Weight
Tube current (mAs)
Kilovoltage (kVp)
<10
40
80
10–14
50
80
15–24
60
80
25–34
70
80
35–44
80
80
45–54
90
90
55–70
100–120
100–120
Routine pediatric thoracic CT protocols using intravenous iodinated contrast material are sufficient to diagnose the most clinically important chest traumatic lesions. Fast table speed (<1 s), thin detector collimation (<1 mm), and a 1–2 mm reconstruction interval are recommended to allow the creation of isotropic reformatted images as well as three-dimensional volume-rendered images of the aorta and the thoracic cage. CT angiography (either with or without electrocardiogram gating) is the preferable imaging study when there is a high suspicion of aortic pathology [1, 8].
3.2.3 Chest Ultrasound
Emerging indications of ultrasound include the evaluation of pneumothoraces, costochondral and rib fractures, and even pulmonary contusions.
In patients with major trauma, the initial US examination is generally performed with a FAST (focused assessment with sonography in trauma) protocol that is effective in depicting intraperitoneal collections of free fluid that are an indirect sign of solid organ injury and require urgent surgical exploration. After the initial FAST survey, the US examination may be rapidly extended to the thorax to rule out hemothorax and pneumothorax or to guide interventional procedures such as endotracheal intubation. This “extended to thorax” examination is called extended FAST (e-FAST).
In the trauma setting, the FAST examination is usually performed in hypotensive and hemodynamically unstable patients because it helps determine whether immediate surgery is needed before the patient undergoes a CT evaluation; in fact, if an intra-abdominal bleeding is present, the probability of death increases by about 1 % for every 3 min that elapses before surgical exploration [9].
In a meta-analysis by Ding et al. comparing the use of anteroposterior chest radiography with transthoracic ultrasonography for the diagnosis of pneumothorax, pooled sensitivity and specificity were 88 and 99 %, respectively, for ultrasonography and 52 and 100 %, respectively, for CR [10].
As with sonography elsewhere in the body, the appropriate transducers and frequencies vary with the size of the patient and the structure examined. Neonates and small infants are easily examined with high-frequency linear transducers, whereas older children require lower-frequency transducers. Basic B-mode real-time is generally all that is required for chest US. The use of M-mode imaging could be helpful in the evaluation of pneumothorax [11].
Current trends in pediatric imaging support the increased use of ultrasound to decrease radiation exposure. Unfortunately, at this time, ultrasound cannot replace other imaging modalities in the setting of acute pediatric thoracic trauma because of a variety of inherent limitations and its operator dependence. We believe that this imaging method could answer to specific clinical questions during the acute resuscitation period.
3.2.4 Other Imaging Modalities
Catheter-based angiography of the thoracic aorta is performed far less frequently than in the past, as CT angiography has been accepted as an accurate diagnostic tool for the diagnosis of acute aortic injury. It should be used only in cases of equivocal CT findings [12].
Magnetic resonance imaging (MRI) carries major drawbacks in the acute emergency setting such as longer acquisition times, inability to closely observe the patient within the MRI scanner, and prohibition to introduce ferromagnetic devices. For this reason, MRI is rarely indicated in children after thoracic trauma. MRI is commonly indicated in the evaluation of spinal cord lesions in cases of abnormality of the neurologic examination or unexplained severe spinal pain after thoracic trauma [2].
3.3 Radiation Dose Consideration in Pediatric Examinations
A single chest radiograph exposes a patient to a dose of 0.02 millisievert (mSv), whereas a CT of the chest exposes the patient to roughly 8 mSv of ionizing radiation [13].
A retrospective study from Pearce et al. suggests that radiation doses of 50–60 mGy (2–3 head CTs) in children could triple their risk of brain tumors [14].
Children are more prone to radiation-induced cancers and have a longer expected life span than adults. Although there are multiple imaging modalities in the trauma specialist’s arsenal, the use of CT has increased exponentially also in children. Despite this trend, chest radiograph remains an acceptable screening tool to analyze which patients may require CT evaluation.
The ALARA (as low as reasonably achievable) principle aims to balance appropriate use and low-dose imaging with imaging quality; it refers to a campaign to reduce the amount of ionizing radiation exposure by using specialized pediatric protocols and using alternate modalities when possible [13].
