3 Patient-Related Complications In the case of impaired renal function, patients should be treated according to the current European Society of Urogenital Radiology (ESUR) guidelines (http://www.esur.org/esur-guidelines/). Following these guidelines will minimize problems related to uncontrolled iodized contrast media application.1 Patients with known allergic reactions to contrast material should be prepared according to international guidelines.2 The ACR Manual on Contrast Media, Version 10.1, 2015 from the ACR Committee on Drugs and Contrast Media will help in both prevention and treatment of acute reactions to contrast media (http://www.acr.org/quality-safety/resources/~/media/37D84428BF1D4E1B9A3A2918DA9E27A3.pdf/). Practitioners should have extensive knowledge of dose management protocols during endovascular therapy in order to avoid excessive radiation exposure to both the patient and staff.3,4 Strategies for preventing infections during endovascular procedures include general, preoperative, intraoperative, and postoperative regimes. These strategies are important because vascular patients are prone to infection (i.e., in cases of diabetes, chronic wounds, renal impairment, and malignancies responsible for an impaired immunity).5 The Joint Practice Guideline for Sterile Technique during Vascular and Interventional Radiology Procedures from the Society of Interventional Radiology, Association of Perioperative Registered Nurses and the Association for Radiologic and Imaging Nursing, is a particularly useful reference work (http://www.sirweb.org/clinical/cpg/QI35.pdf). Major periprocedural complications are uncommon in interventions, but they may manifest suddenly and require swift and orderly response. Although the experience of the surgeon, nursing, and technical staff is important, the relative rarity of serious events makes the use of a checklist a valuable practice, helping to ensure organized implementation of a preplanned response. “Planning for failure” is a strategy used by effective teams that perform procedures with significant risks. Patel et al (2012) report improved endovascular outcomes with a preprocedural “mental rehearsal” in hybrid aortic cases.6 In 2013, Chen developed a checklist for response to a cerebral artery aneurysm perforation and a separate checklist for thrombosis in neurosurgical interventions.7 These listed expected responses from the surgeon, anesthesiologist, nursing and technologist staff, each with specific roles and responsibilities. In the case of thrombosis, the interventionist should record the activated clotting time (ACT) and request an empiric bolus of heparin based on the patient’s weight and predetermined dose. If vasospasm is detected at the site of the sheath, intra-arterial nitroglycerin should be given. Nursing staffshould administer fluids, and the technologist should prepare aspiration or thrombolysis devices. For bleeding complications, the interventionist should clearly communicate details of the complication to the staffand his or her plans for correction. Serious bleeding from a superficial femoral artery (SFA) intervention is rare, but a high femoral artery puncture or concomitant iliac artery intervention can lead to rapid blood loss into the pelvis. A retroperitoneal hemorrhage can quickly result in shock. Clearly and succinctly articulating the problem and the anticipated next steps is critical, and it is important to verbally confirm that team members have heard and understood what was said. Recognition
3.1 General Complications Related to Endovascular Procedures
3.1.1 Impaired Renal Function
3.1.2 Known Allergic Reactions to Contrast Material
3.1.3 Radiation Exposure
3.1.4 Infection
3.2 Management of Vascular Complications
3.2.1 Thrombosis
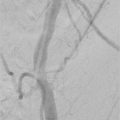
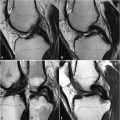
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree