Part 1 Hepatobiliary
Case 1

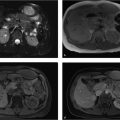
Key Finding
Liver mass with peripheral nodular enhancement.
Top 3 Differential Diagnoses
Hemangioma: Hemangiomas are the most common benign lesion with incidence reported as high as 20% in the general population. The classic imaging findings are initial progressive peripheral nodular enhancement in the arterial phase which on delayed imaging becomes isodense to the surrounding liver parenchyma. On MRI, hemangiomas are hyperintense on T2 (light bulb sign) and hypointense on T1-weighted imaging with similar enhancement patterns as seen with CT. On ultrasound, most hemangiomas are well circumscribed hyperechoic lesions.
Focal nodular hyperplasia (FNH): FNH is an uncommon hepatic lesion with a 5% incidence in the general population. The lesion is composed of hepatocytes and classically contains a central low-density scar. On MRI, FNH is intermediate to low signal on T2 with a bright central scar. Since FNH is composed of hepatocytes, it demonstrates enhancement on delayed intracellular imaging (with gadoxetate disodium), which is helpful in distinguishing FNH from other hepatic lesions.
Hepatic adenoma: Hepatic adenomas are benign lesions predominantly seen in women (90%). Most often they are solitary but may occasionally be multiple, especially in patients with glycogen storage disease. There is an association with oral contraceptive use. Hepatic adenomas have a variable contrast enhancement pattern. Adenomas are typically hypervascular; internal hemorrhage can lead to heterogeneity. The minority of cases may have macroscopic fat and calcifications.
Additional Diagnostic Considerations
Hepatocellular carcinoma (HCC): HCC is the most common visceral malignancy in the world. The most common etiology is cirrhosis. The lesions are typically hypodense and demonstrate increased arterial phase enhancement due to blood supply from the hepatic artery. Portal or hepatic vein invasion is common. MRI can be helpful in these instances since HCC typically displays increased T2 signal intensity. Clinically, HCC is associated with elevated alpha-fetoprotein (poor prognosis with average survival time of 6 months).
Metastases: Metastases are usually multiple but may present as a solitary lesion. Tumors that classically metastasize to liver commonly include lung, breast, melanoma, colon, and pancreas. On contrasted-enhanced imaging, metastases have a variable appearance.
Diagnosis
Hemangioma.
✓ Pearls
Hemangiomas demonstrate peripheral, nodular, enhancement, which becomes isodense to liver.
A hepatic lesion with portal or hepatic vein invasion is HCC until proven otherwise.
Hepatic adenomas are associated with oral contraceptives.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Kamel IR, Lawler LP, Fishman EK. Comprehensive analysis of hypervascular liver lesions using 16-MDCT and advanced image processing. AJR Am J Roentgenol. 2004; 183(2):443–452 Saenz RC. MRI of benign liver lesions and metastatic disease characterization with gadoxetate disodium. J Am Osteopath Coll Radiol. 2012; 1(4):2–9Case 2

Key Finding
Calcific density in the right upper quadrant.
Top 3 Differential Diagnoses
Gallbladder calcification: Gallstones are a common cause of right upper quadrant calcification, despite the fact that only a minority contain enough calcium making them visible on X-ray. The “Mercedes-Benz” sign is an additional radiographic indicator of cholelithiasis caused by nitrogen gas collecting in degenerating gallstones. Porcelain gallbladder is an additional consideration as it represents gallbladder wall calcification. Recent studies have shown a much weaker association between porcelain gallbladder and gallbladder carcinoma than traditionally thought.
Renal calcification: Numerous etiologies are possible for renal calcification, with nephrolithiasis being the most common. Most renal calculi are predominantly composed of calcium and demonstrate uniform opacity. Clustered, diffuse, mottled, or thin rim-like renal calcification can be seen in medullary and cortical nephrocalcinosis. Additionally, approximately 10% of renal cell carcinomas (RCCs) contain calcification, typically in an amorphous pattern.
Hepatic calcification: The etiologies of liver calcification are numerous. The most common etiology is calcified granuloma, which can form as a result of numerous infections, most commonly histoplasmosis. These often appear as multiple punctate, solid calcifications. Punctate calcification involving the spleen and/or lungs in addition to the liver is highly suggestive of granulomatous disease. Certain malignant neoplasms can also calcify, especially metastasis from mucinous adenocarcinomas of the colon, breast, stomach, or ovary. These calcifications tend to be faint and amorphous rather than dense.
Additional Diagnostic Considerations
Adrenal calcification: The most common cause of adrenal calcification is prior adrenal hemorrhage, which is more common in neonates than in adults and can appear as amorphous paraspinal calcification. Calcifications are typically seen greater or equal to 1 year after hemorrhage in adults and within 1 to 2 weeks in neonates.
Diagnosis
Cholelithiasis.
✓ Pearls
Cholelithiasis is the most common cause of right upper quadrant calcifications.
Nephrolithiasis is the most common cause of renal calcification.
Subcentimeter calcifications involving the liver, spleen, and/or lungs are highly suggestive of old healed granulomatous disease.
Suggested Readings
Bortoff GA, Chen MYM, Ott DJ, Wolfman NT, Routh WD. Gallbladder stones: imaging and intervention. Radiographics. 2000; 20(3):751–766 Dyer RB, Chen MY, Zagoria RJ. Abnormal calcifications in the urinary tract. Radiographics. 1998; 18(6):1405–1424 Stoupis C, Taylor HM, Paley MR, et al. The Rocky liver: radiologic-pathologic correlation of calcified hepatic masses. Radiographics. 1998; 18(3):675–685, quiz 726Case 3

Key Finding
Hepatic lesion with capsular retraction.
Top 3 Differential Diagnoses
Metastases: Metastasis is the most common tumor and malignancy of the liver. The most common source of metastatic disease is melanoma, lung, breast, pancreas, and colon carcinomas. Hepatic metastases on dynamic cross-sectional imaging most commonly show enhancement on the early arterial phase. Imaging findings depend on the primary tumor type, but lesions are often poorly circumscribed with variable enhancement and are usually multiple. Remember, the liver is the most common organ site for metastatic disease.
Hepatocellular carcinoma (HCC): HCC is the most common primary hepatic malignancy. The key imaging features include its characteristic dynamic enhancement pattern (early arterial phase enhancement with washout on delayed imaging) and a tumor capsule. The capsule is best seen on the portal venous and delayed images. MRI has a high accuracy of identifying an HCC capsule. Clinical correlation with serum alpha-fetoprotein levels may be helpful and should be elevated.
Cholangiocarcinoma: Cholangiocarcinoma is a rare cancer of the bile ducts. Cholangiocarcinomas are typically infiltrative lesions with segmental peripheral intrahepatic bile duct dilation. These tumors are the second most common primary hepatic malignancy. On dynamic CT, the majority of cases does not demonstrate any significant arterial enhancement and show delayed maximum enhancement (beyond 10 minutes), which is a key distinguishing feature. The lesion commonly is seen in the left lobe of the liver. Cholangiocarcinoma has a poor prognosis and less than 20% are resectable.
Additional Diagnostic Considerations
Hepatic lymphoma: Hepatic lymphoma may be primary or secondary. Secondary hepatic lymphoma is seen in greater than 50% of all lymphoma patients. Most lesions are lobulated in appearance and are multiple in number. Non-Hodgkin’s lymphoma (NHL) is more common to have hepatic involvement than Hodgkin.
Diagnosis
Metastasis from breast carcinoma.
✓ Pearls
A hepatic lesion with capsular retraction should be considered malignant until proven otherwise.
HCC will achieve maximum enhancement in the arterial phase, and cholangiocarcinoma has maximum enhancement on delayed imaging.
Cholangiocarcinoma is the only liver lesion that is more common in the left lobe.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Saenz RC. MRI of benign liver lesions and metastatic disease characterization with gadoxetate disodium. J Am Osteopath Coll Radiol. 2012; 1(4):2–9 Tang A, Bashir MR, Corwin MT, et al. LI-RADS Evidence Working Group. Evidence supporting LI-RADS major features for CT- and MR imaging-based diagnosis of hepatocellular carcinoma: a systematic review. Radiology. 2018; 286(1):29–48Case 4

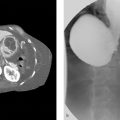
Clinical History
A 54-year-old male with acute right upper quadrant pain and elevated total bilirubin (▶Fig. 4.1).
Key Finding
Common bile duct dilation.
Top 3 Differential Diagnoses
Choledocholithiasis: Obstructing biliary stones are a common cause of a dilated common bile duct and occur in about 10% of patients with gallstones. Magnetic resonance cholangiopancreatography (MRCP) is very sensitive for their detection and stones will appear as one or more low-signal filling defects with angular margins and surrounding high-signal bile with associated ductal dilation. The central or segmental bile ducts may be involved in isolation or there can be dilation of the whole biliary tree. Chronic choledocholithiasis can result in biliary strictures, which will appear as smooth symmetric short segment narrowing of the duct either superior or inferior to the calculi on MRCP. Patients are at risk of developing cholangitis and cholestasis.
Strictures: Biliary strictures are classified as either benign or malignant. The features of benign strictures (causes include iatrogenic, pancreatitis, and inflammatory conditions) are smooth margins, symmetric tapering, and are typically short segment with or without duct dilation on MRCP. In contrast, malignant strictures (caused by tumor) are longer in length, asymmetric, and demonstrate abnormal irregular luminal shouldering.
Neoplasm: Tumors such as cholangiocarcinoma, pancreatic adenocarcinoma, gallbladder malignancies, and metastasis may invade the biliary system. These tumors can result in focal narrowing of the common bile duct and poststenotic dilation. Malignant strictures involving the common bile duct create an abrupt caliber change with intraluminal shouldering and eccentric asymmetry, which is often present at the transition point between the dilated obstructed duct and the smaller caliber decompressed duct. Extrinsic compression from malignant masses, lymphadenopathy, or dilated collateral vasculature may also produce poststenotic ductal dilation.
Additional Diagnostic Considerations
Choledochol cyst: A type 1 choledochol cyst is defined by dilation of the common bile duct. This can be seen in isolation or with concomitant dilation of the common hepatic duct. The common bile duct may be focally enlarged distally or can be enlarged in a fusiform morphology. These lesions will demonstrate bile-type signal on MRCP and MR studies.
Papillary stenosis: Defined as obstruction of bile flow at the sphincter of Oddi without the presence of a mass or inflammation at the ampulla, papillary stenosis appears as common bile duct dilation on MRCP. The most common cause is dysfunction of the sphincter of Oddi and patients typically present clinically with jaundice and pancreatitis. Papillary size less than 12 mm suggests an underlying benign cause. Endoscopic retrograde cholangiopancreatography (ERCP) is useful in determining the cause.
Diagnosis
Choledocholithiasis.
✓ Pearls
Choledocholithiasis appears as a filling defect with a dilated common bile duct.
Benign strictures are typically short with smooth tapering, and malignant strictures are characteristically long with irregular luminal shouldering and asymmetry.
Neoplasm may present with poststenotic common bile duct dilation as the mass narrows the duct from direct invasion or from extrinsic compression from tumor, lymphadenopathy, or enlarged collateral vessels.
Suggested Readings
Nikolaidis P, Hammond NA, Day K, et al. Imaging features of benign and malignant ampullary and periampullary lesions. Radiographics. 2014; 34(3):624–641 O’Connor OJ, O’Neill S, Maher MM. Imaging of biliary tract disease. AJR Am J Roentgenol. 2011; 197(4):W551–8 Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics. 2009; 29(6):1669–1688Case 5

Key Finding
Geographic liver lesion.
Top 3 Differential Diagnoses
Steatosis: Hepatic steatosis also known as fatty liver is due to the accumulation of triglycerides in the hepatocytes. The etiology may be from alcoholic or non-alcoholic liver disease (nonalcoholic steatohepatitis, NASH). Steatosis has many appearances including: diffuse, diffuse with sparring, focal, multifocal, and geographic. The focal form is less common. A key imaging feature is noting normal vessels coursing through the lesion. On CT, the diagnosis can be made by noting Hous-field Units (HU) less than 40 on non-contrast imaging or HU 20 less than splenic parenchyma on portal venous phase.
Metastases: Metastasis is the most common lesion of the liver. The most common appearance of hepatic metastases on CT is a low-density lesion with respect to the liver parenchyma. Imaging findings depend upon the primary tumor type, but lesions are often poorly circumscribed with variable enhancement and typically multiple. Metastasis is more than 10 times more common than primary liver malignancies. The liver is the most common organ site for metastatic disease.
Hepatic infarction: Hepatic infarcts are not common due to the dual blood supply of the liver. Etiologies include postsurgical ligation, vasculitis, blunt trauma, hypercoagulable states, and rare infections. Hepatic artery occlusion is more common than portal vein thrombosis. The most reliable finding is wedge shaped nonenhancement on all phases of a dynamic study. Angiography may be necessary to confirm hepatic artery occlusion. Treatment includes revascularization and transplantation.
Additional Diagnostic Considerations
Hepatic lymphoma: Hepatic lymphoma is known as the great mimicker. Although most often it is lobulated and multiple, it could also appear geographic in appearance. Non-Hodgkin’s lymphoma (NHL) is more common to have hepatic involvement than Hodgkin.
Laceration: On CT, a laceration is usually a linear and of low attenuation on postcontrast images. Advanced lacerations are large and may appear geographic in shape and are associated with hemoperitoneum. Imaging needs to be done in dual phase manner with delayed imaging in order to exclude vascular extravasation. Grading of injuries is done utilizing AAST (American Association for Surgical Trauma) scale. Treatment for patients with vascular extravasation who are unstable needs surgical intervention.
Diagnosis
Focal fatty infiltration.
✓ Pearls
The key to diagnose focal fatty infiltration is noting normal vessels coursing through the lesion.
Advanced AAST grades V to VI liver injuries are usually surgical.
Consider infarct in a postsurgical patient.
Suggested Readings
Coast, et al. Fat-containing liver lesions on imaging: detection and differential diagnosis. Am J Roentgen. 2018; 210:1–10 Federle MP, Jeffrey RB, Woodward PJ, Borhani A, et al. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2009 Saenz RC. MRI of benign liver lesions and metastatic disease characterization with gadoxetate disodium. J Am Osteopath Coll Radiol. 2012; 1(4):2–9Case 6

Key Finding
Gallbladder wall thickening.
Top 3 Differential Diagnoses
Acute cholecystitis: Most frequent inflammatory condition of the gallbladder. Cholecystitis is suspected on CT when a thick-walled gallbladder and fat stranding are seen. However, this is not pathognomonic and should be confirmed on ultrasound. Additional signs should include obstructing gallstone, hydropic dilatation of the gallbladder, pericholecystic fluid, and positive sonographic Murphy sign (most reliable).
Chronic cholecystitis: It is caused by gallbladder stones that create transient obstruction which leads to prolonged inflammation and fibrosis. This fibrosis may lead to a contracted gallbladder, and is almost always seen with cholelithiasis. Imaging findings include gallstones in thick-walled gallbladder with no pericholecystic fluid and lack of wall hyperemia.
Gallbladder carcinoma: More than 90% are adenocarcinomas with a 5-year survival rate of less than 5%. This entity can appear as a mass replacing the gallbladder, an intraluminal polypoid mass, or wall thickening that is focal or diffuse. Most gallbladder carcinomas present after 65. CT and MR are useful in defining extent of disease, adenopathy, and evaluating for metastasis.
Additional Diagnostic Considerations
Adenomyomatosis: Idiopathic, benign condition that has excessive proliferation of surface epithelium within dilated Rokitansky–Aschoff sinuses deep into the muscular wall. The most common findings are nonspecific wall thickening (focal, segmental, or diffuse), sludge, and calculi. The most common form is focally in the fundus. CT is less specific than ultrasound for detection, but it may show cystic-appearing thickening of the gallbladder wall or enhancing epithelium within intramural diverticula surrounded by relatively unenhanced hypertrophied gallbladder muscularis.
Systemic disease: Heart, renal, and liver failure may cause gallbladder wall thickening in the absence of inflammation. This may be related to elevated portal venous pressure, low intravascular osmotic pressure, hypoalbuminemia, and sepsis. Wall thickening may be pronounced (> 10 mm).
Diagnosis
Acute cholecystitis.
✓ Pearls
Gallbladder wall thickening greater than 3 mm is abnormal.
On CT when acute cholecystitis is suspected it should be confirmed on ultrasound.
The most common sites of metastasis for gallbladder carcinoma are the liver and peritoneum.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Runner GJ, Corwin MT, Siewert B, Eisenberg RL. Gallbladder wall thickening. AJR Am J Roentgenol. 2014; 202(1):W1–W12 van Breda Vriesman AC, Engelbrecht MR, Smithuis RH, Puylaert JB. Diffuse gallbladder wall thickening: differential diagnosis. AJR Am J Roentgenol. 2007; 188(2):495–501Case 7

Key Finding
Solitary, nonenhancing liver lesion.
Top 3 Differential Diagnoses
Hepatic cyst: Hepatic cysts are thought to be congenital lesions arising from developmental defects of the biliary ducts. They are well circumscribed with very thin or imperceptible walls. These are benign lesions and are more commonly seen in women. When cysts are innumerable, these may be associated with autosomal dominant polycystic kidney disease (ADPKD) or tuberous sclerosis. Simple cysts do not enhance.
Hepatic abscesses: Hepatic abscesses are uncommon and can be categorized into pyogenic (80%), amebic (10%), and fungal (10%). Pyogenic hepatic abscesses, being the most common, are found in the setting of diverticulitis and sepsis. Amebic abscesses are prone to rupture. Imaging findings include thick-walled, hypoattenuating liver masses with internal septations, peripheral lesion enhancement, and gas in up to 20% of cases. Pyogenic abscesses are commonly multilocular. Untreated, liver abscesses have a high mortality rate.
Biliary hamartoma: Biliary hamartomas are uncommon, benign, congenital malformations of the biliary tract. These are classically multiple (may be solitary), fluid attenuated, and measure less than 1.5 cm. There is no gender bias and these are asymptomatic, not requiring any treatment. The lesions typically do not enhance but if associated with solid components may enhance or show thin wall enhancement. These are also known as von Meyenburg complexes.
Additional Diagnostic Considerations
Biliary cystadenoma: Biliary cystadenomas are uncommon, multilocular, well-defined cystic masses arising from the bile ducts which are premalignant. They typically occur in middle-aged women who complain of chronic abdominal pain. The cyst wall may enhance. Malignant transformation to cystadenocarcinoma can occur.
Metastases: Metastasis is the most common lesion of the liver. The most common appearance of hepatic metastases on CT is a low-density lesion with respect to the liver parenchyma. Imaging findings depend on the primary tumor type, but lesions are often poorly circumscribed with variable enhancement and typically multiple. Metastasis is more than 10 times more common than primary liver malignancies. The liver is the most common organ site for metastatic disease.
Diagnosis
Hepatic cyst.
✓ Pearls
The key to diagnose hepatic cysts is confirming nonenhancement.
Hepatic cysts follow fluid on all MRI sequences.
Consider abscess with septic patients with a multilocular foci.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001; 21(4):895–910 Saenz RC. MRI of benign liver lesions and metastatic disease characterization with gadoxetate disodium. J Am Osteopath Coll Radiol. 2012; 1(4):2–9Case 8

Key Finding
Gallbladder mass.
Top 3 Differential Diagnoses
Cholelithiasis: Gallstones commonly present with right upper quadrant discomfort after a fatty meal in women in their 40s. It is the most commonly encountered gallbladder mass. Ultrasound is the best modality for detecting gallstones. Calcified gallstones appear hyperattenuated on CT, while pure cholesterol stones are hypoattenuating on CT. Isodense stones may be missed on CT. Treatment of choletlithiasis may be conservative if asymptomatic. Surgical removal of the gallbladder may be necessary if symptomatic.
Gallbladder polyp: These are nonmobile masses protruding from the gallbladder wall that may simulate focal wall thickening. These can be polypoid or sessile. The majority of polyps less than 10 mm are benign (>90%). CT is useful for staging larger polyps where there is an increased risk of malignancy. Polyps greater than 10 mm warrant resection. These are classified into adenoma, adenocarcinoma, cholesterol polyps, and inflammatory polyps.
Gallbladder carcinoma: There are several different imaging appearances. It can appear as a mass completely replacing the gallbladder which is most common. There can be focal or diffuse gallbladder wall thickening. Additionally, it can present as an intraluminal polypoid mass. Typically hypodense on venous phase. Calcified gallstones or porcelain gallbladder may be present.
Additional Diagnostic Considerations
Adenomyomatosis: Results in diffuse or focal thickening of the muscular wall of the gallbladder. There will be cystic nonenhancing spaces within gallbladder wall reflecting intramural diverticula. Deposition of cholesterol crystals into mucosal diverticula called Rokitansky–Aschoff sinuses. This a benign finding that is incidentally discovered. Contrast-enhanced CT is limited in the evaluation of adenomyomatosis.
Tumefactive sludge: Usually a result of biliary stasis from prolonged fasting or hyperalimentation. Most biliary sludge presents as a layering in the dependent gallbladder. Tumefactive sludge presents as an intraluminal polypoid mass that can mimic a tumor (> 25 HU). It should not enhance; however, vicarious excretion of iodinated contrast may confuse evaluation.
Diagnosis
Gallbladder adenocarcinoma.
✓ Pearls
Gallstones may contain nitrogen gas centrally which is called the “Mercedes-Benz” sign.
Size is most important predictor of malignancy with gallbladder polyps.
Increased risk of gallbladder carcinoma in patients with porcelain gallbladder.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Furlan A, Ferris JV, Hosseinzadeh K, Borhani AA. Gallbladder carcinoma update: multimodality imaging evaluation, staging, and treatment options. AJR Am J Roentgenol. 2008; 191(5):1440–1447 McKnight T, Patel A. Gallbladder masses: multimodality approach to differential diagnosis. J Am Osteopath Coll Radiol. 2012; 1(4):22–31Case 9

Key Finding
Liver mass with a central scar.
Top 3 Differential Diagnoses
Hemangioma: Hemangiomas are the most common benign hepatic lesion. The classic imaging findings are initial discontinuous peripheral nodular enhancement in the arterial phase with delayed central filling. Smaller hemangiomas may demonstrate flash-filling during the arterial phase, while larger lesions may have central regions of fibrosis or cystic changes. On MRI, hemangiomas are hyperintense on T2 (light bulb sign) and hypointense on T1-weighted imaging with similar enhancement patterns as seen with CT. On ultrasound, most hemangiomas are well circumscribed hyperechoic lesions.
Focal nodular hyperplasia (FNH): FNH is an uncommon hepatic lesion that typically presents in young females (75%). The lesion is composed of hepatocytes and classically contains a central low-density scar. On arterial phase imaging, there is enhancement of the lesion with a low-density central scar, which fills in on delayed imaging. The central scar is hyperintense on T2-weighted MR imaging. Since FNH is composed of hepatocytes, it may demonstrate uptake of sulfur colloid (other hepatic lesions demonstrate cold defects) on scintigraphy, although this examination has been somewhat supplanted by MRI. Hepatocyte specific MR contrast agents with delayed imaging are less than 95% specific in distinguishing FNH from other hepatic lesions.
Hepatocellular carcinoma (HCC): HCC is the most common primary hepatic malignancy with an increased incidence in patients with chronic liver disease. Patients may present with a single lesion, multiple lesions, or diffuse hepatic involvement. The lesions are typically hypodense and demonstrate increased arterial phase enhancement due to blood supply from the hepatic artery. Portal or hepatic vein invasion is common. Diagnosis can be difficult in cirrhosis with regenerating nodules. MRI can be helpful in these instances since HCC typically displays increased T2 signal intensity. Clinically, HCC is associated with elevated alpha-fetoprotein.
Additional Diagnostic Considerations
Hepatic adenoma: Hepatic adenomas are benign lesions predominantly seen in women (90%). Most often they are solitary but may occasionally be multiple, especially in patients with glycogen storage disease. Hepatic adenomas have an increased frequency and risk of rupture with the use of oral contraceptives. Adenomas are typically hypervascular; internal hemorrhage can lead to heterogeneity.
Hypervascular metastases: Hypervascular metastases are usually multiple but may occasionally present as a solitary mass. Tumors that classically result in hypervascular metastases include melanoma, renal cell carcinoma (RCC), choriocarcinoma, thyroid, carcinoid, pancreatic islet cell tumors, and sarcomas.
Diagnosis
FNH.
✓ Pearls
FNH demonstrates variable enhancement with the scar being isoattenuated on delayed phase imaging.
A hypervascular hepatic lesion within a cirrhotic liver is HCC until proven otherwise.
Hepatic adenomas are associated with oral contraceptives and are prone to hemorrhage.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Kamel IR, Lawler LP, Fishman EK. Comprehensive analysis of hypervascular liver lesions using 16-MDCT and advanced image processing. AJR Am J Roentgenol. 2004; 183(2):443–452 Saenz RC. MRI of benign liver lesions and metastatic disease characterization with gadoxetate disodium. J Am Osteopath Coll Radiol. 2012; 1(4):2–9Case 10

Key Finding
Round focus in common bile duct.
Top 3 Differential Diagnoses
Choledocholithiasis: Choledocholithiasis is one of the most common indications for magnetic resonance cholangiopancreatography (MRCP) of the biliary system, which has a high sensitivity and specificity for their detection. The vast majority of common bile duct stones originate from the gallbladder. Both cholesterol and pigmented stones manifest as low signal on T2-weighted images, however their T1 characteristics can vary. Nondilated biliary ducts can be seen in up to one-third of patients with biliary stones. Therefore, a nondilated biliary tract should still be scrutinized for filling defects, as intermittent obstruction can occur.
Ascending cholangitis: The classical clinical presentation of ascending cholangitis includes fever, jaundice, and right upper quadrant pain (Charcot’s triad). Ascending cholangitis occurs in the setting of biliary obstruction, most commonly from choledocholithiasis/hepatolithiasis. There is resultant bile stasis with subsequent infection, typically ascending from the duodenum. Irregular, dilated bile ducts with wall enhancement and biliary obstruction are characteristic. Occasionally, low signal intensity biliary calculi can be seen on T2-weighted images.
Recurrent pyogenic cholangitis: Recurrent pyogenic cholangitis is endemic in Southeast Asia and has a strong association with parasitic infections of the bile ducts. The disease is characterized by recurrent attacks of bacterial cholangitis with associated biliary calculi (pigmented stones). Dilated bile ducts with intrahepatic biliary strictures and intraductal calculi are characteristic. Atrophy of the affected hepatic segment is commonly present.
Additional Diagnostic Considerations
Cholangiocarcinoma: Cholangiocarcinoma can be classified based on the anatomic location. Hilar (Klatskin tumor) is the most common and classically involves the biliary confluence. Extrahepatic cholangiocarcinoma involves the common hepatic or common bile duct and peripheral cholangiocarcinoma arises from intrahepatic bile ducts. The tumors characteristically demonstrate slow, progressively increasing enhancement that persists on delayed images. Proximal biliary ductal dilatation and abrupt biliary stricture/occlusion can be seen on MRCP.
Diagnosis
Choledocholithiasis.
✓ Pearls
Stones are characterized on T2 images as low signal intensity foci within the bile duct.
Ascending cholangitis occurs in the setting of biliary obstruction, most commonly from gallstones.
Suspect recurrent pyogenic cholangitis in the setting of bile duct dilatation/stones in Southeast Asian patients.
Suggested Readings
Catalano OA, Sahani DV, Forcione DG, et al. Biliary infections: spectrum of imaging findings and management. Radiographics. 2009; 29(7):2059–2080 Leyendecker JR, Brown JJ, Merkle EM. Practical Guide to Abdominal and Pelvic MRI, 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011 Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics. 2009; 29(6):1669–1688Case 11

Key Finding
Pneumobilia.
Top 3 Differential Diagnoses
Sphincter of Oddi dysfunction: Choledocholithiasis and patulous sphincter of Oddi are the most common causes of a dysfunctional sphincter of Oddi. Passage of gallstones through the sphincter of Oddi may cause incompetence of the sphincter and result in passage of bowel gas into the bile ducts. A patulous sphincter of Oddi is primarily seen in the elderly and typically the pneumobilia will be minimal.
Iatrogenic/postsurgical: Patients typically have a history of enteric or biliary intervention such as endoscopic retrograde cholangiopancreatography (ERCP) biliary-enteric anastomosis, or sphincterotomy. Biliary sphincterotomy and patent biliary stents are common surgical causes of pneumobilia. Incising the sphincter of Oddi during an ERCP for removal of gallstones, and/or placement of a stent enables bowel gas to pass through the stent or the postsurgical sphincter into the bile ducts.
Infection/inflammation: Emphysematous cholecystitis, most commonly in diabetic and the elderly, may reflux air into the bile ducts. Look for surrounding inflammatory changes.
Additional Diagnostic Considerations
Fistula: Gallstone ileus may cause the gallstone to erode through inflamed bile duct or gallbladder wall into the small bowel creating a cholecystoduodenal fistula. Extensive inflammatory changes are usually present.
Diagnosis
Pneumobilia post-sphincterotomy.
✓ Pearls
Pneumobilia can reflux into the gallbladder and mimic emphysematous cholecystitis.
Portal venous gas is along the periphery of the liver.
Occluded biliary stents do not allow passage of bowel gas into the bile ducts.
Suggested Readings
Catalano OA, Sahani DV, Forcione DG, et al. Biliary infections: spectrum of imaging findings and management. Radiographics. 2009; 29(7):2059–2080 Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Patel NB, Oto A, Thomas S. Multidetector CT of emergent biliary pathologic conditions. Radiographics. 2013; 33(7):1867–1888 Shah PA, Cunningham SC, Morgan TA, Daly BD. Hepatic gas: widening spectrum of causes detected at CT and US in the interventional era. Radiographics. 2011; 31(5):1403–1413Case 12

Key Finding
Gallbladder intraluminal air.
Top 3 Differential Diagnoses
Emphysematous cholecystitis: Emphysematous cholecystitis is a rare form of acute cholecystitis due to secondary infection by gas-forming organisms. The pathogenesis is thought to be secondary to vascular compromise of cystic artery. This is considered a surgical emergency. There is a high risk of gangrene, perforation, and sepsis if untreated. An urgent cholecystectomy is the definitive treatment. A cholecystostomy may be needed to bridge to cholecystectomy in high-risk poor surgical candidates. Emphysematous cholecystitis most commonly occurs in elderly or diabetic patients.
Sphincter of Oddi dysfunction: Incompetence of the sphincter of Oddi may result in passage of bowel gas into the bile ducts and into the gallbladder. This incompetence is caused by choledocholithiasis, senescent change, or a patulous sphincter. The sphincter may also be dysfunctional secondary to prior instrumentation (esophagogastroduodenoscopy, sphincteroplasty, or papillotomy).
Cholelithiasis: These may present with gas filled fissures. About 50% of gallstones have fissures, however less than half have gas. This triradiate pattern of nitrogen gas is called the “Mercedes-Benz sign.” This can be mistaken for emphysematous cholecystitis. The presence of air-filled gallstones does not imply infection.
Additional Diagnostic Considerations
Gangrenous cholecystitis: The most common complication of acute cholecystitis affecting 15% of patients. It occurs as a result of ischemia with necrosis of the gallbladder wall. CT signs include gallbladder wall or lumen gas, focal irregularity or defect in the gallbladder wall, intraluminal membranes, absence of mural enhancement, and pericholecystic abscess.
Fistula: There may be an abnormal connection between the bowel and the gallbladder. This connection allows air from the bowel to enter into the gallbladder. The cholecystocolonic fistula is uncommon, occurring in around 0.1% of patients with biliary disease. The cholecystoduodenal fistula is the most common type involving the gallbladder. A complication of cholecystocolonic fistula is perforation of the colon with resultant fecal peritonitis which can progress to sepsis or death.
Diagnosis
Sphincter of Oddi dysfunction secondary to a patulous sphincter.
✓ Pearls
Clostridium perfringens is the most common gas forming organism in emphysematous cholecystitis.
CT is the best modality for identifying intramural or intraluminal gas.
Portal venous gas may mimic biliary gas.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Grayson DE, Abbott RM, Levy AD, Sherman PM. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002; 22(3):543–561 Smith EA, Dillman JR, Elsayes KM, Menias CO, Bude RO. Cross-sectional imaging of acute and chronic gallbladder inflammatory disease. AJR Am J Roentgenol. 2009; 192(1):188–196Case 13

Key Finding
Target liver lesion.
Top 3 Differential Diagnoses
Metastases: Metastasis is the most common tumor and malignancy of the liver. The most common source of metastatic disease is melanoma, lung, breast, pancreas, and colon carcinomas. Metastatic lesions can have peripheral rim- or target-like enhancement. Imaging findings depend on the primary tumor type, but lesions are often poorly circumscribed with variable enhancement and typically multiple. Metastasis is more than 10 times more common than primary liver malignancies. The liver is the most common organ site for metastatic disease.
Hepatocellular carcinoma (HCC): HCC is the most common primary hepatic malignancy. Patients may present with multiple lesions. The lesions typically demonstrate increased arterial phase enhancement due to blood supply from the hepatic artery with washout of contrast on delayed imaging. MRI can be helpful in these instances since HCC typically displays increased T2 signal intensity. Clinically, HCC is associated with elevated alpha-fetoprotein.
Hepatic lymphoma: Hepatic lymphoma may be primary or secondary. Secondary hepatic lymphoma is seen in more than 50% of all lymphoma patients. Most lesions are lobulated in appearance and are multiple in number. Non-Hodgkin’s lymphoma (NHL) is more common to have hepatic involvement than Hodgkin.
Additional Diagnostic Considerations
Hepatic abscesses: Hepatic abscesses are uncommon and can be categorized into pyogenic (80%), amebic (10%), and fungal (10%). Pyogenic hepatic abscesses are the most common and found in the setting of diverticulitis and sepsis. Amebic abscesses are prone to rupture. Imaging findings include thick-walled, hypoattenuating liver masses with internal septations, peripheral lesion enhancement, and air in up to 20% of cases. Untreated, liver abscesses have a high mortality rate.
Diagnosis
Metastasis from breast carcinoma.
✓ Pearls
A hepatic lesion with a target enhancement should be considered metastatic until proven otherwise.
A hepatic metastatic target lesion is classically from breast or gastrointestinal adenocarcinoma.
HCC will have an elevated serum alpha-fetoprotein.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001; 21(4):895–910 Saenz RC. MRI of benign liver lesions and metastatic disease characterization with gadoxetate disodium. J Am Osteopath Coll Radiol. 2012; 1(4):2–9Case 14

Key Finding
Gallbladder wall thickening with cystic changes.
Top 3 Differential Diagnoses
Adenomyomatosis: It is also known as adenomyomatous hyperplasia or diverticulosis of the gallbladder. Adenomyomatosis is a benign condition with cholesterol deposition within dilated Rokitansky–Aschoff sinuses with associated wall thickening. The most common form is focally in the fundus. CT is less specific than ultrasound for detection, but it may show cystic-appearing thickening of the gallbladder wall or enhancing epithelium within intramural diverticula surrounded by relatively unenhanced hypertrophied gallbladder muscularis. On MRI, the intramural diverticula may be seen as high T2 signal foci in line mimicking a “pearl necklace.”
Acute cholecystitis: Most frequent inflammatory condition of the gallbladder. Cholecystitis is suspected on CT when a thick-walled gallbladder and fat stranding are seen. However, this is not pathognomonic and should be confirmed on ultrasound or nuclear hepatobiliary scan. On ultrasound, the most reliable sign is a positive sonographic Murphy sign (pain when the sonographer pushes on the gallbladder while imaging).
Chronic cholecystitis: It is caused by gallbladder stones that create transient obstruction which leads to prolonged inflammation and fibrosis. This fibrosis may lead to a contracted gallbladder, and is almost always seen with cholelithiasis. Imaging findings include gallstones in thick-walled gallbladder with no pericholecystic fluid and lack of wall hyperemia.
Additional Diagnostic Considerations
Gallbladder carcinoma: The majority are adenocarcinomas with the second most common being squamous cell. This entity can appear as a mass replacing the gallbladder, an intraluminal polypoid mass, or wall thickening that is focal or diffuse. Most gallbladder carcinomas present after 65. CT and MR are useful in defining extent of disease, adenopathy, and evaluating for metastasis.
Diagnosis
Adenomyomatosis.
✓ Pearls
Adenomyomatosis is a benign condition.
Adenomyomatosis is seen in up to 25% of cholecystectomy specimens.
On CT when acute cholecystitis is suspected it should be confirmed with ultrasound or nuclear.
Suggested Readings
Federle MP, Jeffrey RB, Woodward PJ, Borhani A. Diagnostic Imaging: Abdomen. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009 McKnight T, Patel A. Gallbladder masses: multimodality approach to differential diagnosis. J Am Osteopath Coll Radiol. 2012; 1(4):22–31 Runner GJ, Corwin MT, Siewert B, Eisenberg RL. Gallbladder wall thickening. AJR Am J Roentgenol. 2014; 202(1):W1–W12Case 15

Clinical History
A 67-year-old woman with chronic liver enzyme elevation and a history of breast cancer (▶Fig. 15.1).
Key Finding
Nodular liver contour.
Top 3 Differential Diagnoses
Cirrhosis: Cirrhosis is a chronic liver disease characterized by hepatic fibrosis and regenerative hepatic nodules. Common causes include alcohol (micronodular cirrhosis), chronic viral hepatitis (macronodular cirrhosis), autoimmune hepatitis, and chronic metabolic conditions (primary biliary cirrhosis, primary hemochromatosis, Wilson’s disease, alpha-1 antitrypsin deficiency). Imaging findings include nodular liver surface contour, distorted hepatic architecture with atrophy, and stigmata of portal hypertension (enlarged main portal vein with slow flow, flow reversal or occlusion; varices, splenomegaly, gallbladder/bowel wall thickening, and ascites). MRI of liver nodules helps distinguish regenerative nodules (low T2 signal) from neoplastic nodules (high T2 signal). The use of gadoxetate disodium can help in distinguishing or characterizing hepatic lesions due to hepatocyte phase of imaging.
Treated metastases: Chemotherapy treatment of liver metastases (commonly from breast, lung, and colorectal cancer) can result in scarring of hepatic tumor implants. Liver parenchyma, between these areas of scarring, can be normal or regenerative. The overall imaging appearance simulates macronodular cirrhosis, and hence is referred to as “pseudocirrhosis.” Correlation with appropriate history is helpful.
Budd–Chiari syndrome: Chronic hepatic venous occlusive disease can result in a nodular liver contour, usually as a consequence of regenerative nodules. In chronic Budd–Chiari syndrome, these nodules are usually small, multiple, and hypervascular, and the number of nodules is often underestimated on CT. Large regenerative hypervascular nodules may be seen and are usually hyperintense on T1 MRI sequences. There is no evidence that large regenerative nodules degenerate into malignancy. A central scar in nodules greater than 1 cm can be seen. Caudate hypertrophy occurs as a result of its separate venous drainage into the inferior vena cava (IVC), which may simulate a dominant nodule.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree