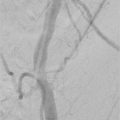
2 Minor and Major Complications Minor complication is defined as a treatment-related adverse event requiring nominal therapy or no treatment with or without overnight hospitalization for observation. 1. No therapy, no consequence. Or, 2. Nominal therapy, no consequence; includes overnight admission for observation only. Major complication is defined as a treatment-related adverse event requiring further therapy with increase in the level of care or prolonged hospitalization. 1. Requires therapy, minor hospitalization (< 48 h). 2. Requires major therapy, unplanned increase in level of care, prolonged hospitalization (> 48 h). 3. Has permanent adverse sequelae. Or, 4. Results in death. Endovascular therapy on the wrong body part, performing inadequate procedures, or even treating the wrong person are all examples of intervention confusion. With regard to all performed procedures, treating the wrong person or body part is rare. When they occur, however, the impact on the patient and on all individuals involved in the care process is momentous. Intervention confusion is generally considered preventable. The aim of standard operation procedure (SOP) is to prevent confusion by implementing and consistently applying the following three complementary steps in the preparation of each patient for endovascular interventions: 1. Preoperative verification process (including patient identification, procedures, site[s], laterality and level, confirmed by source documents, consent form, medical records, and discussion with the patient). 2. Marking the intervention site(s) on the patient. 3. “Team time-out” just prior to the start of the intervention, involving verbal communication by all the professionals involved. It is essential that all members of the pre- and perioperative teams are actively involved and effectively communicate with each other. In addition, it is important to involve the patient as much as possible. A Patient Safety Checklist and knowledge of how to deal with impaired renal function and allergic reactions to contrast media will also help avoid complications.1,2 It is strongly recommended that the patient is prepared according to the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) IR Patient Safety Checklist (Fig. 2.1). The essential points on the checklist will minimize problems of communication and misinformation or any further confusion before starting the procedure. It is of utmost importance to document and store all procedural steps, including fluoroscopic images, especially when they make a significant contribution to the progress of a procedure. In this way, the operator can later highlight these steps in the report after storing the images in the picture archiving and communication system (PACS). The importance of adequate image documentation is emphasized in the following case example: A 48-year-old woman had been undergoing hemodialysis for many years. The patient suffered from recurrent swelling of her face and left arm (the arm with the Brescia-Cimino shunt). Repeated percutaneous transluminal angioplasty (PTA) was performed and the final stent (self-expanding 14 × 40 mm, open-cell design) at the level of the left brachiocephalic vein was placed 6 months ago. A moderate stenosis of the unstented part of the brachiocephalic vein close to the vena cava superior (VCS) was assumed to be responsible for the current symptoms (Fig. 2.2). A direct stenting procedure of the stenosed venous part was performed (self-expanding stent 16 × 40 mm). Unfortunately, the correct stent position was not documented. The stent (closed-cell design) migrated into the VCS (Fig. 2.3) during the removal of the PTA balloon, which was carefully deflated. The patient was asymptomatic and the swelling of the face and arm disappeared completely. However, the operator would have been more satisfied if at least one stored image had documented the initial correctly placed stent.
2.1 Definitions
2.2 Avoiding Complications
2.2.1 Intervention Confusion
2.2.2 Patient Safety Checklist
2.2.3 Periprocedural Documentation
Radiology Key
Fastest Radiology Insight Engine