Part 2: Bone Tumors
Case 14

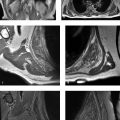
Key Finding
Aggressive periosteal reaction.
Top 3 Differential Diagnoses
Primary bone malignancies: Aggressive patterns of periosteal reaction are seen with osteosarcoma, Ewing’s sarcoma, and chondrosarcoma. High-grade conventional intramedullary osteosarcomas have rapid doubling times and tend to invade the cortex without expanding it. Codman’s triangle, lamellated or spiculated (hair-on-end and sunburst) patterns of periosteal reaction are seen. Codman’s triangle forms when a portion of the periosteum is lifted off the cortex by a lesion. In lamellated or onion skin pattern, multiple layers of new bone are formed concentrically around the cortex. Spicules of bone form perpendicular (hair-on-end) or radiate in a divergent pattern (sunburst) from the surface of bone in spiculated pattern. Ewing’s sarcomas also typically have aggressive periosteal reaction, with hair-on-end subtype being characteristic of them. In conventional chondrosarcoma, the cortex responds to maintain the lesion in the medullary canal, leading to cortical remodeling, thickening and periosteal reaction.
Hematologic malignancies: In leukemia, lamellated appearance is common with hair-on-end appearance being less frequent. Lymphoma can produce aggressive and disorganized periosteal reaction with associated soft tissue mass that is larger than the area of bone destruction.
Osteomyelitis: Various periosteal reaction patterns that can be seen with infection include disorganized, lamellated, and spiculated. In the acute phase, Codman triangle can also develop.
Additional Diagnostic Considerations
Benign bone tumors: Calvarial hemangiomas can present as lucent lesions with spiculated sunburst pattern. Enplaque meningiomas usually provoke hyperostosis with rough spiculated margins in adjacent sphenoid ridge. Aneurysmal bone cysts (ABC) can show shell type periosteal reaction; however, intracortical or subperiosteal forms of ABC can also show spiculated pattern.
Metastases: Prostatic osseous metastases can occasionally show sunburst-type reaction. Hypervascular lesions like renal cell metastases can be associated with shell-like pattern.
Diagnosis
Ewing’s sarcoma.
Pearls
Osteosarcoma and Ewing’s sarcoma are typically associated with various patterns of aggressive periosteal reaction.
Lymphoma can be associated with aggressive periosteal reaction and a soft-tissue mass that is larger than the area of bone destruction.
Osteomyelitis, especially in acute phase, can have aggressive periosteal reaction and other features, making it difficult to distinguish from a malignancy based on imaging. Clinical features, laboratory tests, and tissue sampling will help to distinguish.
Suggested Readings
- 45 Bisseret D, Kaci R, Lafage-Proust MH et al. Periosteum: characteristic imaging findings with emphasis on radiologic-pathologic comparisons.. Skeletal Radiol 2015; 44 (3) 321-338 PubMed 25269751
- 46 Rana RS, Wu JS, Eisenberg RL. Periosteal reaction.. AJR Am J Roentgenol 2009; 193 (4) W2597-12 PubMed 19770293
Case 15

Key Finding
Focal cortical thickening.
Top 3 Differential Diagnoses
Osteoid osteoma:Osteoid osteoma is a benign bone tumor usually seen in boys and men between 7 and 25 years of age. The appearance of an osteoid osteoma may vary according to its location. Cortical osteoid osteoma, the most common variety, typically demonstrates fusiform sclerotic thickening in the shaft of a long bone, especially the tibia and femur. A characteristic radiolucent nidus representing the lesion itself is located in the center of osteosclerosis. The reaction can be so dense that the central nidus may be masked on plain films. CT is more sensitive than radiography for detection of the nidus, which may be entirely radiolucent or contain variable amount of mineralization. The reactive periosteal bone is usually solid but may be laminated.
Stress fracture:Another common cause of focal cortical thickening or uninterrupted periosteal reaction is stress fracture. The periosteal reaction and endosteal thickening develop in an attempt to buttress the weakened cortex initially. As damage increases, a true fracture line may appear. These injuries typically involve the shaft of a long bone and are common in the posterior cortex of tibia in runners. In cases with atypical clinical and radiographic presentation, CT is excellent at demonstrating the presence of subtle lucent fracture lines and longitudinal fracture lines. The sclerosis associated with osteoid osteoma is usually much greater than the reactive change seen in stress fracture. A stress fracture is more likely than an osteoid osteoma if the size of the cortical lesion decreases during a short follow-up period. Bone scintigraphy can also help differentiate as a stress fractures demonstrates intense, linear uptake, whereas osteoid osteoma displays the “double density” sign, in which intense central uptake is seen at the nidus and moderate uptake is seen in the surrounding area.
Chronic osteomyelitis or intracortical abscess:Chronic osteomyelitis can also cause cortical thickening and a lucent lesion. At radiography, an intracortical abscess and an osteoid osteoma can be indistinguishable. However, it is easier to differentiate between the two on CT. In osteoid osteoma, the inner side of the nidus is smooth, and a round calcification is seen at the center of the nidus. In an intracortical abscess, the inner margin is irregular and the sequestrum is also irregular and eccentric. On CT, osseous tunneling is seen extending from the lucency, and presence of a soft-tissue abscess adjacent to the area of sclerosis can be seen with infection. On MR, the central part of the abscess does not enhance, whereas in osteoid osteoma, an unmineralized nidus of highly vascularized stroma enhances strongly.
Diagnosis
Osteoid osteoma.
Pearls
In osteoid osteomas, CT is more sensitive than radiography for detection of the central nidus.
CT is also excellent at demonstrating subtle lucent fracture lines in cases of stress fractures.
The central part of an intracortical abscess does not enhance, whereas the central nidus of an osteoid osteoma enhances avidly on MR.
Suggested Readings
- 47 Chai JW, Hong SH, Choi JY et al. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings.. Radiographics 2010; 30 (3) 737-749 PubMed 20462991
- 48 Datir AP. Stress-related bone injuries with emphasis on MRI.. Clin Radiol 2007; 62 (9) 828-836 PubMed 17662729
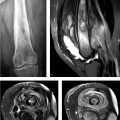
Case 16

Key Finding
Epiphyseal equivalent lucent lesion.
Top 3 Differential Diagnoses
Chondroblastoma: Chondroblastomas are rare lesions that occur in the epiphyses of long bones and are usually seen before skeletal maturity. Most common locations include the humerus, tibia, and femur, as well as within epiphyseal equivalents such as the patella. On radiographs, chondroblastomas tend to be well-defined lucent lesions with a thin rim of sclerosis; calcifications can be seen in approximately 50% of cases. Periosteal reaction can occasionally be seen quite a distance away from the primary lesion. On MRI, they tend to show decreased signal intensity on T1 and variable signal intensity on T2-weighted sequences, depending upon the amount of chondroid matrix and calcification. However, chondroblastomas are associated with significant surrounding marrow edema that may extend into the soft tissues. They demonstrate increased uptake on nuclear medicine bone scans.
Giant cell tumor (GCT): Giant cell tumors are locally aggressive bone tumors composed of giant cells, connective tissue, and stromal cells. They are most common in the third and fourth decades and more so in women than men. Its fundamental feature is extensive epiphyseal involvement and is usually seen after growth plate closure. GCT favors long tubular bones, but it can also be seen in the spine and flat bones such as the clavicles, ribs, and sternum. Radiographic evaluation shows a lucent, expansile, eccentric lesion, producing overlying cortical thinning. Margins can be well- or poorly defined. Approximately 5 to 10% of them may be malignant. They can also have recurrence after treatment.