Blunt thoracic trauma can result in life-threatening emergencies. CT will frequently be necessary for its high specificity and sensitivity in the detection of thoracic trauma lesions. The concept of ALARA should never be used to withhold a gold standard diagnostic test from a sick child. Chest CT scanning is particularly important in children with chest trauma when hemodynamic instability or respiratory failure requiring intubation develops or when there is persistent drainage of blood or air from chest tubes or a progressive pneumomediastinum.
Alternative imaging modalities to CT, such as MRI and US, should be considered to answer specific clinical questions during the observation period.
3.4 Lung Parenchymal Injuries
3.4.1 Contusion
A major difference between adults and children is the compliance of the chest wall, due to greater elasticity of the ribs. This allows greater deformation of the chest before the ribs fracture. Thus, major internal injuries may occur without any external chest injury.
Pulmonary contusions are the most common finding in pediatric patients after a blunt chest trauma. This condition is the result of the direct impact of adjacent bony structures such as ribs and spine on the lung parenchyma, leading to focal hemorrhage, edema, and/or alveolar collapse.
They are more reliably demonstrated on CT scans as peripherally located ground-glass or consolidative airspace opacities, not always associated to rib fractures; they typically exhibit a thin zone of surrounding subpleural lucency. Most contusions resolve in 2–7 days.
The differential diagnosis includes atelectasis and aspiration pneumonia that are typically located in the dependent portions of the lung and have a segmental distribution.
While in the adults large pulmonary contusions (involving at least 20 % of the lung parenchyma) can lead to acute respiratory distress syndrome, increased need of mechanical ventilation, and increased mortality, in children these injuries do not appear to have the same degree of morbidity [1].
In recent studies, US has been shown in adults to be more sensitive than chest radiography for the diagnosis of pulmonary contusion, with sensitivity and specificity rates of >90 % [16]. Also in children, the relatively high radiation dose associated with CT may be avoided by the use of US (Fig. 3.1).


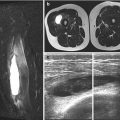
Fig. 3.1
A 14-year-old male with blunt chest trauma. Axial CT image demonstrates left-sided pulmonary laceration (white arrow), left-sided pneumothorax (white arrowhead), and right lower lobe contusions (black arrow)
3.4.2 Pneumatocele
Pneumatoceles are caused by the rupture of the most distal airways resulting from abnormal forces applied to the compliant pediatric chest. They appear as round or oval collections of air and/or blood (hemato-pneumatocele), are usually central and surrounded by lung contusions, and vary in size from a few millimeters to several centimeters [1] (Figs. 3.2, 3.3, and 3.4).
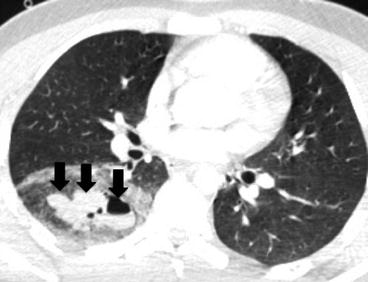
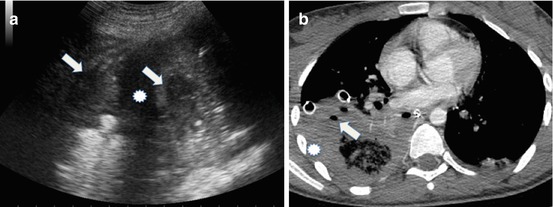
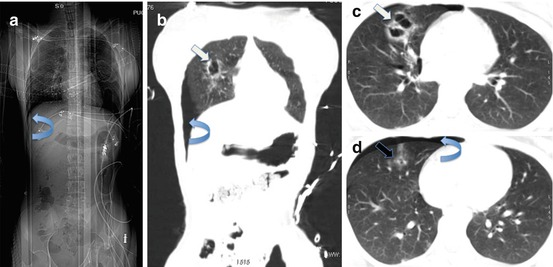
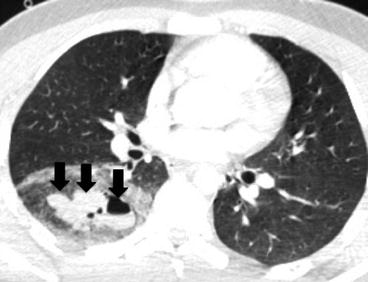
Fig. 3.2
A 13-year-old male with blunt chest trauma. Axial CT image demonstrates right-sided round or oval collections of air and/or blood suggestive of hemato-pneumatocele (arrows). Note that they are central and surrounded by lung contusions
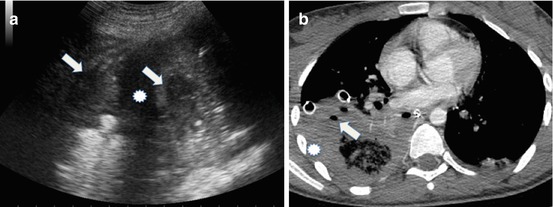
Fig. 3.3
A 12-year-old male with blunt chest trauma. Ultrasonographic scan (a) of the base of the right lung demonstrates multiple fluid collections (arrows in a) and pleural effusion (asterisk). Axial CT image (b) demonstrates right-sided round or oval collections of air and/or blood suggestive of hemato-pneumatocele (arrows in b) and pleural effusion (asterisk). Note the presence of hemothorax
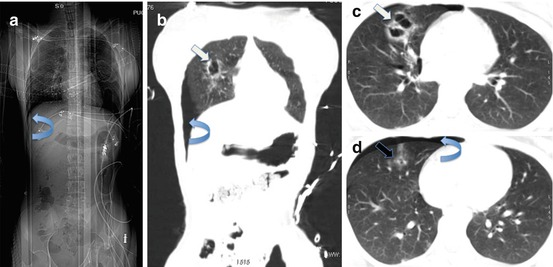
Fig. 3.4
A 14-year-old male with blunt chest trauma. CT scanogram (a) shows the deep sulcus sign (curved arrow in a). Coronal reformatted multidetector-row CT image (b) and axial multidetector-row CT images (c and d) show the presence of pneumothorax (curved arrow in b and d) and right-sided pneumatoceles (white arrow in b and c). A small contusion is also present (black arrow in d)
3.4.3 Laceration
Pulmonary lacerations are derived from penetrating injuries, rib fractures, or compressive shear on the lung at the time of the blunt injury and consist of a disruption of the lung parenchyma. On CT, they appear as linear areas of lucency and are more easily demonstrated on reformatted images (Fig. 3.5).
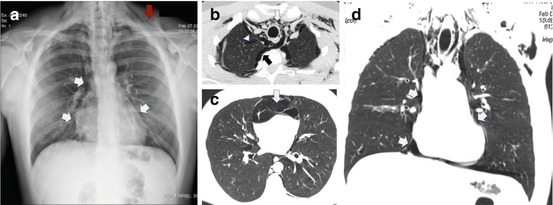
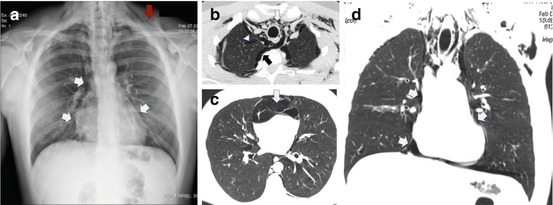
Fig. 3.5
A 14-year-old male with blunt chest trauma. On chest radiograph, (a) note the presence of pneumomediastinum (white arrow) and subcutaneous emphysema (red arrow). Axial CT images (b and c) and coronal reformatted CT image (d) demonstrate the presence of a linear area of lucency in the right upper lobe consistent with parenchymal laceration (white arrowhead in b), extensive pneumomediastinum (white arrow in b–d), right-sided pneumothorax (black arrow in b), and subcutaneous emphysema
Large lacerations involving the pleural surface may cause the development of a bronchopleural fistula.
3.5 Pleural Space Abnormalities
3.5.1 Pneumothorax
Traumatic pneumothorax occurs via blunt or penetrating mechanism. Usually, air enters the pleural space from pulmonary, chest wall, esophageal, or tracheobronchial tree injuries. Rib fractures may not be present in children.
The most concerning adverse outcome of traumatic pneumothorax is progression to a tension pneumothorax. This occurs when the air flows into the pleural cavity without a means of escape, resulting in mediastinal shift, reduced venous blood return to the heart, and a rapid decline in cardiac output. The typical indicators that a pneumothorax is under tension are the mediastinal shift to the contralateral side, depression of the ipsilateral diaphragm, and rapid expansion on serial radiographs.
Pneumothorax occurs in one-third of pediatric thoracic traumas, with the majority of these having associated intrathoracic and extrathoracic injuries and only one-third occurring in isolation. Vital signs and symptomatology depend on the size of the pneumothorax. Patients may present in moderate to severe distress, and tachycardia, hypotension, and oxygen desaturation are also seen [17].
In patients presenting with multiple trauma, an upright chest radiograph cannot be performed. Supine anteroposterior chest radiograph is unreliable at detecting pneumothorax, with a sensitivity of 36–48 % in some studies. Subtle findings include a sharply defined diaphragm or an inferior lung border or cardiac border. Some patients may exhibit the deep sulcus sign, which represents lucency of the lateral costophrenic angle extending toward the hypochondrium and giving the deepened lateral costophrenic angle a very sharp appearance [18, 19].
With the introduction and increased availability of multidetector CT scanners, chest CT has become the reference standard examination in the diagnosis of traumatic pneumothorax.
As expected, CT is more sensitive for small pneumothoraces than chest radiography [20]. Most of this occult pneumothoraces (pneumothoraces not seen on chest radiography) remain clinically silent. However, if the patient undergoes positive-pressure ventilation for any cause, they may enlarge causing cardiorespiratory compromise.
Ultrasound has become more readily available at the bedside in the trauma setting. Several authors have investigated the accuracy of US for the detection of pneumothorax in adult trauma patients and in those who have sustained interventional procedures such as lung biopsy [21]. In a study of Soldati et al., the sensitivity and specificity of chest US in detecting PNX were 92 and 99.4 %, respectively, if compared to CT as the reference standard [22].
In a retrospective study of 368 adult patients with major chest trauma, we found an accuracy of 97.2 % for chest ultrasound in the diagnosis of pneumothorax compared with MDCT and thoracostomy tube placement [23] (Figs. 3.4, 3.5, and 3.6).
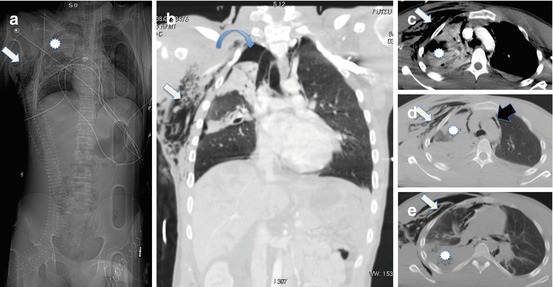
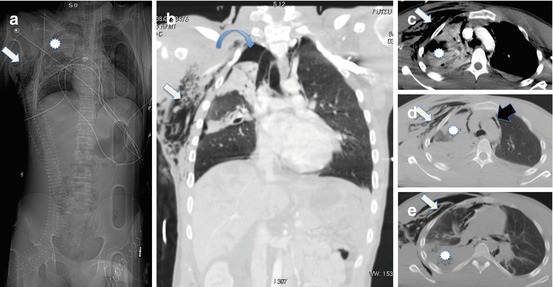
Fig. 3.6
A 15-year-old male with blunt chest trauma. CT scanogram (a), coronal reformatted CT image (b), and axial CT images (c–e) demonstrate the presence of large contusions (asterisk in a, c–e), right-sided pneumothorax (curved arrow in b), subcutaneous emphysema (white arrow in a–e), and pneumomediastinum (black arrow in d)
We believe that ultrasound will play a major role in the evaluation of traumatic pneumothorax in the near future, in children.
3.5.2 Hemothorax, Chylothorax, and Cholothorax
Hemothorax is the result of arterial or venous bleeding into the pleural cavity and occurs in about 13 % of pediatric trauma patients. The vascular injury may be the result of tearing from rapid deceleration or laceration from an adjacent rib fracture. On supine chest radiography, hemothorax manifests as a veillike increased density over the involved hemithorax, often associated to ipsilateral rib fractures. At CT, hemothorax appears as a high-attenuation pleural fluid (between 50 and 80 HU); active contrast extravasation into the pleural space is rarely seen by CT in children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree