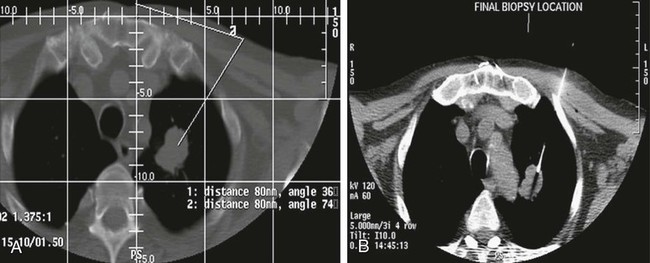
Mark F. Given, Alison Corr, Kenneth R. Thomson and Stuart M. Lyon Percutaneous biopsy of chest lesions is performed for evaluation of focal lung lesions, mediastinal or hilar masses, and pleural or chest wall lesions. This procedure has become an essential part of staging of pulmonary and extrathoracic tumors.1 In the case of lung carcinoma, aspiration biopsy results in a positive diagnosis in 80% to 90% of cases. If a cutting needle is used, a positive diagnosis is expected in up to 95% to 98% of patients unless the lesion is necrotic.2–5 A cutting needle (Fig. 152-1) is generally required for benign lesions, because more material is required to allow use of the special stains necessary for the pathologist to make a definitive diagnosis. The presence of a cytopathologist at the time of biopsy reduces the number of passes needed for diagnosis and avoids the unfortunate necessity for repeat examinations because of an inadequate sample. With computed tomography (CT) guidance, it is possible to perform a biopsy on almost any portion of the chest with a high degree of safety and minimal morbidity because of the ability to plan a needle path such that major vascular structures are avoided (Fig. 152-2). The smallest needle suitable for the biopsy should be used to reduce complications.6 • Severe emphysema. Patients with severe emphysema may not have sufficient lung capacity in the event of pneumothorax and have a higher risk for bronchopleural fistula (forced expiratory volume in 1 second [FEV1] < 1.0 L). • Insufficient lung capacity in the case of unilateral pneumothorax. Patients with extensive fibrosis or other causes of restricted lung capacity may not tolerate pneumothorax. Patients who have undergone pneumonectomy should have an intercostal tube placed before the biopsy. • Bleeding diathesis (international normalized ratio [INR] > 1.5 or platelets < 50,000/mm3). This is a relative risk, and the bleeding tendency should be corrected unless an urgent biopsy is imperative. • Uncooperative patients, including those with an intractable cough. In these patients, development of pneumothorax is a certainty, and a diagnostic specimen may be impossible to obtain. • Positive pressure ventilation, which increases the risk for pneumothorax and bronchopleural fistula. • Pulmonary arterial hypertension when a central biopsy is contemplated. There is an increased risk for fatal hemorrhage if a major central artery is punctured. • Suspected hydatid cyst. Diagnosis of a hydatid cyst is usually made on the preliminary CT scan. There is a possible risk for anaphylaxis if the cyst is intact, but if it has already ruptured, this is debatable. • An appropriate imaging modality (usually a CT scanner but may be a fixed fluoroscopy unit or ultrasound) • Equipment suitable for resuscitation • Aspiration needle (Chiba or Westcott, 20-25 gauge) • Fragment/aspiration needle (20-22 gauge) • Coaxial needle system (19-gauge outer, 22-gauge inner) • Core cutting needle (spring activated, 18-20 gauge) • Cytologist to assess the sample immediately • Microscope, slides, stains, and specimen pots (air and formalin) When it is possible to biopsy a lung lesion percutaneously, a direct vertical approach is preferred, with the skin entry site upright. After the biopsy, the patient is turned so that the punctured side is lowermost to reduce ventilation of that lung and, one hopes, the incidence of pneumothorax. One study comparing conventional treatment with side-down treatment found a reduction in both the pneumothorax rate (41.6% reduced to 12.9%) and the incidence of chest tube requirements (18% reduced to 2.7%).7 • Informed consent, including discussion of the risk for hemoptysis and pneumothorax, must be obtained. Ensure the patient is cooperative enough and can make an effort to not cough after the biopsy. • Anticoagulants, including aspirin, should be discontinued for 3 to 5 days before biopsy. A clotting profile should be obtained in the 24 hours before biopsy. If it is abnormal, fresh frozen plasma, platelets, or vitamin K should be administered as indicated. • If CT is used for guidance, it is helpful to place markers on the skin and obtain scans at a phase of respiration easy for the patient to reproduce. Make sure the display on the screen is being projected in the same-side aspect the patient is being viewed. • If fluoroscopy is used for guidance, the lesion must be visible in two views.
Percutaneous Biopsy of the Lung, Mediastinum, and Pleura
Contraindications
Equipment
Technique
Anatomy and Approach
Technical Aspects
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Percutaneous Biopsy of the Lung, Mediastinum, and Pleura