Langerhans cell histiocytosis (LCH): LCH typically occurs in children, adolescents and young adults, and has a 2:1 male predominance. Although LCH can be multiple, solitary lytic bone lesions predominate with a punched-out appearance; it commonly involves the skull (“punched out” lesion with beveled edges), mandible (“floating tooth”), spine (flattened vertebral body or vertebra plana), ribs, and long bones. These lesions occur in the epiphyses and can cross an open growth plate. LCH can mimic more aggressive processes such as infection or Ewing sarcoma both clinically and radiographically.
Additional Diagnostic Consideration
Intraosseous ganglion cyst: These lesions tend to occur within the subchondral/subarticular regions of the shoulder, knee, ankle, hip, and carpal joints after skeletal maturation. On radiographs, they are well-defined lucent lesions with surrounding sclerotic margins. They demonstrate low-T1 and high-T2 signal intensity.
Diagnosis
Chondroblastoma.
Pearls
Chondroblastomas usually occur in epiphyses or epiphyseal equivalents before skeletal maturity.
Chondroblastomas tend to be associated with a significant amount of marrow and soft-tissue edema.
Giant cell tumors typically involve the epiphysis or epiphyseal equivalent only after skeletal maturity.
LCH can occur in the epiphysis and can cross the growth plate.
Suggested Readings
- 49 Douis H, Saifuddin A. The imaging of cartilaginous bone tumours. I. Benign lesions.. Skeletal Radiol 2012; 41 (10) 1195-1212 PubMed 22707094
- 50 Greenspan A, Jundt G, Remagen W. Differential Diagnosis in Orthopedic Oncology. 2nd ed. Lippincott Williams and Wilkins;2007
Case 17

Key Finding
Solitary focal sclerotic lesion.
Top 3 Differential Diagnoses
Bone island: An enostosis, or bone island, is a benign entity that represents a focus of mature compact (cortical bone) within the cancellous bone. Radiography reveals a usually homogeneously dense, sclerotic focus within cancellous bone with spiculated margins or brush borders. Most lesions are between 2 mm and 2 cm in size and often oriented with the long axis of the bone. A lesion larger than 2 cm is termed “giant bone island.” There is no destruction of cortex, soft-tissue mass or periosteal reaction. Their appearance is pathognomonic; however, if large in size, multiple, atypical in appearance, or in patients with history of a primary malignancy, they may need to be distinguished from other blastic lesions. On radionuclide imaging, they show no or occasionally low-grade activity.
Blastic metastasis: Metastatic disease is a common cause of a sclerotic lesion, most commonly caused by prostate cancer in men and breast cancer in women. When presented with a sclerotic lesion, helpful features to suggest malignant disease include the following: 1) lesion borders which tend to be indistinct with a wide zone of transition, 2) presence of periosteal reaction, 3) soft tissue extension, and 4) size, as metastatic lesions tend to be larger and less uniform than those seen in benign conditions. Most blastic metastatic lesions show increased radiotracer uptake on bone scan.
Melorheostosis: Melorheostosis (Leri disease) is a sporadic, sclerosing skeletal dysplasia that typically manifests in late childhood or early adulthood. It has a characteristic radiographic appearance consisting of cortical and medullary hyperostosis of a single bone or multiple adjacent bones. When a single bone is involved, the characteristic wavy appearance of hyperostosis that resembles melted wax dripping down the side of a candle, usually involving only one side of the bone, is helpful in making the diagnosis.
Additional Diagnostic Considerations
Low-grade intraosseous osteosarcoma: Low-grade intraosseous osteosarcoma is an unusual variant of conventional osteosarcoma. It occurs most frequently in patients in the third decade of life, but patients have a wide age range. The most commonly affected sites are metaphyses of the femur and tibia (about the knee). At radiologic examination, the lesion may show well-defined margins, sclerotic rim, prominent internal trabeculation, and diffuse sclerosis. However, radiologic evidence of a more aggressive process like focally indistinct margin, focal bone lysis, soft-tissue mass, and cortical destruction is apparent even if subtle.
Lymphoma: Sclerotic lesions are rare in primary bone lymphoma compared to metastatic bone lymphoma. Hodgkin disease of bone tends to be sclerotic, and even in Hodgkin disease, lytic lesions predominate.
Diagnosis
Giant bone island.
Pearls
A bone island typically appears as a small, homogeneously sclerotic lesion within cancellous bone with spiculated margins.
Blastic metastatic disease is commonly caused by prostate cancer in men and breast cancer in women.
Melorheostosis has a characteristic “dripping candle wax” appearance of hyperostosis.
Suggested Readings
- 52 Ihde LL, Forrester DM, Gottsegen CJ et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis.. Radiographics 2011; 31 (7) 1865-1882 PubMed 22084176
Case 18

Key Finding
Lesion with permeative or moth-eaten pattern.
Top 3 Differential Diagnoses
Multiple myeloma: Multiple myeloma is a neoplastic monoclonal gammopathy that usually affects the axial skeleton and proximal portions of humerus and femur. The hallmark is detection of monoclonal protein in blood and/or urine. It can present as a solitary lesion, diffuse skeletal myelomatosis, diffuse osteopenia, and sclerosing myeloma. Diffuse osteopenia can change to more permeative destructive pattern.
Lymphoma: Primary bone lymphoma occurs in a broad range of patients, from pediatric to elderly, with peak incidence in the sixth and seventh decades. Femur is the most common site. The most common radiographic appearance of primary bone lymphoma is permeative or moth-eaten pattern of lytic destruction. Secondary osseous lymphoma can present similarly.
Ewing’s sarcoma: Ewing’s sarcoma is the second most common malignant bone tumor in children and adolescents. The most common sites are femur, ilium, and tibia. Bone destruction with moth-eaten to permeative pattern is seen in 76 to 82% of lesions with associated, often large, soft-tissue mass. Continuity between intraosseous and extraosseous components may be through large areas of cortical destruction or subtle channels through cortex.
Additional Diagnostic Considerations
Metastases: Metastatic lesions can present as permeative or moth-eaten pattern of destruction. A history of known primary malignancy and multiplicity of lesions can help in making the diagnosis.
Infection: Acute aggressive osteomyelitis can present with this pattern and be indistinguishable from a malignant lesion. Tissue sampling will be confirmatory, as even clinical picture can sometimes be confusing.
Diagnosis
Lymphoma.
Pearls
Permeative or moth-eaten pattern of bone destruction is indicative of an aggressive process.
Multiple myeloma can present in a variety of forms. Serum and urine presence of monoclonal M protein is the hallmark.
Round cell tumors such as lymphoma and Ewing’s sarcoma can have relatively little cortical destruction in the presence of extensive marrow involvement and soft-tissue component.
Suggested Readings
- 54 Angtuaco EJ, Fassas AB, Walker R, Sethi R, Barlogie B. Multiple myeloma: clinical review and diagnostic imaging.. Radiology 2004; 231 (1) 11-23D PubMed 14990813
- 55 Krishnan A, Shirkhoda A, Tehranzadeh J, Armin AR, Irwin R, Les K. Primary bone lymphoma: radiographic-MR imaging correlation.. Radiographics 2003; 23 (6) 1371-1383 PubMed 14615550
- 56 Murphey MD, Senchak LT, Mambalam PK, Logie CI, Klassen-Fischer MK, Kransdorf MJ. From the radiologic pathology archives: ewing sarcoma family of tumors: radiologic-pathologic correlation.. Radiographics 2013; 33 (3) 803-831 23674776
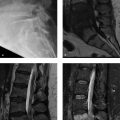
Case 19

Key Finding
Osseous lesion with fluid–fluid levels.
Top 3 Differential Diagnoses
Aneurysmal bone cyst: An aneurysmal bone cyst (ABC) is an expansile bone lesion containing multiple, thin-walled, blood-filled cystic cavities. Most of the ABCs are found in patients from 5 to 20 years of age. Typical sites include metaphyses of long bones and posterior elements of the spine. Fluid–fluid levels occur whenever substances of different densities are contained within a cystic or compartmentalized structure. Fluid–fluid levels can be seen in ABCs with CT or MRI and are believed to represent sedimentation of red blood cells within the cystic cavities.
Simple bone cyst:A simple bone cyst (SBC) or unicameral bone cyst (UBC) is a benign fluid-containing lesion that usually arises in the metaphyses of long bones. Proximal humerus and proximal femur are the most common sites. Majority of these lesions are seen in patients who are less than 20 years of age. On imaging, it is seen as a mildly expansile lesion, which has a narrow zone of transition with a thin sclerotic rim and no tumor matrix. It is often found incidentally or as a pathologic fracture. Fluid–fluid levels can be seen in SBCs usually associated with a pathologic fracture.
Telangiectatic osteosarcoma:Telangiectatic osteosarcoma is a very aggressive type of osteosarcoma and is seen predominantly in the second and third decades of life. The lesions are expansile and destructive, and largely composed of cystic cavities containing necrosis and hemorrhage. Multiple aneurysmally dilated cystic cavities separated by septations are seen. Fluid–fluid levels are seen commonly. Nodularity can be seen along septations and periphery, which is a key feature to differentiate from ABCs.
Additional Diagnostic Considerations
Fibrous dysplasia:Fibrous dysplasia is a noninherited bone disease characterized by replacement of normal lamellar cancellous bone by abnormal fibrous tissue. It can be monostotic or polyostotic. The radiographic appearance varies, with lesions containing greater fibrous content appearing more radiolucent and a characteristic ground glass appearance. Lesions with greater osseous content are more sclerotic. Fluid–fluid levels have been reported in cystic fibrous dysplasia.
Chondroblastoma:Chondroblastoma is a benign cartilaginous tumor, mostly seen between the ages of 5 and 25 years and in epiphyses or apophyses of long bones. On imaging, it manifests as a geographic, lytic lesion that may contain chondroid matrix. They can show fluid–fluid levels.
Diagnosis
Aneurysmal bone cyst.
Pearls
ABCs commonly show fluid–fluid levels.
SBCs can show fluid–fluid levels in association with a pathologic fracture.
Telangiectatic osteosarcomas can show nodularity along septations and periphery which can be very helpful in distinguishing them from ABCs.
Suggested Readings
- 57 Keenan S, Bui-Mansfield LT. Musculoskeletal lesions with fluid-fluid level: a pictorial essay.. J Comput Assist Tomogr 2006; 30 (3) 517-524 PubMed 16778633
- 58 Van Dyck P, Vanhoenacker FM, Vogel J et al. Prevalence, extension and characteristics of fluid-fluid levels in bone and soft tissue tumors.. Eur Radiol 2006; 16 (12) 2644-2651 PubMed 16612549
Case 20

Clinical History
A 56-year-old female with incidentally discovered lesion on shoulder radiographs (Fig. 20‑1).
Key Finding
Focal lesion with chondroid matrix.
Top 3 Differential Diagnoses
Enchondroma: Enchondroma is a benign chondroid lesion with a characteristic “arcs and rings” pattern of mineralization within an intramedullary lucent lesion. The lesions are common in the long tubular bones, particularly distal femur, proximal tibia and proximal humerus. They usually appear purely lucent in the short tubular bones of hands and feet, another common location. CT may show matrix calcifications to better advantage. On MRI, enchondromas are seen to be composed of high-T2 signal intensity lobules with thin intervening low-T2 signal intensity septations and mineralizations.
Chondrosarcoma: Chondrosarcoma is the third most common primary malignant bone tumor. Chondroid matrix mineralization is seen in 60 to 78% of lesions. It can be challenging to differentiate between low-grade chondrosarcomas and enchondromas on imaging alone. Features that would suggest chondrosarcoma include clinical symptom of pain, size greater than 6 cm, rapid growth, cortical breakthrough, deep endosteal scalloping (more than two-thirds of the overlying cortex), and soft-tissue component.
Chondroblastoma: Chondroblastoma is an uncommon benign lesion occurring before skeletal maturity, characteristically presenting in the epiphyses of long bones like femur, and humerus and in epiphyseal equivalents like patella. These lesions can have chondroid matrix; however, young age of the patient, typical location, and smaller size help to differentiate these lesions from clear cell chondrosarcoma.
Additional Diagnostic Consideration
Bone infarct: Medullary bone infarcts can sometimes mimic chondroid lesions on plain radiography. The key to differentiating the two is that calcifications are more central in chondroid lesions and more peripheral in bone infarcts which show a serpentine margin. On MRI, bone infarcts present as geographic medullary lesions with central fat (bright on T1) and a margin that is hypointense on both T1- and T2-weighted sequences.
Diagnosis
Enchondroma.
Pearls
Enchondromas are common benign chondroid lesions with ”rings and arcs” mineralizations.
It is difficult to distinguish enchondromas and low-grade chondrosarcomas in long bones on imaging. Pain, deep endosteal scalloping and other aggressive features favor chondrosarcoma.
Bone infarcts have serpentine, calcified margins.
Suggested Readings
- 59 Brien EW, Mirra JM, Kerr R. Benign and malignant cartilage tumors of bone and joint: their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology. I. The intramedullary cartilage tumors.. Skeletal Radiol 1997; 26 (6) 325-353 PubMed 9229417
- 60 Murphey MD, Flemming DJ, Boyea SR et al. Enchondroma versus chondrosarcoma in the appendicular skeleton: differentiating features.. Radiographics 1998; 18: 1213-1237
- 61 Murphey MD, Walker EA, Wilson AJ, Kransdorf MJ, Temple HT, Gannon FH. From the archives of the AFIP: imaging of primary chondrosarcoma: radiologic-pathologic correlation.. Radiographics 2003; 23 (5) 1245-1278 PubMed 12975513
Case 21

Key Finding
Osseous lesion with osteoid matrix.
Top 3 Differential Diagnoses
Osteosarcoma: Osteosarcoma is the most common primary malignant tumor of bone in adolescents and young adults. Identification of osteoid matrix and aggressive features usually allow easy prospective radiologic diagnosis of this tumor. Intramedullary osteosarcomas frequently affect long bones, particularly about the knee. A vast majority of these lesions (90%) demonstrate fluffy, cloud-like opacities, which are characteristic of osteoid matrix, within the lesion. Occasionally, the lesion may be completely blastic or lytic. Ossifications may also be seen in metastases.
Osteoid osteoma: Osteoid osteoma is a benign bone tumor seen in boys and men between 7 and 25 years of age. Typical findings include an intracortical nidus that may display a variable amount of mineralization, accompanied by cortical thickening and reactive sclerosis in the shaft of a long bone. CT is more sensitive than radiography for detection of the mineralized osteoid within the nidus.
Osteoblastoma: Osteoblastoma is an uncommon benign bone-forming lesion that is histologically identical to osteoid osteoma. It has a predilection for the spine and is almost always in the posterior elements. Osteoblastoma displays progressive growth and may have malignant potential. At imaging, osteoblastoma is usually more expansile, larger than 2 cm, with more osteoid tissue formation, and has less surrounding sclerosis than osteoid osteoma. In spine, it can have a blowout appearance similar to aneurysmal bone cyst. Osteoblastomas can also have an aggressive appearance, simulating an osteosarcoma.
Additional Diagnostic Consideration
Enostosis: Enostosis, or bone island, is a small benign lesion seen as round or oval focus of dense bone within medullary space. Spiculated margins or brush borders are seen classically. Their appearance is pathognomonic; however, if large in size, multiple or in patients with history of a primary malignancy, they may need to be distinguished from other blastic lesions with the help of radionuclide imaging on which they show no or occasionally low-grade activity.
Diagnosis
Osteosarcoma.
Pearls
Osteosarcomas with osteoid matrix and aggressive features usually do not pose a diagnostic challenge.
CT is more sensitive for detection of mineralization in the central nidus of osteoid osteomas.
Osteoblastomas can have a variety of appearances but are usually larger than 2 cm and with less surrounding sclerosis than osteoid osteomas.
Suggested Readings
- 62 Chai JW, Hong SH, Choi JY et al. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings.. Radiographics 2010; 30 (3) 737-749 PubMed 20462991
- 63 Murphey MD, Robbin MR, McRae GA, Flemming DJ, Temple HT, Kransdorf MJ. The many faces of osteosarcoma.. Radiographics 1997; 17 (5) 1205-1231 PubMed 9308111
Case 22

Key Finding
Polyostotic lesions–looks like a syndrome.
Top 3 Differential Diagnoses
Hereditary multiple exostoses (HME): HME is characterized by multiple osteochondromas and shows an autosomal dominant inheritance pattern. Any bone can be involved except calvarium. The lesions are similar to solitary osteochondromas with cortical and medullary bone protruding and continuous with the underlying bone and can be pedunculated or sessile. Hyaline cap may show chondroid calcifications, has variable thickness and best measured by MRI. Various complications associated with osteochondromas include osseous deformity, vascular or neurologic compromise, bursa formation, and malignant transformation. The prevalence of malignant transformation is higher than with solitary osteochondromas.
Enchondromatosis: Ollier disease or enchondromatosis is defined by presence of multiple enchondromas with asymmetric distribution of lesions which can be extremely variable (in terms of size, number, and evolution of enchondromas). Enchondromatosis associated with soft-tissue hemangiomas is called Maffucci syndrome. Both disorders appear spontaneously and are not inherited. Enchondromas are exclusively located in the metaphyses of long bones and in the small bones of hand and feet. They appear as multiple lucent lesions that may show chondroid calcifications. Growth abnormalities and deformities are common. Reported risk of malignant transformation varies from 5 to 50% of cases.
Polyostotic fibrous dysplasia: Fibrous dysplasia is a benign skeletal disorder characterized by replacement of medullary bone with fibrous tissue. Polyostotic form may involve a few or many bones, most commonly skull, facial bones, pelvis, and spine. The lesions have varying degrees of density and may display characteristic ground glass appearance. Deformities like shepherd’s crook may be seen. McCune–Albright syndrome consists of a triad of precocious puberty, café’ au lait spots, and polyostotic fibrous dysplasia.
Additional Diagnostic Consideration
Neurofibromatosis (NF): Multiple, well-defined, lucent expansile lesions with sclerotic margins may be seen with NF-1, possibly representing nonossifying fibromas.
Diagnosis
Maffucci syndrome.
Pearls
HME consists of multiple sessile or pedunculated osteochondromas.
In enchondromatosis, growth abnormalities and deformities are common.
Polyostotic fibrous dysplasia tends to involve larger segments of bone with severe deformities.
Suggested Readings
- 64 Fitzpatrick KA, Taljanovic MS, Speer DP et al. Imaging findings of fibrous dysplasia with histopathologic and intraoperative correlation.. AJR Am J Roentgenol 2004; 182 (6) 1389-1398 PubMed 15149980
- 65 Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: variants and complications with radiologic-pathologic correlation.. Radiographics 2000; 20 (5) 1407-1434 PubMed 10992031
- 66 Silve C, Jüppner H. Ollier disease.. Orphanet J Rare Dis 2006; 1: 3-7 PubMed 16995932
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree