Pyogenic spondylitis and discitis are usually seen following a recent infection or surgery. A septic embolus causes an infarcted area within the bone. Pyogenic spondylitis is characterized by edema, vascular leakage, and supportive inflammatory reaction characterized with polymorphonuclear leukocytes. In tuberculosis of the spine, active lesions are characterized by formation of epithelioid granulomas with central caseating necrosis. Mycobacterium tuberculosis can be shown by histochemical stains for acid-fast bacteria or by immunochemistry. In brucella spondylitis, microgranulomatous proliferation composed of histiocytes containing numerous bacilli without caseating necrosis is characteristic. Brucella melitensis can be shown on histochemical Gram stain.
Key points
- •
Histopathologic features should be correlated with the pathologic changes during the evaluation of different stages of spondylitis with various causes.
- •
Differential diagnosis between pyogenic and chronic granulomatous spondylitis is significant for the outcome of the patients.
- •
Histopathologic changes seen in discitis, although primarily less investigated, could be helpful for understanding the nature of the disease.
Pyogenic spondylitis and discitis
Pyogenic spondylitis and discitis are usually seen following a recent infection or a surgery. In routine practice, because vertebral osteomyelitis and intervertebral discitis usually occur in conjunction with one another, spondylodiscitis is the preferred term to define this condition. The most common cause of both pyogenic spondylitis and discitis is hematogenous spread of Staphylococcus aureus .
In adults, the intervertebral disc is avascular, without direct blood supply; in contrast, the subchondral metaphyseal region of the vertebral body has the richest vascular network. A septic embolus causes an infarcted area within the bone where a subsequent infection settles down to form pyogenic spondylitis. As well as many other enzymes, the pyogenic bacteria express some receptors for collagen, the main bone matrix component, which help them to adhere.
Most hematogenous infections of the disc space are the result of dissemination from the infected adjacent bone. However, in isolated discitis, inoculation of the pyogenic bacteria during the surgical procedure under suboptimal conditions remains the main cause. Here, the protease activity via proteolytic enzymes of pyogenic bacteria is particularly responsible for degrading of proteins within the disc structure.
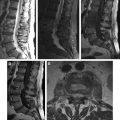
Pyogenic spondylitis is characterized by a suppurative inflammatory reaction. Within the infected area, histologic changes are closely related to the duration of spondylitis. In the early acute phase, vascular dilation and vascular endothelial fluid leakage produce edema between the intertrabecular area of bone. The vessels in the bone marrow are fenestrated, enabling the rapid fluid outflow. The pressure of the area increases and the vascular blood flow reduces, initiating the ischemic process. The acute inflammatory exudate composed of polymorphonuclear cells, mainly the neutrophil leukocytes, and proteinous material then collects in this infected area. Because the bone is highly vascularized, ischemia-induced endogenous lysosomal activity of neutrophils destroys the bone matrix more rapidly. Because of this suppuration and ongoing ischemia, bone necrosis develops within 48 hours. If the inflamed area is close to the cortex, cortical bone destruction may be prominent, otherwise the destruction mainly takes place in the medulla.
In discitis, especially when the disc has a degenerative disease or a traumatic condition, which means a vascularized disc structure facilitating these enzymatic activities, the progression of this acute inflammatory phase is more rapid. In the subacute and early regenerative phases, after the first 48 hours, the neutrophilic infiltration gradually ceases and mononuclear inflammatory cells (mainly the lymphocytes and macrophages) enter the area within the granulation tissue made up of newly formed fine capillary network and proliferation of fibroblastic cells in an edematous background. This process results in swelling of the disc. The degenerative and destructive changes characterized by a cracking and myxohyalinized appearance follow this stage. In the late regenerative and subsequent chronic phase, edema subsides, lymphocytes and plasma cells dominate, and fibroblastic proliferation accompanies, which may end up the shrinked and sclerotic disc material.
The elastase activity of Staphylococcus aureus destroys the elastic reticular network of the bone and the discs, particularly inducing fibrosis. However, even in the chronic stage, neutrophil foci may continue to exist, as well as areas of ischemic necrosis and reactive newly produced bone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree