Part 3: Upper Extremity
Case 36

Clinical History
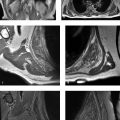
A 21-year-old female with pain at the shoulder with overhead movements (Fig. 36‑1).
Key Finding
Abnormal/variant appearance of anterosuperior labrum.
Top 3 Differential Diagnoses
Sublabral sulcus: A sublabral sulcus or recess is the most common normal variant of glenoid labrum. If one utilizes a clock face description for the glenoid (such that when looking at it en face on sagittal imaging, the biceps tendon attachment upon the labrum is defined as the 12 o’clock position while anterior at the level of the equator is termed the 3 o’clock position), it is usually present between 11 o’clock and 3 o’clock positions. A normal sulcus is identified as a small linear fluid-filled gap between the labrum and the glenoid articular cartilage. This small cleft has smooth margins, parallels the glenoid articular cartilage, and is usually anterior to the biceps anchor. This can be typically identified on conventional MRI but is best depicted on coronal MR arthrographic imaging, with linear fluid signal following the contour of the medial glenoid articular cartilage, and a triangular appearance of the labrum just lateral to the fluid signal cleft.
Sublabral foramen: A sublabral foramen or hole is a focal detachment of the labrum from the glenoid rim in the anterosuperior quadrant, usually located between 12 o’clock to 3 o’clock positions. It is found in about 10% of individuals. Similar to a sublabral sulcus, there will be smooth margins, and there should be no extension into the long head biceps tendon or glenohumeral ligaments.
Buford complex: In a Buford complex, the middle glenohumeral ligament is thickened, and the anterior–superior glenoid labrum is absent. This occurs in about 1% of individuals and can be differentiated from a tear of the labrum by its lack of involvement of the labrum at the biceps tendon attachment. While both a sublabral foramen and a Buford complex are normal variants, individuals with these anatomic variants have an increased risk of a labral tear, which is felt to be due to increased laxity and tension placed upon the remainder of the labrum. It is important to recognize these anatomic variants, as attempts to repair a normal labrum in these cases may lead to decreased range of motion and pain.
Additional Diagnostic Consideration
SLAP tear: A tear of the superior glenoid labrum extending anterior to posterior is termed a SLAP tear. This tear can sometimes be challenging to differentiate from normal variants. Key imaging features that can aid the radiologist in making the diagnosis of a SLAP lesion include the presence of fluid signal extending laterally into the labrum, irregular margins, extension into and posterior to the attachment of the long head biceps tendon upon the labrum, more than 2 to 2.5 mm width of signal abnormality, and presence of paralabral cysts.
Diagnosis
Buford complex.
Pearls
Anatomic variants are commonly seen in the anterosuperior and superior labrum.
Presence of intralabral signal, irregular margins, nonparallel orientation to glenoid margin, and extension of signal posterior to biceps anchor are some features that aid in the diagnosis of a SLAP lesion.
Suggested Readings
- 102 De Coninck T, Ngai SS, Tafur M, Chung CB. Imaging the glenoid labrum and labral tears.. Radiographics 2016; 36 (6) 1628-1647 PubMed 27726737
- 103 De Maeseneer M, Van Roy F, Lenchik L et al. CT and MR arthrography of the normal and pathologic anterosuperior labrum and labral-bicipital complex.. Radiographics 2000; 20 (Spec No) S67-S81 PubMed 11046163
Case 37

Key Finding
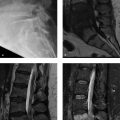
Abnormality of inferior glenohumeral ligament.
Top 3 Differential Diagnoses
Capsular avulsion: The inferior glenohumeral ligament (IGHL) extends from the inferior labrum to the surgical neck of the humerus and consists of anterior and posterior bands, with an intervening axillary recess of capsule. IGHL can avulse at its humeral or glenoid attachments as a result of acute traumatic glenohumeral subluxation or dislocation. These injuries are termed humeral avulsion of the glenohumeral ligament (HAGL) and glenoid avulsion of the glenohumeral ligament (GAGL), respectively. On MRI, the IGHL is best visualized on oblique coronal sequences as a hypointense “U” shaped band, serving as the inferior portion of the glenohumeral joint capsule, which is also termed the axillary pouch. Both HAGL and GAGL are best identified on MRI as either change in configuration of the IGHL to a “J” shape and extravasation of fluid or injected contrast, extending inferiorly into the axilla. In a subset of patients, there may also be an avulsion fracture at the humeral attachment. The HAGL lesion is an important cause of anterior instability of the glenohumeral joint.
Midsubstance tear: Midsubstance tears represent about a third of IGHL injuries. When the IGHL fails at this location, the fluid within the glenohumeral joint may escape inferiorly into the axilla, or the inferior joint capsule may no longer be its typical “U” shape on oblique coronal MRI sequences.
Adhesive capsulitis: Adhesive capsulitis is a clinically diagnosed condition characterized by painful limitation of motion of shoulder. Multiple imaging findings have been described in this entity, including thickening and intermediate- to high-signal of the inferior glenohumeral ligament. This can be differentiated from IGHL injury primarily by clinical presentation, but also by the lack of other imaging findings that may be found in a shoulder dislocation (Hill–Sachs impaction fracture and anterior inferior labral injury) that led to injury of IGHL. Similar to IGHL injury, the thickening and intermediate/edema signal of the IGHL in adhesive capsulitis is best identified on oblique coronal, fat-suppressed fluid-sensitive sequences. Other findings described on MRI in adhesive capsulitis include edema and soft-tissue thickening within the rotator interval, and thickening of the coracohumeral ligament.
Diagnosis
Midsubstance tear of the IGHL related to a shoulder dislocation.
Pearls
IGHL tears can result from shoulder dislocations. Injuries are best identified in the acute setting as extravasation of fluid, contrast from axillary recess, or abnormal J shape of the inferior joint capsule.
Thickening and intermediate signal of the IGHL can be seen in adhesive capsulitis.
Suggested Readings
- 104 Omoumi P, Teixeira P, Lecouvet F, Chung CB. Glenohumeral joint instability.. J Magn Reson Imaging 2011; 33 (1) 2-16 PubMed 21182115
- 105 Walz DM, Burge AJ, Steinbach L. Imaging of shoulder instability.. Semin Musculoskelet Radiol 2015; 19 (3) 254-268 PubMed 26021586
Case 38

Key Finding
Abnormality of proximal long head of biceps tendon.
Top 3 Differential Diagnoses
Dislocation or subluxation: The coracohumeral ligament, superior glenohumeral ligament, subscapularis tendon, and supraspinatus tendon are all important in maintaining the stability of the long head biceps tendon (LHBT) within the bicipital groove. On ultrasound or MRI, if the long head biceps tendon is not identified within the bicipital groove, there should be close inspection for medial displacement or tear of the biceps tendon. Displacement of the LHBT can occurs due to injury of any of the four aforementioned stabilizers, although, most frequently, this is due to a tear of the subscapularis tendon. The dislocated tendon may be anterior to subscapularis tendon, within an intratendinous tear of subscapularis tendon, or deep to the subscapularis tendon in an intra-articular location.
Tendon tear: Partial and complete tears of LHBT are usually associated with underlying tendon pathology like degeneration. Complete rupture occurs most commonly in the bicipital groove or just proximal to the groove. It is commonly accompanied by “popeye” deformity, a bulge that occurs over the anterior arm from retraction of the torn tendon and muscle. Partial tears are seen as sudden reduction in caliber and irregularity of the tendon contour. Complete tears are indicated by absence of the tendon in the groove, and careful inspection confirms that the tendon is not dislocated. In acute ruptures, ventral edema and retracted tendon stump may also be seen. LHBT tears are very common in individuals with rotator cuff abnormalities, occurring in approximately 75% of individuals with rotator cuff tears.
Tendinitis: Biceps tendinitis is not an uncommon finding on MR imaging, especially in the presence of abnormalities of supraspinatus and subscapularis. Tendinitis can occur in both diffuse and segmental form. The imaging findings of tendinitis are increased signal in the tendon on all pulse sequences, and thickening and inhomogeneity of the tendon.
Additional Diagnostic Consideration
Variant anatomy: A wide range of anatomic variations has been reported for LHBT and proximal biceps, including aberrant intra-articular and extra-articular origin, congenital absence, and accessory heads. In individuals with a congenitally absent tendon, the bicipital groove will be either hypoplastic or absent. Other common variations about the long head biceps tendon that may mimic an injury include a duplication or bifurcation of the long head biceps tendon. On MRI, an accessory tendon is seen as an additional hypointense structure in the bicipital groove which is flattened and can be misinterpreted as a longitudinal tear of LHBT without carefully tracing the tendon to its origin.
Diagnosis
Medial dislocation of the long head biceps tendon into an interstitial tear of subscapularis.
Pearls
Tears of the subscapularis tendon are the most common cause of medial dislocation of the LHBT.
There is a very high association of injuries of the LHBT with rotator cuff tears.
An accessory LHBT tendon can be misinterpreted as a longitudinal tear without carefully tracing it to its origin.
Suggested Readings
- 106 Beltran J, Jbara M, Maimon R. Shoulder: labrum and bicipital tendon.. Top Magn Reson Imaging 2003; 14 (1) 35-49 PubMed 12606868
- 107 Petchprapa CN, Beltran LS, Jazrawi LM, Kwon YW, Babb JS, Recht MP. The rotator interval: a review of anatomy, function, and normal and abnormal MRI appearance.. AJR Am J Roentgenol 2010; 195 (3) 567-576 PubMed 20729432
Case 39

Key Finding
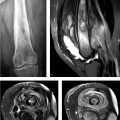
Tear of the anteroinferior labrum.
Top 3 Differential Diagnoses
Bankart lesion: A Bankart lesion is an injury to the anteroinferior labrum, which may involve the labrum or both the labrum and adjacent bony glenoid. The labrum (and potentially the glenoid) will be displaced due to a tear of the adjacent periosteum. This injury to the labrum is most commonly associated with an anterior shoulder dislocation. It commonly coexists with a Hill–Sachs lesion, which is a compression fracture of posterolateral humeral head. The detached labrum can remain in situ or migrate distal to its attachment site. MR imaging demonstrates a disrupted medial scapular periosteum, irregular fluid, or contrast extending into or deep to the labrum, but the labrum stays continuous to the anterior inferior glenohumeral ligament.
Perthes lesion: When the anteroinferior labrum is detached from the glenoid surface but the labrum is still partially attached by the periosteum and not displaced, the injury is called a Perthes lesion. This can be difficult to see both by imaging and arthroscopy, as the labrum may appear to be in normal position, unlike a Bankart lesion. The pressure placed upon the labrum by distension of the joint with fluid in an MR arthrogram can better depict a Perthes lesion. In addition, placing the arm in the abducted and externally rotated (ABER) position as part of an MR arthrogram can best identify a Perthes lesion due to stress placed upon the anterior labrum by a taut inferior glenohumeral ligament in this position. The Perthes injury can be found both due to an acute traumatic event or repetitive stress.
Anterior labroligamentous periosteal sleeve avulsion (ALPSA):An ALPSA lesion is often the result of a chronic injury rather than acute dislocation. This entity is similar to a Perthes lesion in that the anteroinferior labrum is separated from the glenoid surface, and the labrum will be partially attached to the periosteum. However, unlike in a Perthes lesion, the labrum is displaced medially along the anterior aspect of the scapular neck in an ALPSA lesion. As the labrum is not in its normal position, this is easier to diagnose on MR than its similar correlate, the Perthes lesion.
Diagnosis
Perthes lesion.
Additional Diagnostic Consideration
Glenoid labral articular disruption (GLAD): In a GLAD lesion, the anteroinferior labrum and a portion of the adjacent articular cartilage are torn, and these may be either minimally displaced or displaced medially. Unlike the other above-mentioned entities, this more commonly occurs as a direct acute traumatic impaction injury rather than a dislocation injury. MR arthrography can best depict the tear of the glenoid articular cartilage.
Pearls
In a Bankart lesion, there is detachment of the labrum and disruption of the scapular periosteum.
ABER positioning can help in identifying a Perthes lesion on MR.
In an ALPSA lesion, the labrum is detached, and the scapular periosteum is stripped with medial displacement of labrum.
Suggested Readings
- 108 Bencardino JT, Gyftopoulos S, Palmer WE. Imaging in anterior glenohumeral instability.. Radiology 2013; 269 (2) 323-337 PubMed 24155283
- 109 De Coninck T, Ngai SS, Tafur M, Chung CB. Imaging the Glenoid Labrum and Labral Tears.. Radiographics 2016; 36 (6) 1628-1647 PubMed 27726737
Case 40

Key Finding
Bursa or cyst around the shoulder.
Top 3 Differential Diagnoses
Subacromial–subdeltoid bursa: Subacromial–subdeltoid bursa is superficial to all the rotator cuff tendons. It does not communicate with the glenohumeral joint. If there is a full-thickness tear of rotator cuff, an abnormal communication gets established between the glenohumeral joint and the subacromial–subdeltoid bursa, allowing fluid to escape from the joint into the bursa. Inflammation and distension of this bursa can also occur in infectious or inflammatory conditions, such as calcium hydroxyapatite deposition without a rotator cuff tear. It can be normal to have a trace amount of fluid within this bursa.
Geyser sign: In a full-thickness rotator cuff tear, fluid can escape from the glenohumeral joint into the subacromial–subdeltoid bursa and then into the acromioclavicular (AC) joint. If considerable pressure and fluid are present, a fluid-filled mass called geyser sign can develop above the AC joint. The geyser sign on shoulder arthrography is characterized by extension of contrast from the glenohumeral joint to subacromial–subdeltoid bursa and then into the AC joint space. It usually indicates full-thickness tear of the rotator cuff of long duration, with erosion of the inferior capsule of AC joint. Sometimes, this mass can get large and simulate a tumor clinically.
Subcoracoid bursa: Subcoracoid bursa is located anterior to the subscapularis and inferior to coracoid and subscapularis recess. It does not communicate with glenohumeral joint but does communicate with subacromial–subdeltoid bursa. Distension of this bursa occurs with bursitis or full-thickness rotator cuff tears. The subcoracoid bursa can be differentiated from the subscapularis recess by its further inferior extent anterior to the subscapularis muscle, and its location purely anterior to the subscapularis muscle.
Diagnosis
Subacromial–subdeltoid bursitis.
Additional Diagnostic Considerations
Paralabral cyst: A paralabral cyst usually shows close relationship with the labrum and is frequently found in association with a labral tear. MRI appearance may vary from a small unilocular to a large multilocular cystic lesion. Paralabral cyst of suprascapular or spinoglenoid notch can cause entrapment of suprascapular nerve.
Long head of biceps tendon sheath fluid: The synovial sheath of long head of biceps tendon communicates with the glenohumeral joint. Fluid in the biceps tendon sheath should not be considered abnormal unless the tendon is completely surrounded by it or there are morphological alterations in the biceps tendon.
Pearls
If there is more than a trace fluid within the subacromial–subdeltoid bursa, the rotator cuff should be closely evaluated for a tear.
Geyser sign usually indicates full-thickness tear of rotator cuff of long duration.
Subcoracoid bursa is differentiated from subscapularis recess by its further inferior extent and entirely anterior location to subscapularis.
Suggested Readings
- 110 Mellado JM, Salvadó E, Camins A et al. Fluid collections and juxta-articular cystic lesions of the shoulder: spectrum of MRI findings.. Eur Radiol 2002; 12 (3) 650-659 PubMed 11870482
- 111 Motamedi D, Everist BM, Mahanty SR, Steinbach LS. Pitfalls in shoulder MRI: part 2–biceps tendon, bursae and cysts, incidental and postsurgical findings, and artifacts.. AJR Am J Roentgenol 2014; 203 (3) 508-515 PubMed 25148153
Case 41

Key Finding
Rotator cuff abnormality.
Top 3 Differential Diagnoses
Partial thickness tear: Partial-thickness rotator cuff tears can be described according to the surface of the tendon involved as well as the percentage of tendon involved. Tears may involve the articular surface, bursal surface, or intrasubstance. Articular surface tears are the most common type. They are seen as the focal region of tendon discontinuity which is filled with fluid on T2-weighted imaging. Fat-suppressed, T2-weighted imaging increases lesion conspicuity. Additional findings may include surface fraying or changes in tendon caliber such as attenuation or thickening. Tendon retraction may occasionally be seen in high-grade, partial-thickness tears. Intrasubstance tears are characterized by intratendinous T2 fluid signal without extension to either articular or bursal surface. Bursal-sided tears involve the superior or bursal surface of the tendon with an extra-articular, fluid-filled gap. Partial-thickness tears are classified arthroscopically according to the degree of tendon involvement. Grade 1 lesions involve less than 25% (less than 3 mm) of tendon thickness; grade 2 lesions involve 25 to 50% (3–6 mm); and grade 3 lesions involve greater than 50% of the tendon (greater than 6 mm).
Full-thickness tear: In full-thickness tears, the discontinuity of the tendon extends from the articular surface to the bursal surface. Of the four rotator cuff tendons (supraspinatus, infraspinatus, subscapularis, and teres minor), a full-thickness tear most commonly involves the supraspinatus, and this most often is at its insertion upon the greater tuberosity. Full-thickness tears can be classified based on the size of the tears—small (less than 1 cm), medium (1–3 cm), large (3–5 cm), and massive (greater than 5 cm). The tear does not need to involve the entire tendon in an AP dimension to be considered a full-thickness tear. The most characteristic sign of a full-thickness tear is tendon discontinuity with a fluid-filled gap. Secondary signs include presence of fluid in subacromial–subdeltoid bursa, tendon retraction, and muscle atrophy. Muscle atrophy usually indicates chronicity, although there can be other causes of muscle atrophy even in the presence of an intact cuff.
Rotator cuff tendinosis: Classically, rotator cuff tears occur in cuff tendons with preexisting tendinosis. On MRI, there is increased signal in the tendon on proton density and T2-weighted images, but signal intensity will not reach that of fluid, and the area of abnormality is more globular in appearance than linear as would be found with a tear. Differentiation between tendinosis and a partial-thickness tear can sometimes be challenging. One pitfall of assessing the tendons on short TE images is that magic angle phenomenon can result in artificially increased signal in regions where the tendon courses at a 55-degree angle in relation to the main magnetic field. Magic angle artifact should resolve on T2-weighted (long TE) sequences.
Diagnosis
Full thickness tear of the supraspinatus tendon.
Pearls
The supraspinatus is the most commonly torn tendon of the rotator cuff.
Rotator cuff tears should be described by thickness as well as width (anterior to posterior dimension).
Differentiation between a partial-thickness tear and tendinosis of rotator cuff can sometimes be challenging; in tendinosis, the increased T2 signal of the tendon tends to be globular rather than linear and not reach fluid intensity.
Suggested Readings
- 112 Kassarjian A, Bencardino JT, Palmer WE. MR imaging of the rotator cuff.. Radiol Clin North Am 2006; 44 (4) 503-523 PubMed 16829246
- 113 Morag Y, Jacobson JA, Miller B, De Maeseneer M, Girish G, Jamadar D. MR imaging of rotator cuff injury: what the clinician needs to know.. Radiographics 2006; 26 (4) 1045-1065 PubMed 16844931
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree