Fig. 2.1
Normal ultrasound of the spine. Sagittal (a) and axial (b). High-resolution ultrasound image of an infant on prone position. The conus medullaris (arrow), the filum terminale (small arrow) and the cauda equina nerve roots (*)
The position of conus is above the L2-3 disc in a normal term infant. Some accept up to the upper border or midbody of L3 to be within normal limits, if the filum is normal. Ventriculus terminalis is persistent focal dilation of the central canal that is limited to the distal cord. It is a normal variant [3]. If there is question about the position of the conus, placing a radiographic skin marker at the level of the conus under ultrasound guidance and taking a subsequent radiograph of the spine to determine the vertebral level can be performed.
Simple coccygeal dimples or pits, which are shallow, 5 mm or smaller in diameter, located within 2.5 cm cephalad to the anal verge and without any associated suspicious skin lesions, are not associated with an increased risk for spinal dysraphism (Fig. 2.2) [4–6]. No imaging is required for simple coccygeal pits.

Fig. 2.2
Simple coccygeal dimple. Sagittal ultrasound image of the coccygeal region. Hypoechoic line extending from the skin dimple to the distal coccyx. This finding is considered a normal variant and is not associated with spinal dysraphic anomalies
The craniocervical junction can be imaged using the foramen magnum as a sonographic window. It is rarely performed, however it can be used to image the inferior cerebellum and proximal cervical cord [1].
Spinal Dysraphism
Spinal dysraphism is the term used for incomplete fusion of the posterior arch of the vertebrae. Closed spinal dysraphism is covered by skin and in open spinal dysraphism the spinal canal contents are exposed without overlying skin.
Open spinal dysraphism can be of two major types: (1) Myelocele with a flat neural placode (distal end of the cord) exposed and flush with the surrounding skin; (2) Myelomeningocele where the placode is associated with herniated subarachnoid space and meninges. In both the defect is repaired with approximation of the skin within the first 72 h of birth (Fig. 2.3).
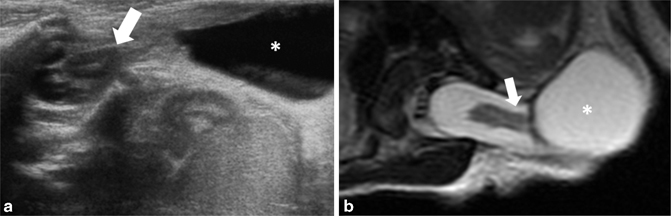
Fig. 2.3
Myelomeningocele. Axial ultrasound (a) and axial T2 MRI weighted image (b). The neural placode (arrows) and the meninges (*) protruding through the spinal dysraphism
Myelomeningocele is virtually always associated with Chiari II malformation. Chiari II malformation involves a small posterior fossa with downward herniation of cerebellar tonsils. In fetal life ultrasound demonstrates the bifrontal skull narrowing called lemon sign and crowding of cerebellum around the brainstem, called banana sign. In the neonate sonographic scanning of the posterior fossa and via the foramen magnum at the craniocervical junction can demonstrate the herniated cerebellar tonsils lying posterior to the upper cervical cord. Repair of the cerebellar herniation is only rarely performed in infancy [3]. The cord remains low in position after tethered cord release and closure of the myelomeningocele . It is very difficult to diagnose secondary tethering due to adhering scar tissue after surgery as the imaging findings overlap normal postoperative appearance. Clinical assessment is of utmost importance when re-tethering is suspected.
A meningocele, whether in the cervical or more commonly lumbosacral region, contains only CSF-filled sac of dura mater without any neural elements. The cord can be tethered to the periphery of the sac. It is not associated with Chiari II malformation. A terminal myelocystocele is a rare condition where the herniated CSF space communicates with the distal spinal canal. It is associated with more proximal cord syrinx. Terminal myelocystoceles are associated with omphalocele, cloacal exstrophy, imperforate anus, and spinal anomalies (OEIS) complex [7].
Closed spinal dysraphism is covered by skin. Also called as occult spinal dysraphism it is not associated with an increase in maternal serum and amniotic fluid Alpha-feto Protein (AFP) levels. Most commonly it manifests as a midline spinal abnormality on physical examination in the newborn. Bifurcation or asymmetry of the superior gluteal crease, skin covered hairy patch, skin tag, subcutaneous mass or lump (lipoma), abnormally pigmented patch, telangectasias, hemangiomas, and high sacral dimples may herald an underlying spinal dysraphic anomaly [4, 8].
Spinal lipoma is the term given to a variety of spinal dysraphisms associated with a fatty component. Lipomyelocele is akin to a myelocele, except that the neural placode is covered by a lipoma that is contiguous with the subcutaneous fat. The neural elements lie within the confines of the vertebral canal (Fig. 2.4). In a lipomyelomeningocele the subarachnoid spaces bulges out of the vertebral canal and pushes the neural placode and the overlying lipoma as well. The nomenclature of these defects can be easily understood as it represents the layer that is first encountered from the dorsal aspect [1].
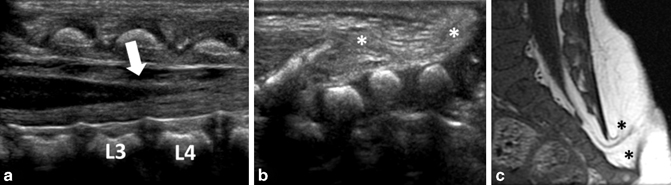
Fig. 2.4
Lipomyelocele. Sagittal ultrasound image (a, b) and sagittal MRI T1 weighted image (c). Low-lying conus medullaris terminating at the level of L4 (arrow) with the distal spinal dysraphism covered by a lipoma that is contiguous with the subcutaneous fat (*)
Intradural lipoma is a lipoma in the subpial location that is typically attached to the dorsal spinal cord. Intradural lipomas occur more commonly in the thoracic spine, followed by the cervicothoracic junction, and may cause symptoms related to cord compression. The intradural lipomas located in the lumbosacral region, intimately related to the filum terminale, are named terminal lipomas and are often associated with tethered cord (Fig. 2.5). Terminal lipomas are frequently associated with sacral hypoplasia, anorectal malformations, genitourinary malformations, and dorsal dermal sinus.
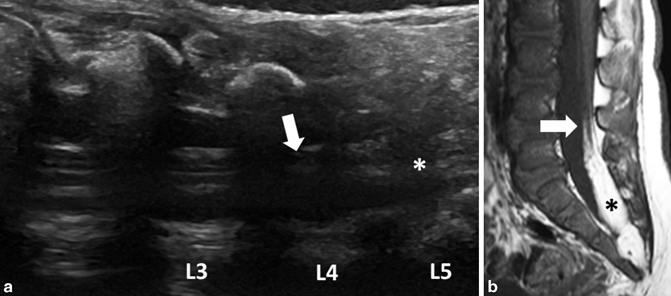
Fig. 2.5
Terminal lipoma. Sagittal ultrasound images of the lumbosacral junction (a) and the sagittal MRI T1 weighted image (b). Tethered cord terminating at the level of the lumbosacral junction (arrow) inseparable from an echogenic mass, consistent with the terminal lipoma seen on MRI T1-weighted image (*)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree