Nonencapsulated, retroperitoneal structure that lies in the anterior pararenal space between the duodenal loop and the splenic hilum.
Supplied by gastroduodenal artery (GDA) and splenic artery.
Length: 12.5–15 centimeters.
Parts: Head, uncinate process, neck, body, and tail.
Two ducts: Main pancreatic duct (MPD)—Duct of Wirsung—drains through major papilla.
Accessory pancreatic duct—Duct of Santorini—open into the duodenum at minor papilla.
USG: Normally, it has homogenously hyperechoic echotexture.
With aging and obesity, it becomes more echogenic as a result of fatty infiltration.
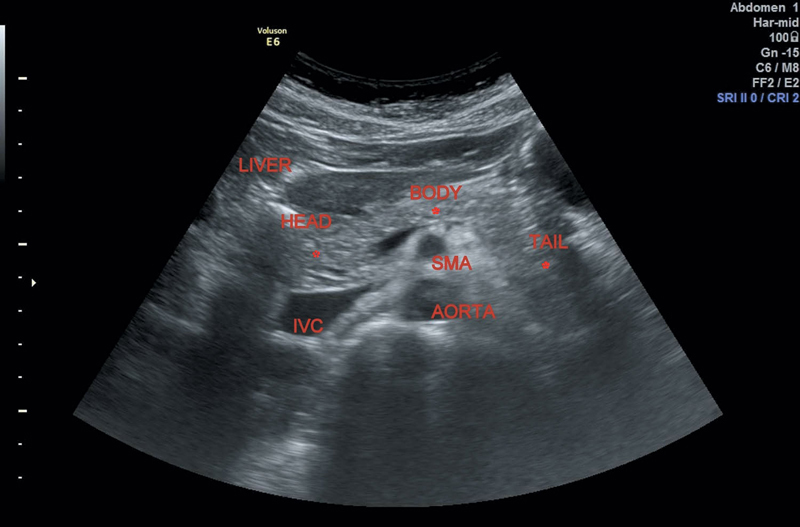
Anteroposterior (AP) dimensions of normal (Figure 6.1):
Head—Up to 3.0 centimeters.
Figure 6.1 Depicting normal anatomy of pancreas and adjacent structures.
Body—Up to 2.5 centimeters.
Tail—Up to 2.0 centimeters.
GDA lies anteriorly and common bile duct (CBD) lies posteriorly in the pancreatic head.
Sometimes the posterior half of pancreatic head reveals diminished echogenicity due to lesser fat content of ventral embryonic anlage. Can simulate a hypoechoic lesion and has to be differentiated by lack of biliary dilatation and absence of mass effect.
Patient preparation—Minimum fasting of 6 hours.
Erect/semierect position displaces gas-filled stomach or colon away from the pancreas.
If not possible, stomach distension with water also allows pancreatic visualization.
Causes: Most common are biliary tract calculi and alcohol abuse.
USG examination is more beneficial, 48 hours after the acute episode as the paralytic ileus resolves.
• Focal and hypoechoic enlargement of pancreas, usually head.
• Difficult to differentiate from neoplasm. Consider clinical severity and amylase/lipase correlation for acute pancreatitis.
• Gradually tapering CBD.
• Usually seen in chronic alcoholics, but may also be caused due to adjacent inflammatory process such as penetrating peptic ulcer.
• Diffusely hypoechoic parenchyma and certain inhomogenities with increasing severity.
• Pancreatic duct may appear dilated.
• Normal on USG with abnormal clinical and laboratory findings.
• Reduced echogenicity and increasing size (due to edema and inflammation) are observed as the condition worsens (Figure 6.2).
Extrapancreatic manifestations:
1. Fluid collections in lesser sac, anterior pararenal space, and so on.
Seen within 4 weeks from the onset of an acute attack with high incidence of spontaneous regression.
Can be treated conservatively with serial sonography scans.
2. Ascites.
3. Thickened edematous gallbladder (GB) wall.
4. Pleural effusion (left sided).
1. Pancreatic pseudocysts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree