Fig. 5.1
Transabdominal ultrasound of the pelvis (B bladder, V vagina, U uterus, R rectum)
However, in the assessment of voiding dysfunction, urinary incontinence and pelvic organ prolapse, the transperineal approach (Fig. 5.2) allows for an easy, non-invasive method of imaging the three compartments of the pelvic floor. Furthermore, there is little distortion of anatomy and patient discomfort because the transducer is placed externally. Transperineal imaging is often conducted with the patient in supine position (Fig. 5.3) but the standing position (Fig. 5.4) can be utilized and is useful for the assessment of incontinence and pelvic organ prolapse.
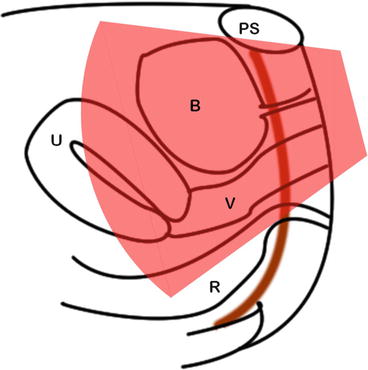


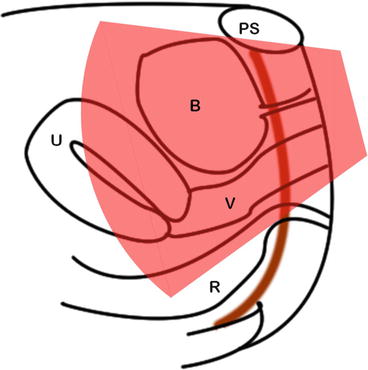
Fig. 5.2
Transperineal ultrasound of the pelvis (B bladder, V vagina, U uterus, R rectum, PS pubic symphysis)

Fig. 5.3
Transducer placement for transperineal (translabial) ultrasound

Fig. 5.4
Transducer placement for transperineal (translabial) ultrasound with the patient standing
Slings and synthetic meshes are easily visible as echogenic structures on ultrasound and transperineal imaging allows for good assessment especially in patients with a failed sling or complications post sling.
For most patients with voiding dysfunction, incontinence and pelvic organ prolapse, 2D imaging is sufficient but 3D imaging has an emerging role in evaluation of prolapse and meshes (see Chaps. 6 and 9).
Use of Ultrasound as the Imaging Modality for Video Urodynamics
Urodynamics are a commonly performed investigation in the evaluation of patients with voiding dysfunction and arguably remain the ‘gold standard’. Traditionally video urodynamics have utilized fluoroscopic imaging. However, not all clinicians have access to radiological equipment and there is the risk of radiation exposure to the patient and occupational exposure to the clinician, as well as the requirement to wear heavy protective garments. Furthermore, depending on the equipment, the patient may have to transfer on and off a fluoroscopy table. This poses difficulty for the elderly or patients with neurologic disease. Ultrasound imaging (by suprapubic and transperineal routes) provides an alternative imaging modality of the lower urinary tract during urodynamics (Fig. 5.5). Transperineal imaging, in particular, allows good visualization of the pelvic floor and arguably provides more information than contrast fluoroscopy in assessment of urinary incontinence and pelvic organ prolapse. This is especially the case if there is mesh or a sling present as these are easily visible on ultrasound. A protocol for using ultrasound as the imaging modality for urodynamics is attached (Tips 5.1).
A Technique of Transperineal 2D Imaging (Tips 5.2)
Indications
Assessment of urinary incontinence, pelvic organ prolapse, and slings/mesh complications.
Equipment
Transperineal (translabial) 2D ultrasound can be performed using standard grayscale ultrasound equipment and the curved array transducer (e.g. 2–5 MHz) used for transabdominal imaging.
Transducer Placement
The transducer is placed on perineum in the sagittal plane (Fig. 5.3) and the image can be orientated according to the preference of the clinician (Videos 5.1 and 5.2). The key anatomic landmarks are pubic symphysis, urethra, bladder, vagina and rectum (Figs. 5.2 and 5.6).
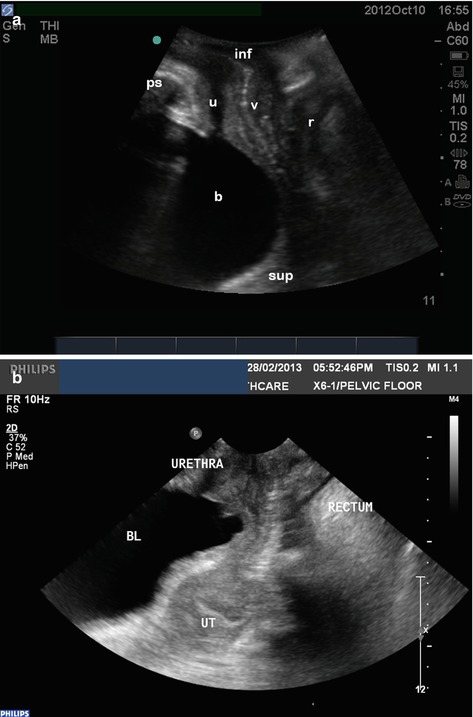
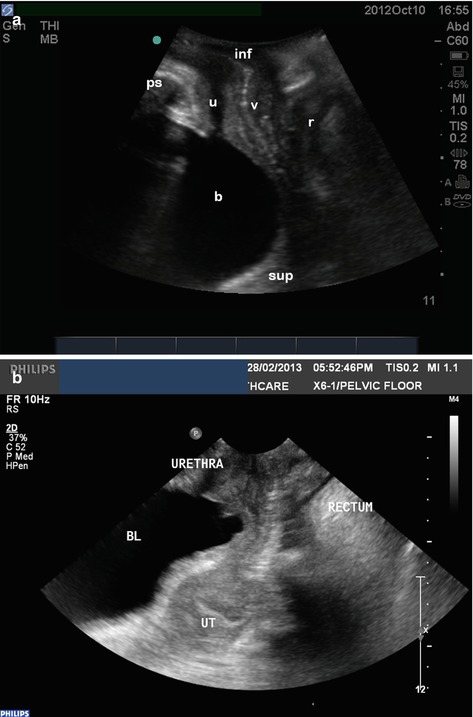
Fig. 5.6
(a, b) Sagittal transperineal ultrasound images demonstrating the three compartments of the pelvis. Bladder (b), urethra (u), vagina (v), rectum (r), pubic symphysis (ps), inferior/caudal (inf), superior/cranial (sup), UT uterus
Scanning Position
Patient can be scanned in the supine or standing positions. It is important to avoid excessive pressure of the transducer against the perineum that may cause discomfort and/or distort anatomy.
Movements of the Transducer
The ‘rocking’ manoeuver allows the field of view to be adjusted covering the compartment of interest (anterior, middle or posterior). It is important to adjust the depth-of-view setting to the region of interest.
Dynamic Imaging
The ability of ultrasound to obtain dynamic imaging information is an important advantage of this modality of imaging in the assessment of the pelvic floor. This should be tailored to the clinical problem, hence the importance of clinician input in performance of scans.
Dynamic assessment during transperineal ultrasound include evaluation of the bladder neck and urethral mobility, pelvic organ prolapse during Valsalva and cough, as well as pelvic floor contractions (Video 5.3). Some of these may be best performed with the patient in the standing position (Fig. 5.4). Dynamic imaging can be incorporated as part of video-urodynamics (see Case 1).
Pelvic floor ultrasound can also be used as an adjunct for pelvic floor physiotherapy. This can be performed via transabdominal or transperineal approaches and is usually performed with some urine in bladder (e.g. about 1–200 ml) but not overfilled. Dynamic 2D imaging can detect pelvic floor contraction/‘lift’ (see Video 5.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree