KEY FACTS
Terminology
- •
Collection of pancreatic fluid and inflammatory exudate encapsulated by nonepithelial fibrous tissue developing > 4 weeks after acute pancreatic fluid collection
Imaging
- •
2/3 are peripancreatic: Body and tail (85%)
- •
Uncomplicated pseudocyst: Well-defined, unilocular, peripancreatic cystic mass in setting of prior pancreatitis
- ○
Smooth-walled, posterior acoustic enhancement
- ○
1/3 extrapancreatic
- ○
In addition to peripancreatic space, other locations, such as peritoneal space, intraabdominal parenchyma, and intrathoracic cavity, should also be evaluated
- ○
- •
Complex pseudocysts: Fluid-debris level, internal echoes, or septations (due to hemorrhage/infection); multilocular
- •
Develops over 4-6 weeks from acute pancreatic fluid collection
- •
CT best to evaluate extent of pseudocyst and complications
- ○
Gas within pseudocyst: Infection vs. decompression into stomach or bowel
- ○
- •
MRCP helpful to visualize communication with pancreatic duct
- •
Dilated pancreatic duct and common bile duct
- •
Wall calcification
- •
Absence of internal blood flow
- •
Endoscopic ultrasound may be required for aspiration and histologic diagnosis
Top Differential Diagnoses
- •
Mucinous or serous cystic neoplasm
- •
Intraductal papillary mucinous neoplasm
- •
Cystic islet cell tumor
- •
Choledochal cyst
- •
True epithelial cysts
Pathology
- •
Collection of fluid, tissue, debris, pancreatic enzymes, and blood covered by thin rim of fibrous capsule
Clinical Issues
- •
Associated with acute or chronic pancreatitis; alcoholism, cholelithiasis/choledocholithiasis
- •
Chronic alcoholism (75%)
- •
Clinical significance is related to size and complications; however, may be asymptomatic
- •
Abdominal pain, typically radiating to back; palpable tender mass
- •
Complications: More common in pseudocysts > 4-5 cm
- ○
Spontaneous rupture into peritoneal cavity
- ○
Erosion into adjacent vessel causing pseudoaneurysm or hemorrhage
- ○
Compression of adjacent bowel or bile duct
- ○
Fistula to stomach or bowel
- ○
- •
Spontaneous resolution in 25-40% of patients
- •
Rupture and hemorrhage are prime causes of death from pseudocyst
- •
Conservative therapy if asymptomatic or decreasing in size
- •
Percutaneous drainage required when symptomatic or enlarging
- ○
Curative in 90% of cases
- ○
Scanning Tips
- •
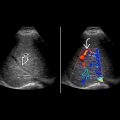
Turn on color Doppler to look for pseudoaneurysm or active bleeding in pseudocyst
 in the pancreatic body consistent with a pancreatic pseudocyst. The adjacent pancreatic duct is not compressed or displaced.
in the pancreatic body consistent with a pancreatic pseudocyst. The adjacent pancreatic duct is not compressed or displaced.
 . Posterior acoustic enhancement
. Posterior acoustic enhancement  is noted. The spleen
is noted. The spleen  provides an acoustic window.
provides an acoustic window.
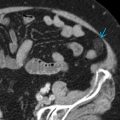
 . There is posterior acoustic enhancement
. There is posterior acoustic enhancement  . Calcification in the wall
. Calcification in the wall  is a sign of chronic pancreatitis.
is a sign of chronic pancreatitis.