that cannot easily be recognized on single-contrast studies. Affected individuals may have a solitary ulcer ( Fig. 21-1A ), several discrete ulcers ( Fig. 21-1B ), or multiple small ulcers on a normal background mucosa ( Fig. 21-1C ). The ulcers are usually clustered together in the midesophagus near the level of the aortic arch or left main bronchus. These ulcers may be recognized en face as punctate, linear, ovoid, stellate, or serpiginous collections of barium or in profile as shallow depressions (see Fig. 21-1 ). When esophageal ulcers are drug induced, a follow-up esophagogram 7 to 10 days after withdrawal of the offending agent often shows dramatic healing of the lesions.

Potassium chloride, quinidine, NSAIDs, and alendronate tend to cause a more severe form of esophagitis, sometimes associated with stricture formation. Potassium chloride and quinidine may result in particularly large ulcers with considerable surrounding edema and inflammation, mimicking the appearance of an ulcerated carcinoma ( Fig. 21-2A ). Subsequent scarring and fibrosis occasionally lead to the development of strictures that typically appear as segmental areas of concentric narrowing above the level of an enlarged left atrium ( Fig. 21-2B ). In contrast, aspirin and other NSAIDs sometimes produce giant, flat ulcers that are several centimeters or longer ( Fig. 21-3A ). Healing of these ulcers may result in smooth, re-epithelialized depressions that are sometimes mistaken for active ulcer craters ( Fig. 21-3B ). Finally, alendronate may be associated with the development of severe ulcerative esophagitis and stricture formation in the distal esophagus ( Fig. 21-4 ).



Differential Diagnosis
Herpes esophagitis is the major consideration in the differential diagnosis for discrete, superficial ulcers in the upper or midesophagus. Although viral ulcers may be indistinguishable from the ulcers of drug-induced esophagitis, the correct diagnosis can usually be suggested on the basis of the clinical history. Occasionally, however, herpes esophagitis may occur in otherwise healthy individuals who have no underlying immunologic problems (see Chapter 20 ). The diagnosis of drug-induced esophagitis should therefore be considered only when there is a definite temporal relationship between ingestion of the offending medication and the onset of esophagitis.
Reflux esophagitis is a more common cause of superficial ulceration, but the ulcers are almost always confined to the distal esophagus. Mediastinal irradiation and caustic ingestion are other causes of ulceration, but the correct diagnosis is usually suggested on clinical grounds. Crohn’s disease may also be associated with shallow ulcers in the esophagus, but these patients usually have advanced Crohn’s disease in the small bowel or colon (see later, “ Crohn’s Disease ”). Finally, giant drug-induced ulcers may be indistinguishable from ulcerated carcinomas or from cytomegalovirus or human immunodeficiency virus (HIV) ulcers in patients with AIDS (see Chapter 20 ). However, these conditions can usually be differentiated by the clinical history and presentation.
Because drug-induced strictures are usually located at a considerable distance from the gastroesophageal junction, they must be differentiated from high esophageal strictures caused by Barrett’s esophagus, mediastinal irradiation, caustic ingestion, eosinophilic esophagitis, and primary or metastatic tumors. However, the possibility of a drug-induced stricture should be suspected in patients with cardiomegaly who have a history of taking potassium chloride or quinidine.
Radiation Esophagitis
Malignant tumors involving the lungs, mediastinum, or thoracic spine are often treated by high-dose, external-beam radiation to the chest. The major limiting factor with this form of treatment is esophageal damage by ionizing radiation. Total doses of 45 to 60 Gy may lead to severe esophagitis, with irreversible damage and stricture formation. Smaller doses (20 to 45 Gy) may cause a self-limited esophagitis without permanent sequelae. Most patients have clinical evidence of esophagitis shortly after the onset of radiation therapy, but barium studies are not usually performed during this period. Instead, esophagography has been used primarily to detect strictures or other signs of chronic radiation injury. Both the acute and the chronic forms of radiation esophagitis are considered in this chapter.
Pathogenesis
Experiments on laboratory animals have shown that high-dose radiation to the esophagus causes an acute, self-limited form of esophagitis within 1 to 3 weeks of the onset of radiation therapy. After the acute stage of radiation injury and subsequent epithelial repair, chronic radiation esophagitis is characterized by progressive submucosal scarring and fibrosis with the development of esophageal strictures 4 to 8 months after completion of radiation therapy at doses of 30 to 50 Gy. If the radiation dose is more than 60 Gy, esophageal strictures may develop within 3 to 4 months.
Clinical Findings
Most patients who receive mediastinal irradiation develop a self-limited esophagitis, manifested by acute onset of substernal burning, odynophagia, or dysphagia within 1 to 3 weeks after the onset of radiation therapy. The symptoms usually subside within 24 to 48 hours but may occasionally persist for several weeks. Because these patients are immunocompromised, the development of odynophagia may erroneously be attributed to opportunistic esophagitis. The correct diagnosis should be suggested, however, by the temporal relationship between the onset of radiation therapy and onset of symptoms. When acute radiation esophagitis is suspected, these patients are usually treated empirically with viscous lidocaine and analgesics, so radiologic or endoscopic examinations are not often performed in this setting.
Chronic radiation injury to the esophagus may cause dysphagia within several months after completion of radiation therapy. Dysphagia may result from esophageal dysmotility or, less commonly, from the development of strictures. Mild radiation strictures may be successfully dilated, but more severe strictures necessitate feeding tube placement or other palliative measures. Occasionally, severe radiation injury may lead to life-threatening complications such as an esophageal airway fistula or esophageal perforation. However, these unusual complications of radiation therapy almost always occur in an area of the esophagus involved by tumor and rarely in normal irradiated tissue.
Radiographic Findings
Although most patients with acute radiation esophagitis are treated empirically, barium studies are sometimes performed when the clinical diagnosis is uncertain. This condition may be manifested on double-contrast esophagography by a granular appearance of the mucosa and decreased distensibility from edema and inflammation of the irradiated segment ( Fig. 21-5A ). Other patients with acute radiation esophagitis have multiple small, discrete ulcers within a known radiation portal ( Fig. 21-6 ). With more severe disease, the esophagus may have a grossly irregular, serrated contour secondary to larger areas of ulceration and mucosal sloughing.


After the acute phase of radiation injury, the most frequent finding on barium studies is abnormal esophageal motility, which usually develops 4 to 8 weeks after completion of radiation therapy. This dysmotility is characterized by interruption of primary peristalsis at the superior border of the radiation portal, with numerous nonperistaltic contractions distal to the point of disruption of the primary wave. Less commonly, the irradiated segment may be aperistaltic.
Radiation strictures in the esophagus usually develop 4 to 8 months after completion of radiation therapy. Higher doses of radiation may shorten the interval for developing a stricture but have no effect on its length or caliber. The strictures typically appear as relatively smooth, tapered areas of concentric narrowing in the upper or midesophagus within a preexisting radiation portal ( Fig. 21-5B ).
Tracheoesophageal and esophagobronchial fistulas are potentially life-threatening complications of mediastinal irradiation. These fistulas are usually caused by radiation necrosis, with erosion of tumor into the esophagus and adjacent airway. The most frequent site of fistula formation is the left main bronchus, where it crosses the esophagus at the level of the fourth or fifth thoracic vertebra. When an esophageal airway fistula is suspected, the radiologic examination should be performed with barium sulfate because a water-soluble contrast agent may cause severe pulmonary edema if it enters the lungs via a fistula.
Differential Diagnosis
When acute odynophagia or dysphagia develops several weeks after mediastinal irradiation, the major diagnostic considerations are acute radiation esophagitis versus infectious esophagitis in an immunocompromised patient. Candida esophagitis should be suggested on barium studies by mucosal plaques, whereas herpes esophagitis should be suggested by discrete superficial ulcers without plaque formation. In contrast, radiation esophagitis may be manifested by a granular appearance or ulceration, but the area of involvement almost always conforms to a known radiation portal, with a sharp demarcation at the superior and inferior borders of the portal (see Fig. 21-6 ).
Although many conditions should be considered in the differential diagnosis for an upper or midesophageal stricture, the major considerations after mediastinal irradiation should be a radiation stricture versus esophageal involvement by recurrent mediastinal tumor (see Chapter 24 ). A concentric area of smooth, tapered narrowing should favor the diagnosis of a radiation stricture, whereas irregular, eccentric narrowing with extrinsic mass effect should suggest a malignant tumor. When the radiographic findings are equivocal, computed tomography (CT) may be helpful for differentiating a radiation stricture from recurrent tumor in the mediastinum.
Caustic Esophagitis
Caustic esophagitis did not become a serious medical problem in the United States until 1967, when concentrated liquid lye solutions were made commercially available to the U.S. public for use as drain cleaners. Because they could be swallowed rapidly, liquid corrosives exposed all surfaces of the upper GI tract to potentially life-threatening caustic injury. Thus, caustic esophagitis became an important clinical entity. Endoscopy has generally been advocated as the best means of assessing the extent and severity of esophageal injury, but radiologic studies may also provide valuable information during the acute and chronic stages of the disease.
Pathogenesis
Caustic injury to the esophagus may be caused by ingestion of alkali, acids, ammonium chloride, phenols, silver nitrate, and a variety of other common household products. Children usually ingest these corrosive substances accidentally, whereas adults take them intentionally to commit suicide. The degree of injury depends on the nature, concentration, and volume of the corrosive agent as well as the duration of tissue contact. In the United States, most patients with caustic esophagitis swallow some form of liquid lye (concentrated sodium hydroxide), which causes severe esophageal injury by liquefaction necrosis. In contrast, ingested acids cause tissue damage by coagulative necrosis, forming a protective eschar that tends to limit further tissue penetration. Nevertheless, acidic agents may produce severe esophagitis and strictures comparable to those caused by lye.
Caustic esophagitis is characterized pathologically by three phases of injury—an acute necrotic phase, an ulceration-granulation phase, and a final phase of cicatrization and scarring. The initial phase of acute cellular necrosis begins immediately after caustic ingestion. This acute phase usually lasts 1 to 4 days and is accompanied by an intense inflammatory reaction in the surrounding tissues. The ulceration-granulation phase begins 3 to 5 days after caustic ingestion and is characterized by edema, ulceration, and sloughing of necrotic mucosa. During the next 7 to 14 days, subsequent healing leads to the production of granulation tissue in areas of mucosal sloughing. The esophagus is thought to be weakest and therefore most vulnerable to perforation during this period. The final phase of cicatrization begins 3 to 4 weeks after caustic ingestion. Depending on the degree of injury, this cicatrization process may lead to severe scarring and stricture formation.
Clinical Findings
Acute caustic esophagitis may be manifested by odynophagia, chest pain, drooling, vomiting, or hematemesis. Severe substernal pain, fever, and shock usually indicate esophageal perforation and mediastinitis. Associated gastric perforation leads to the development of peritonitis. If patients survive the acute illness, there may be a latent period of several weeks, during which they are no longer symptomatic. Subsequently, however, these patients often develop severe dysphagia secondary to progressive stricture formation 1 to 3 months after the initial injury.
Diagnosis and Treatment
When caustic ingestion is suspected, examination of the mouth and oropharynx sometimes reveals obvious tissue injury, with ulceration of the lingual, buccal, or pharyngeal mucosa. Liquid corrosives may be swallowed rapidly, however, so caustic esophagitis often occurs without associated pharyngeal injury. Direct visualization of the esophagus is therefore required to confirm this diagnosis. A limited radiographic study may be performed with a water-soluble contrast agent to detect an esophageal or gastric perforation or other signs of caustic injury. However, most authors advocate endoscopy within 24 hours of caustic ingestion (assuming that there are no clinical or radiographic signs of perforation) to assess the extent and severity of esophageal injury.
Treatment of caustic esophagitis is generally aimed at preventing stricture formation. Some advocate early administration of steroids and antibiotics to inhibit collagen formation and decrease the risk of infection. Others believe that esophageal bougienage should be performed as early as 2 to 3 weeks after caustic ingestion. Despite such measures, 10% to 40% of patients with caustic esophagitis develop strictures. Some of these strictures may respond to periodic dilation procedures, but others eventually require an esophageal bypass operation, such as a colonic interposition (see Chapter 27 ). When strictures develop after caustic ingestion, barium studies may be used to determine the degree and extent of stricture formation as well as the response to treatment. Patients with lye strictures are also thought to have a substantially increased risk of developing esophageal carcinoma 20 to 40 years after the initial caustic injury. This subject is discussed in detail in Chapter 23 .
Radiographic Findings
Chest and abdominal radiographs should be obtained routinely for patients who have ingested caustic agents. With severe esophageal injury, posteroanterior and lateral radiographs of the chest may show a dilated, gas-filled esophagus or, if esophageal perforation has occurred, mediastinal widening, pneumomediastinum, or pleural effusions. Similarly, abdominal radiographs may reveal pneumoperitoneum or a localized gas-containing abscess from gastric perforation.
When esophageal or gastric perforation is suspected in patients who have normal or equivocal chest and abdominal radiographs, a water-soluble contrast study should be performed to document the presence of a leak. Water-soluble contrast agents are used because barium in the mediastinum may cause mediastinal fibrosis, and barium in the peritoneal cavity may cause peritonitis. If there is no evidence of esophageal or gastric perforation with a water-soluble contrast agent, however, barium should be given for a more detailed examination.
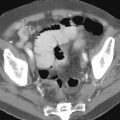
Acute caustic esophagitis may be manifested on esophagography by esophageal dysmotility with poor primary peristalsis, nonperistaltic contractions, diffuse esophageal spasm, or a dilated, atonic esophagus ( Fig. 21-7 ). Some authors believe that the latter finding indicates diffuse muscular necrosis and that it is an ominous sign of impending esophageal perforation. These various motor abnormalities have been attributed to edema, inflammation, or destruction of ganglion cells in Auerbach’s plexus.

In other patients, acute caustic esophagitis may be manifested by multiple shallow, irregular ulcers ( Fig. 21-8 ). With more severe caustic injury, the esophagus may be diffusely narrowed and may have a grossly irregular contour because of marked edema, spasm, and ulceration ( Fig. 21-9 ). Occasionally, contrast material may dissect beneath partially sloughed mucosal fragments, producing a double-barreled appearance.


Subsequent cicatrization and fibrosis may lead to the development of one or more strictures in the esophagus 1 to 3 months after the acute injury. The strictures usually appear as relatively long areas of smooth, tapered narrowing in the upper or midesophagus; some strictures may have an irregular contour or eccentric areas of sacculation because of asymmetric scarring ( Fig. 21-10 ). With severe scarring, the entire thoracic esophagus may have a threadlike, filiform appearance ( Fig. 21-11 ). This finding should be highly suggestive of a caustic stricture because other conditions are rarely associated with such severe esophageal narrowing. When esophagography is performed after caustic ingestion, the stomach should also be evaluated to determine whether associated gastric injury is present. This subject is discussed in detail in Chapter 30 .


Differential Diagnosis
Acute caustic esophagitis may be difficult to differentiate from severe cases of reflux, infectious, drug-induced, or radiation esophagitis. However, reflux esophagitis tends to involve the distal esophagus, drug-induced esophagitis usually involves the midesophagus, and radiation esophagitis occurs within a preexisting radiation portal. In contrast, the site of caustic injury in the esophagus is unpredictable because these patients may have segmental or diffuse esophagitis involving the cervical or thoracic esophagus. Whatever the radiographic findings, the diagnosis of caustic esophagitis is usually apparent from the clinical history.
The classic finding of a long, tapered stricture in the cervical or thoracic esophagus should suggest prior caustic ingestion. However, localized caustic strictures in the upper or midesophagus may be indistinguishable from high esophageal strictures from other causes, including Barrett’s esophagus, mediastinal irradiation, oral medications, metastatic tumor or, rarely, dermatologic diseases such as epidermolysis bullosa dystrophica and benign mucous membrane pemphigoid. When a lye stricture has irregular margins or relatively abrupt borders, differentiation from an infiltrating carcinoma may also be difficult. The ability to distinguish benign from malignant lesions is particularly important because of the increased risk of developing esophageal carcinoma in long-standing lye strictures ( Fig. 21-12 ). Thus, endoscopy and biopsy may be required for a definitive diagnosis.

Idiopathic Eosinophilic Esophagitis
Since its original description by Attwood and associates in 1993, eosinophilic esophagitis has been recognized as a chronic inflammatory disorder in children and adults. Eosinophilic esophagitis has been diagnosed with greater frequency over the past 2 decades, probably because of increasing awareness and increasing prevalence of this condition. The diagnosis is established on pathologic grounds by an increased number of intraepithelial eosinophils (more than 20/high-power field) on endoscopic biopsy specimens from the esophagus. The cause is uncertain, but investigators believe that this condition develops as a result of an allergic immune response to ingested food items involving T-cell mediated hypersensitivity and immunoglobulin E (IgE)–mediated pathways, leading to eosinophilic activation, inflammation, and fibrosis. Most patients with eosinophilic esophagitis do not have eosinophilic infiltration of the stomach and small bowel (eosinophilic gastroenteritis).
Clinical Findings
Adults with eosinophilic esophagitis are typically young men who present with long-standing dysphagia and recurrent food impactions. These individuals may have an atopic history (e.g., asthma, allergic rhinitis, and other allergic conditions) and peripheral eosinophilia, but eosinophilic esophagitis often occurs as an isolated condition in the absence of an allergic history or peripheral eosinophilia.
Based on the assumption that food allergens act as antigenic stimulation for eosinophilic inflammation of the esophagus, most patients are treated with antiallergy therapy, including oral steroids, topical steroids (swallowing metered doses of aerosolized steroid preparations), and elemental diets (i.e., protein-free diets) or elimination food diets (diets that exclude food items most commonly associated with food allergies), with varying degrees of success. Patients with strictures causing intractable dysphagia may undergo endoscopic dilation procedures, but these individuals often have only transient relief of dysphagia, so multiple dilations may be required.
Radiographic Findings
Eosinophilic esophagitis may be manifested on esophagography by strictures, rings, diffuse esophageal narrowing, or some combination of these findings. Not infrequently, affected patients develop one or more segmental strictures in the upper or midesophagus or, less commonly, distal esophagus. These strictures typically appear as relatively long segments of concentric narrowing with smooth contours and tapered margins, although strictures in the distal esophagus tend to be shorter than those in the upper or midesophagus ( Fig. 21-13A ). Other patients may develop a so-called ringed esophagus, manifested on barium studies by distinctive ringlike indentations, with multiple closely spaced concentric rings traversing the lumen (see Fig. 21-13A ). The rings may be associated with strictures or a small-caliber esophagus (see later) or may occur as an isolated finding in the esophagus. Although the pathogenesis is uncertain, such rings have been well documented at endoscopy, producing a typical corrugated appearance. Still other patients with eosinophilic esophagitis may have diffuse loss of caliber of most or all of the thoracic esophagus, resulting in a so-called small-caliber esophagus ( Fig. 21-13B ). Paradoxically, these long segments of narrowing can be more difficult to recognize on barium studies than shorter segments of narrowing because of their long length, uniform luminal diameter, and smooth contour, without obvious demarcations from adjacent normal-caliber esophagus. Despite the frequent subtlety of this finding, eosinophilic esophagitis should be suspected when a small-caliber esophagus is detected on barium studies in the proper clinical setting. In symptomatic patients, treatment with topical steroids can lead to improved esophageal diameter and relief of solid-food dysphagia. It is therefore unclear whether the small-caliber esophagus results from actual fibrosis and stricture formation or other pathophysiologic mechanisms.

Other patients with eosinophilic esophagitis may have abnormal esophageal motility, with an increased frequency of nonperistaltic contractions or even an achalasia-like syndrome. Rarely, small, sessile eosinophilic polyps may be found in the esophagus.
Differential Diagnosis
Upper or midesophageal strictures in eosinophilic esophagitis cannot always be differentiated from high esophageal strictures caused by Barrett’s esophagus, mediastinal irradiation, caustic ingestion, and metastatic tumor. The presence of an atopic history or peripheral eosinophilia, however, should suggest the correct diagnosis. In contrast, distal esophageal strictures in eosinophilic esophagitis may be impossible to differentiate from peptic strictures. Rarely, a long esophageal stricture or even a small-caliber esophagus may develop in patients with lichen planus involving the esophagus.
A ringed esophagus has also been described in patients with congenital esophageal stenosis. These patients may have corrugated esophageal strictures with multiple concentric rings indistinguishable from those in eosinophilic esophagitis. Although congenital esophageal stenosis is usually not associated with an allergic history or peripheral eosinophilia, this condition also occurs in young men with long-standing dysphagia, and biopsy specimens from the esophagus may also reveal increased numbers of intraepithelial eosinophils. Because of the similarities in the clinical, radiographic, and pathologic findings of these conditions, some of the reported patients with congenital esophageal stenosis may have had unrecognized eosinophilic esophagitis as the cause of their symptoms.
The differential diagnosis of the ringed esophagus includes fixed transverse folds in patients with strictures, but these folds generally are incomplete and further apart, producing a characteristic stepladder appearance. The feline esophagus could also conceivably be mistaken for the ringed esophagus of eosinophilic esophagitis, but these transverse striations occur as a transient phenomenon and are not associated with strictures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree