1 Pathological Anatomy, Diagnosis, and Treatment
Clinical Terms
The common constellations of symptoms and signs resulting from degenerative disorders of the spine are referred to as spine syndromes. If the clinical findings are confined to a specific region of the spine, reference is made to a localized cervical, thoracic, or lumbar spine syndrome. Two-thirds of all spinal disorders involve the inferior portion of the lumbar spine (Table 1.1). About one-third involve the cervical spine, and only about 2% involve the thoracic spine.
____________
1 There is a lack of uniformity in spinal terminology between Europe and North America. Indeed, uniformity may be lacking between various academic and professional centers on each continent.
A lay term for acute lumbar spine syndrome is lumbago. The chronic forms of localized lumbar spine syndrome are usually referred to as low back pain; other terms include chronic low back pain, sacralgia, back pain, and unspecific back pain.
When pain radiates from the lumbar region into the leg, reference is made to radicular or pseudoradicular lumbar spine syndrome. In radicular lumbar spine syndrome, it is possible to identify the affected segment. Sciatica refers to involvement of spinal nerve roots L4 through S2 (generally L5-S1). A lumbar spine syndrome that involves nerve roots L2-3 and also L4 to a certain extent will affect the femoral nerve and is referred to as a high or superior root syndrome. In L5 and S1 sciatica, pain radiates from the lumbosacral region via the lateral surface of the thigh to the posterior and lateral surface of the calf and to the foot. In L5 sciatica, pain radiates to the dorsum of the foot; in S1 sciatica, to the lateral edge of the foot. In high or superior lumbar spine syndrome, the pain radiates along the anterior medial aspect of the thigh to the anterior medial aspect of the calf. This is often associated with weakness of the quadriceps and weakening or absence of the patellar tendon reflex.
In radicular pain syndromes, imaging studies focus on the superior or inferior lumbar spine, depending on whether the pain radiates into the anterior or posterior thigh. CT and MRI studies often reveal nerve root compression due to disk protrusion, disk extrusion, or lateral spinal stenosis.
In pseudoradicular lumbar spine syndrome, the radiating leg pain cannot be reliably correlated with segmental pathology. This syndrome is usually due to morphological defects and dysfunction of the lumbar intervertebral joints (zygapophyseal joints) with their articular facets and joint capsules. For this reason, pseudoradicular lumbar spine syndrome is also referred to as facet syndrome. The sacroiliac joints can also produce pseudoradicular symptoms. Patients with facet syndrome typically report low back pain in the sacral region that increases on bending backward (reclination) and radiates into the buttocks, groin, lower abdomen, thighs, and trochanteric region. The pain is described as diffuse, and patients typically indicate it by placing the palm of the hand over the affected region. In contrast, patients with radicular syndromes typically trace the affected dermatome with a finger as a circumscribed area extending from the lumbosacral region to the foot.
| Term | Synonyms | Causes |
| Lumbar spine syndrome | Lumbar disk syndrome | Degenerative changes in the lumbar spine |
| Localized lumbar spine syndrome | Low back pain, sacralgia, nonspecific back pain | Lumbar spine syndrome with symptoms limited to the lumbosacral region |
| Lumbago | Acute lumbar spine syndrome, acute low back pain | Acute form of localized lumbar spine syndrome |
| Pseudoradicular lumbar spine syndrome | Facet syndrome | Pain radiating from the lumbar vertebral and sacroiliac joints into the leg without correlating segmental pathology |
| Radicular lumbar spine syndrome | Lumbar root syndrome, specific back pain | Lumbar spine syndrome with pain radiating into leg and correlating segmental pathology |
| Sciatica | Ischialgia | Lumbar root syndrome involving nerve roots L4–S2 |
| High radicular lumbar spine syndrome | Superior radicular lumbar spine syndrome, femoral neuralgia | Lumbar root syndrome involving nerve roots L1–4 |
| Cauda equina syndrome | — | Narrowing or blockage of the spinal canal with compression of the cauda equina |
| Sacroiliac joint syndrome | — | Increased mobility and degenerative joint disease in one or both of the sacroiliac joints |
| Baastrup’s phenomenon | Kissing spine | Contact between the spinous processes |
Imaging findings in pseudoradicular syndromes include lumbar hyperlordosis, degenerative disease of the facet joints usually occurring in segments L4-5 and L5-S1, degenerative changes in the sacroiliac joints, narrowing of the intervertebral spaces, and impaction of the facet joints. A pseudoradicular lumbar spine syndrome can, however, also occur with normal imaging studies.
Baastrup’s phenomenon, also known as kissing spine, is contact between the spinous processes in the lower lumbar spine.
Terms such as lumbar spine syndrome, localized lumbar spine syndrome, and pseudoradicular lumbar spine syndrome are usually used to describe degenerative disorders. In contrast, terms such as root syndrome and sciatica are also commonly used to describe nerve root compression of any cause, including tumors, spondylolisthesis, and inflammation.
Pathoanatomic Terms (Table 1.2)
It is often difficult to link clinical symptoms and signs to specific findings in diagnostic imaging studies. Not all findings on imaging studies can be identified as generators of pain, but a correlate in one more imaging modalities exists for every pathoanatomic change occurring in degenerative spinal disorders. Intervertebral disk degeneration is the primary focus of interest, and there are a number of terms that describe aspects of this disease.1 All biomechanical and pathoanatomic changes occurring within the intervertebral space are referred to as degenerative disk disease (Fig. 1.1). The desiccation and tears found in the intervertebral disk tissue are age-related changes, which Schmorl and Junghanns have subsumed under the term “chondrosis intervertebralis.” Although the term “chondrosis” appears to refer specifically to cartilage, the degenerative changes are not limited to the cartilage but, rather, involve the entire disk, including both the nucleus pulposus and the annulus fibrosus. Therefore, it is more appropriate to refer to “degenerative disk disease,” using the term analogously to “degenerative joint disease.” Osteochondrosis (Fig. 1.2) is narrowing of the intervertebral disk with sclerosis of the superior end plates and bony reaction occurring in the setting of disk degeneration. A disk may rapidly lose height during the course of degeneration. This process usually produces severe pain. It is referred to as acute degenerative lysis and corresponds to Crock’s “isolated disk resorption” (15).
Nevertheless, disk degeneration is normally a gradual process. This means that reactive changes can usually be appreciated on the margins of the vertebrae. Such changes are referred to as spondylosis (Fig. 1.3). Degenerative disk disease is accompanied by degenerative joint disease of the facet joints (Fig. 1.4), which are forced to bear greater stresses as a result of increased mobility in the joints and subsidence of the intervertebral disks. This disorder was formerly referred to as spondylarthritis.
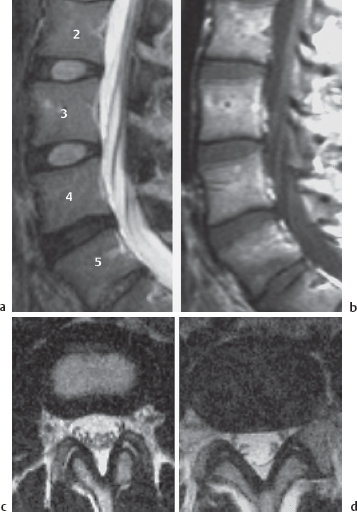
Fig. 1.1a-d Degenerative disk disease at L4-5.
T2: High signal intensity in the nucleus pulposus and the inner portion of the annulus fibrosus, and low signal intensity in the peripheral portion of the annulus fibrosus, in a normal L3-4 intervertebral disk (a, c). Diminished signal intensity, without clear differentiation of the nucleus pulposus and annulus fibrosus, due to degenerative disk disease at L4-5 (a, d).
T1: Identical signals in the normal and degenerated disks (b)
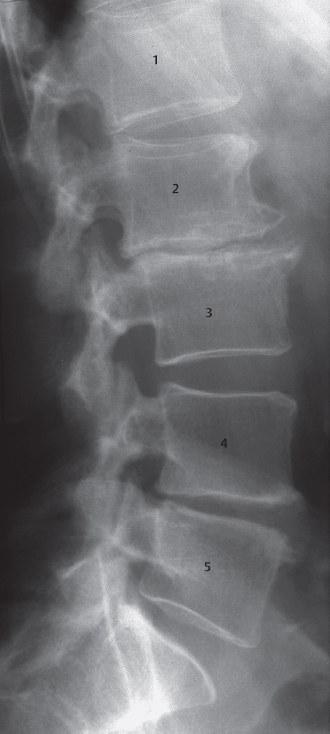
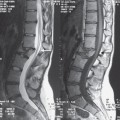
Fig. 1.2 Osteochondrosis of varying severity. Considerable narrowing of the intervertebral space, large osteophytes, contour irregularities of the inferior and superior end plates with increased sclerosis and retrolisthesis in segment L2-3. These findings are significantly less severe in segment L4-5. Compare with the normal L3-4 and L5-S1 segments
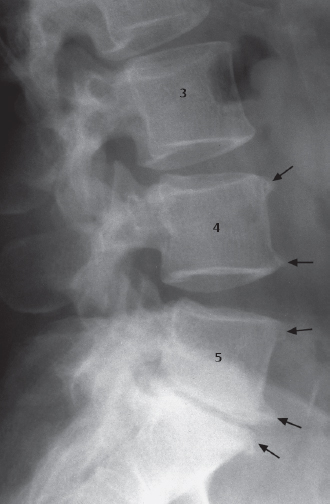
Fig. 1.3 Spondylosis deformans. Spondylophytes (→) on the L4, L5, and S1 bodies with otherwise normal intervertebral spaces at segments L3-4 and L4-5 and osteochondrosis at L5-S1
An accumulation of gas in the interior of the disk in advanced degenerative disk disease is referred to as the vacuum phenomenon (Fig. 1.5). This finding is of no clinical significance and requires no treatment.
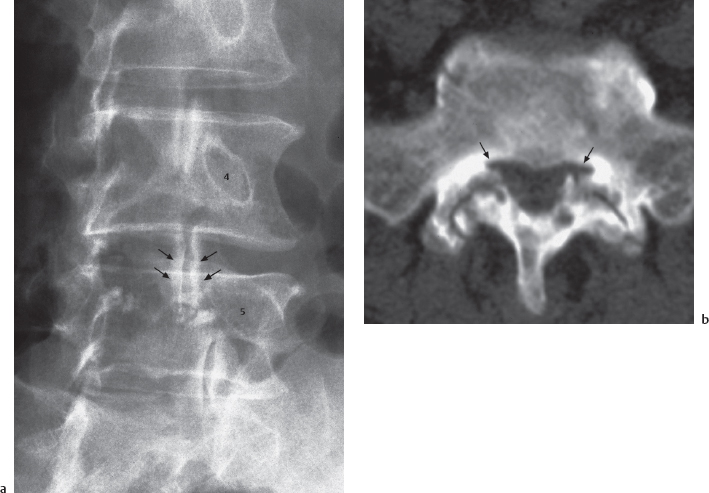
Fig. 1.4a, b Degenerative joint disease of the facet joints (spondylarthritis). a Oblique image of the lumbar spine. Significantly increased sclerosis and contour irregularities of the articular surfaces of the facet joints, especially at L4-5 (→). b CT at L5-S1. Significant narrowing of the articular surfaces, increased subchondral sclerosis, subchondral cysts, and bony processes with secondary recess stenosis (→)
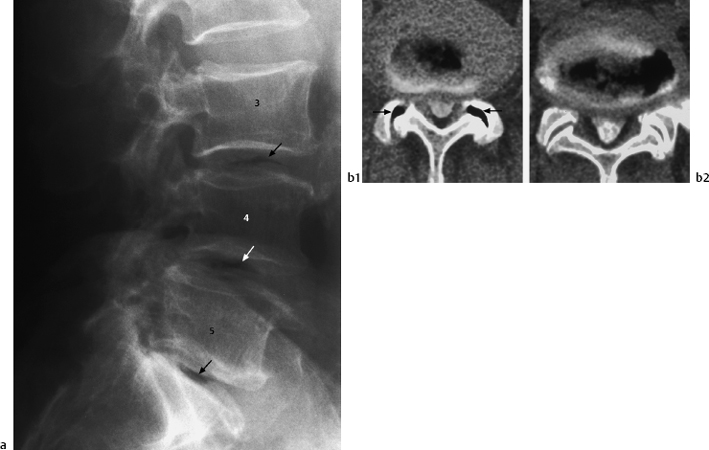
Fig. 1.5a, b Vacuum phenomenon. a Lateral view of the lumbar spine demonstrating a vacuum phenomenon (→) in the intervertebral disks of the last three segments, associated with osteochondrosis. Note pseudospondylolisthesis at L4-5. b CT myelography of the same patient at L4-5 (b1) and L5-S1 (b2). The intradiskal gas inclusions are clearly demarcated. There is also gas in the facet joints bilaterally at L4-5 (→)
| Term | Synonym | Description |
| Degenerative disk disease (Fig. 1.1) | Disk degeneration, chondrosis intervertebralis | All biomechanical and pathoanatomic changes in the intervertebral space associated with disk degeneration |
| Osteochondrosis (Fig. 1.2) | Disk narrowing and bony reaction in the vertebral endplates in degenerative disk disease | |
| Spondylosis (Fig. 1.3) | Spondylotic spurs | Marginal osteophytes on the vertebra, spurs, and marginal hyperostosis accompanying degenerative disk disease |
| Degenerative joint disease of the facet joints (Fig. 1.4) | Spondylarthritis, facet arthritis | Degenerative changes in the facet joints |
| Vacuum phenomenon (Fig. 1.5) | Accumulations of gas in the intervertebral space in degenerative disk disease | |
| Protrusion (Figs. 1.7, 1.8) | Bulging disk | Bulging of the disk without perforation of the annulus fibrosus |
| Extrusion (Figs. 1.8–1.11) | Slipped disk | Displacement of disk tissue with perforation of the annulus fibrosus |
Protrusion and Extrusion (Table 1.2, Fig. 1.6)
Pathology
The use of precise terminology to describe the posterior displacement of disk tissue is crucial to every interaction between clinical and imaging professionals.2 Is there a bulging of the disk with an intact annulus, or a herniation through a perforated annulus? A continuous spectrum of variation may be present, ranging from displacement of tissue within the disk to the presence of a free fragment of disk tissue in the vertebral canal. The terms “protrusion” and “extrusion” are commonly used to describe these conditions.
_________
2 Editor’s note: In many countries, there is a lack of standardization in describing lumbar disk abnormalities seen on advanced imaging studies. This problem has been documented among American surgeons, and French, Canadian, and American radiologists. In 1993, the North American Spine Society sponsored a study in which 49 American spine surgeons used 53 terms to describe eight specifically described conditions of a lumbar disc. The classification system used in this book is based on standard German usage and corresponds to that commonly used by many, though not all, professionals in North America. The American Journal of Neuroradiology, in contrast, defines “protrusion” and “extrusion” in purely geometric fashion, without reference to intactness or perforation of the annulus fibrosus. Thus, a frank herniation through a ruptured annulus might still be classified as a protrusion under the AJNR system.
Readers are advised to be aware of inconsistencies in terminology, and to use terms that make sense to them and cause the least possible confusion in their working environment.
Protrusion refers to the bulging of the disk behind a more or less intact annulus fibrosus; extrusion refers to herniation of the disk with perforation of the annulus fibrosus and extrusion of disk tissue. The terms protrusion and extrusion may be further differentiated, as shown in Fig. 1.6. In a protrusion (Figs. 1.7 and 1.8), the displacement occurs within the disk tissue, with the annulus fibrosus intact. A contrast agent injected into the disk remains within the disk and does not flow into the epidural space. A protrusion in this sense corresponds to the terms “contained disk” or “bulging disk,” which are commonly used in English-speaking countries.
In an extrusion (Fig. 1.8–1.12), the displaced disk tissue has completely perforated the annulus fibrosus but may still be covered by the posterior longitudinal ligament or the epidural membrane. MRI cannot distinguish between peripheral portions of the annulus, the posterior longitudinal ligament, and the dura mater. This makes it difficult to differentiate between disk-level circumscribed protrusions and subligamentous extrusions (see also case studies 4, 29, and 46). Anatomic studies (14) have shown that, in the distal portion of the lumbar spine, the posterior longitudinal ligament itself actually covers only the medial portion of the posterior aspect of the vertebra. Further laterally, where the disk extrusions develop, there is the anterior epidural membrane (14), which forms the anterior boundary of the anterior epidural space adjacent to the vertebral body and intervertebral disk. Sequestra that migrate beneath this membrane or beneath portions of the posterior longitudinal ligament are referred to as subligamentous or submembranous fragments. They correspond to a covered perforation from a surgical standpoint. The term herniation is also applicable to this situation, because the displaced tissue is still enveloped by a layer of tissue. A contrast agent injected into the disk (diskography) fills this space, which may extend above or below the disk. This situation is also referred to in English-speaking countries as herniation with a subligamentous fragment.
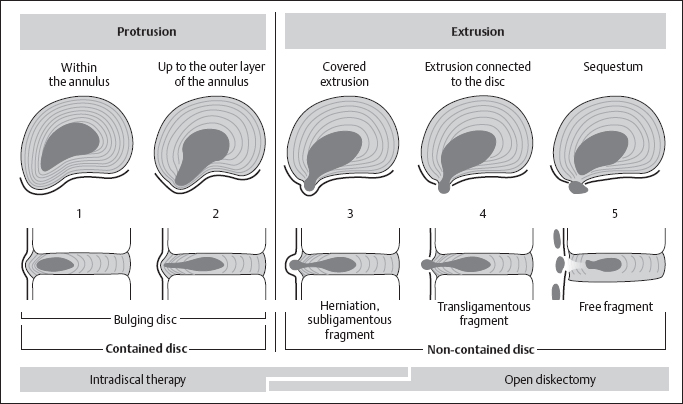
Fig. 1.6 Protrusion and extrusion: progressive degrees of displacement (1–5)
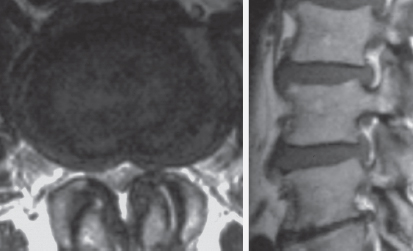
Fig. 1.7 Protrusion. Broad posterior displacement of the intervertebral disk with involvement of the intervertebral foramina (Fig. 1.6, parts 1 and 2; case study 71)
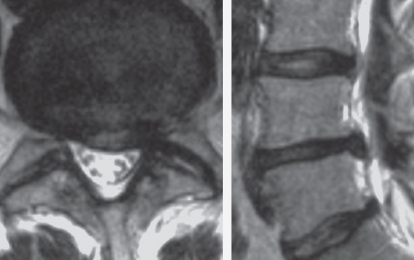
Fig. 1.8 Protrusion with covered subligamentous extrusion (Fig. 1.6, part 3; case study 29)
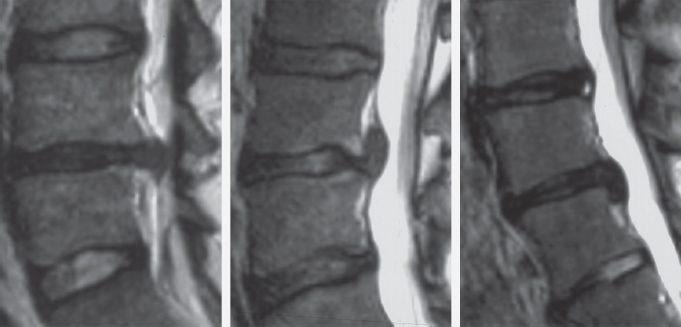
Fig. 1.9a-c Covered extrusion Fig. 1.6, part 3): a at disk level (case study 32), b supradiskal level (case study 56), c infradiskal level (case study 39)
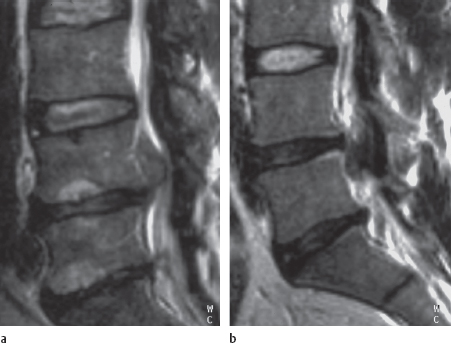
Fig. 1.10a, b Sequestrated disk material obviously originating from the parent disk L4-5 (Fig. 1.6, part 4) a: supradiskal level (case study 35), b infradiskal level (case study 44)
Where the annulus fibrosus and anterior epidural membrane or posterior longitudinal ligament are perforated, the displaced disk tissue will lie in the epidural space. In this case, the perforation is no longer covered. A contrast agent injected into the disk in diskography remains within the disk and does not flow into the epidural space. In an uncovered extrusion, there are two possibilities: The extruded material may remain connected to the disk (Fig. 1.6, no. 4; Fig. 1.10), or it may lie as a sequestrum in the epidural space (Fig. 1.6, no. 5; Fig. 1.11). This distinction is important to the surgeon, in particular, as a connection to a specific intervertebral space indicates which disk is the parent disk, i.e., the disk giving rise to the extrusion.
Therapy
Treatment for protrusion includes all intradiskal procedures such as percutaneous diskectomy, percutaneous laser therapy, and intradiskal injection therapy with substances such as chymopapain (che-monucleolysis). Unequivocal findings on MRI or diskography will determine which treatment is indicated. The contrast agent will remain in the intervertebral space, being held within it by the annulus fibrosus.
In a covered extrusion (Fig. 1.6, no. 3; Fig. 1.19), only those intradiskal procedures may be used that can also reach the subligamentous or submembranous portions of the displaced disk tissue delineated by the flow of contrast agent. Intradiskal systems employing rigid needles or catheters and those that produce heat (such as lasers) are not suitable for this pathoanatomic situation (3) because the hernia sac is immediately adjacent to the dura mater or a nerve root.
Intradiskal procedures are contraindicated in an extrusion with perforation of the annulus fibrosus and the posterior longitudinal ligament or anterior epidural membrane. Percutaneous diskectomy and intradiskal laser treatment are ineffective in this situation, and therapeutic agents injected into the disk, such as chymopapain, will enter the epidural space like the contrast agent does and fail to reach the sequestrum in the proper concentration. Additionally, the therapeutic agent may cause injury to the dura mater or nerve roots. Where diskography demonstrates leakage of contrast agent into the epidural space, only the use of cortisone as a crystalloid suspension should be considered. Such a treatment corresponds to an epidural steroid injection.
Prognosis
The clinical symptoms and signs, course, and prognosis of the disorder hinge on whether the displaced disk tissue is still within the disk and will remain there or has already migrated from the intervertebral space into the vertebral canal as an extrusion or sequestrum. Where the annulus fibrosus is intact, all forms of conservative treatment (disk-preserving treatment) are possible. The primary goal in this situation is to relieve impingement on the nerve root by decompressing the root and controlling periradicular inflammation.

Fig. 1.11 Sequestrum (Fig. 1.6, part 5; case study 14)
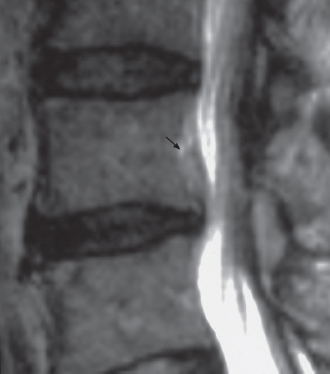
Fig. 1.12 Water-containing extrusion at the supradiskal level (case study 57). The superiorly displaced disk tissue exhibits high signal intensity in the T2 image, indicating high water content (→)
| Sciatica due to disk protrusion | Sciatica due to disk extrusion |
| Gradual onset | Abrupt onset |
| Changing postural abnormality | Constant postural abnormality |
| Proximal pain is most common | Distal pain, paresthesia, paresis |
| Well controlled with medication | Poorly controlled with medication |
| Increased injection pressure with diskography | Decreased injection pressure with diskography |
| Contrast agent remains in intervertebral disk space in diskography | Contrast agent flows into the epidural disk space in diskography and may demonstrate a submembranous hernia sac |
Extruded disk tissue cannot return to the disk space if its diameter is larger than that of the presumed annular perforation. This situation is best explained to the patient with the analogy of toothpaste that has been squeezed out of the tube; it can never go back inside. However, conservative treatment can be successfully employed even in this setting, under several conditions:
— The displaced tissue is of high water content and can shrink by desiccation (Fig. 1.12).
— It is in contact with the well-perfused anterior epidural membrane superior or inferior to the disk and can therefore be more easily resorbed.
— The total mass of tissue amounts to less than a third of the diameter of the vertebral canal.
— The vertebral canal is of normal or greater than normal width.
The symptoms and signs of disk extrusion and protrusion differ in their severity and mode of onset (Table 1.3). Nerve root compression manifests itself gradually when the disk is intact, but the onset of a nerve root syndrome involving a sequestrum in direct contact with the nerve root is abrupt. Here the mechanical compression is aggravated by biochemically induced irritation of the root, because the epidural space is normally devoid of disk tissue. Saal (24), Rydevik (23), and Willburger (33) have demonstrated inflammatory mediators in the intervertebral disk tissue that can cause direct irritation of nerve elements in the vertebral canal.
Nevertheless, the acute pain occurring with extrusion and with a sequestrum in the vertebral canal (Fig. 1.11) is often only temporary. The sequestrated tissue is rapidly broken down by enzymatic action and disappears completely within a few months (11).
This resorption is all the more rapid when the sequestrum consists of nucleus pulposus tissue. Sequestra primarily consisting of portions of the annulus fibrosus or the cartilaginous plates are resorbed more slowly and represent an indication for immediate surgical intervention by virtue of their significant clinical symptoms and signs alone.
Classification of the Lumbar Motion Segments
The system of defining disk, supradiskal, and infradiskal levels and medial, paramedial, and lateral zones within a motion segment (Figs. 1.13 and 1.14) has proven effective in facilitating communication between radiologists and surgeons, especially in describing the location of a lumbar disk extrusion. In local injection therapy, intradiskal therapy, and lumbar disk surgery, it is useful to refer to the segments as the last, second-to-last, and third-to-last, etc., to minimize confusion due to numerical anomalies and transitional vertebrae.
Coronal View (A-P Projection)
The A-P projection provides the best overview of the topography of a lumbar motion segment. Moving from cranial to caudal, reference is made to levels, and from medial to lateral, zones are used. “Motion segment,” or simply “segment,” is the collective designation of two adjacent vertebral bodies and the disk in between.
Levels: The margins of the intervertebral space and pedicle on the anterior wall of the vertebral canal define the levels from cranial to caudal. In the practice of radiology and spinal surgery, the intervertebral disk is the main point of orientation, as it is readily identifiable both on imaging studies and at surgery.
The disk level is defined by the superior end plate and inferior end plate of two adjacent vertebrae.
Above (cephalad to) the disk level is the supradiskal level. This level extends as far as the inferior margin of the pedicle, which corresponds to the middle of the vertebral body. Below (caudal to) the disk level is the infradiskal level. This level extends to the inferior margin of the pedicle of the vertebra inferior to the disk. A cranially dislocated sequestrum lies at the supradiskal level, and a caudally dislocated one lies at the infradiskal level.
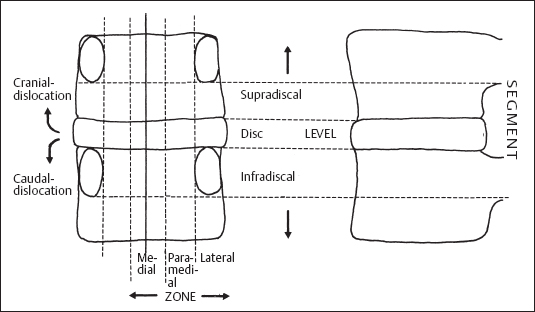
Fig. 1.13 Classification of the lumbar motion segments
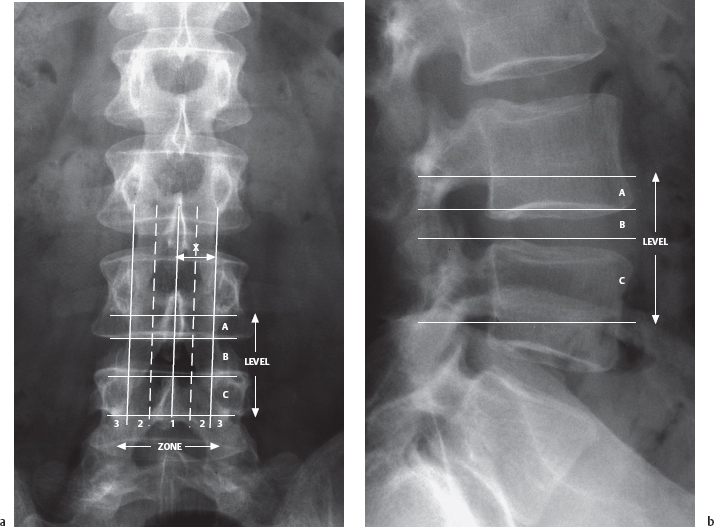
Fig. 1.14a, b A-P (a) and lateral (b) radiographs of the lumbar spine, with the levels indicated: supradiskal level (A), disk level (B), and infradiskal level (C). The A-P radiograph also shows the medial (1), paramedial (2), and lateral zones (3). The paramedial zone is defined as the lateral half of distance x (from the midline to the medial margin of the pedicle); the medial half of distance x on either side of the midline constitutes the medial zone
Zones (Figs. 1.15 and 1.16)
Three zones are differentiated: medial, paramedial, and lateral. The medial zone is divided into right and left halves. The middle of the paramedial zone corresponds to the middle of the interlaminar surgical site after removal of the ligamentum flavum in segments L5-S1 and L4-5. All findings in the immediate vicinity are regarded as paramedial. If they lie closer to the midline, they are regarded as medial; if they lie farther to the outside, they are regarded as lateral. The border line between paramedial and lateral is defined by the medial margin of the pedicle.
The same distinction applies to the superior and infradiskal levels. The medial and paramedial portions of the vertebra lie between the medial margins of the pedicles. The lateral portions of the vertebra (meaning the pedicle itself and zone beneath the pedicle corresponding to the upper portion of the intervertebral foramen) lie lateral to the medial margin of either pedicle. Infradiskal levels do not have lateral zones. The disk level and supradiskal lateral zones correspond to an intraforaminal position.
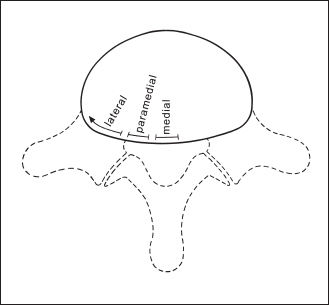
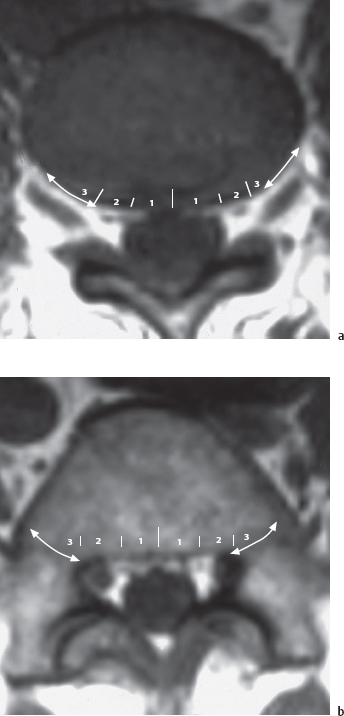
Fig. 1.16 Medial zone (1), paramedial zone (2), and lateral zone (3) in an axial MR image: a disk and supradiskal level, b infradiskal level. The markings in a result from projection of the image over b
Coronal View with Nerve Roots (Figs. 1.17 and 1.18)
A conventional or MR myelogram simultaneously demonstrates the dural sac and the nerve roots arising from it, projected on the A-P view of the vertebral body and intervertebral disk (Fig. 1.18).
In the lower lumbar segments, the roots first cross over the level of an intervertebral disk before passing through the intervertebral foramen at the next lower segment and leaving the vertebral canal. Each lumbar interlaminar window contains two roots. The root crossing over the level of the disk (the “traversing root”) lies in the paramedial zone at the disk level; it is usually affected by the disk level paramedial extrusions and protrusions. The exiting root is lateral, above (cranial to) the intervertebral disk. This exiting root originates in the next higher segment and leaves the vertebral canal beneath the pedicle of the same number. A craniolaterally displaced extrusion can compress the exiting roots in the superior zone beneath the pedicle in the foramen. Extraforaminal extrusions occur farther laterally at the disk level and at the supradiskal level.
Lateral View
Sagittal slices in MRI provide the best view of extruded disk tissue. This tissue will either lie at the disk level or be displaced more or less cranially into the supradiskal level or caudally into the infradiskal level. It is usually possible to identify the parent disk (the disk of origin; Figs. 1.9 and 1.10).
Depending on the imaging plane, the sagittal view may also demonstrate which side is affected. Lateral and craniolateral displacement suggests an intraforaminal location of the sequestrum with compression of the nerve root exiting there (Fig. 1.19).
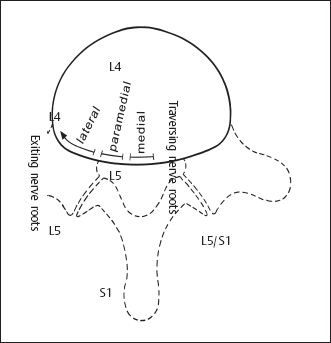
Fig. 1.17 Anteroposterior view of lumbar segments
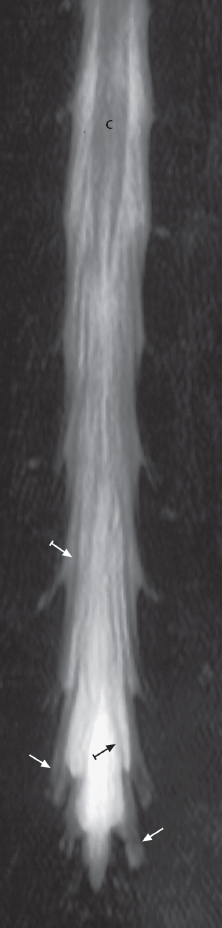
Fig. 1.18 MR myelography (RARE) in an A-P projection. The image demonstrates the dural sac as in myelography, with traversing (↦) and exiting nerve roots (→). C = conus medullaris.
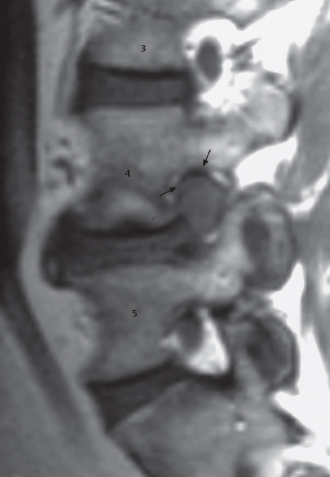
Fig. 1.19 Foraminal extrusion. The nerve roots in the L3-4and L5-S1 foramina can be clearly identified. Foramen L4-5 is completely occluded, and the extrusion compresses nerve root L4 (→) (case study 50)
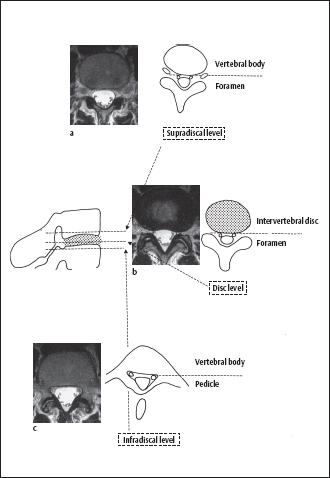
Fig. 1.20a-c Supradiskal level (a), disk level (b), and infradiskal level (c) in an axial (transverse) MR image
Axial View (Fig. 1.20)
The best axial views of lumbar segments are still obtained with CT, although MR images are steadily improving (Fig. 1.20). The ability to identify the disks and vertebral bodies and the specific intervertebral foramen or pedicle makes it possible to determine the level even without a topographic (scout) image. The other posterior elements, such as joints, spinous processes, and transverse processes, are of highly variable appearance and are of little or no assistance in the counting of levels. Scoliosis and a malaligned imaging plane will produce laterally asymmetric images. The axial view of the disk level shows the intervertebral foramen in addition to the intervertebral disk with portions of the superior or inferior end plate that have may been included in the slice.
In the axial slices inferior to the disk, there will be a gradual transition from the vertebral body to the components of the posterior vertebral arch. The site at which the intervertebral foramen is projected at the disk and supradiskal levels will be the site of the lateral recess at the infradiskal level. The lateral recess contains the traversing root next to the pedicle of the same number; thus, the lateral recess of L5 will contain the L5 root. The definition of zones on the axial view (Figs. 1.19 and 1.20) at the various levels corresponds to the definition on the coronal view (Figs. 1.15 and 1.16). The center of the paramedial zone lies between the midline and the lateral margin of the intervertebral disk. This usually corresponds to the center of the surgical exposure in an interlaminar approach. The medial margin of the pedicle in images at the infradiskal level (pedicle image) defines the border with the lateral zone. Medial extrusions and protrusions may be more pronounced on the right or left, and should be so described.
Variations in the Number of Vertebrae and Transitional Vertebrae
Variations in the number of vertebrae in the lumbar spine are clinically significant in the identification of spinal segments. The number of presacral vertebrae without ribs is important. The presence of four ribfree lumbar vertebrae is known as sacralization; the presence of six rib-free lumbar vertebrae is known as lumbarization. A full-spine radiograph is required to determine whether sacralization or lumbarization is present. For this reason, it is best simply to describe transitional vertebrae. Figure 1.21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree