KEY FACTS
Terminology
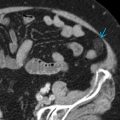
- •
Hemorrhagic collection in perinephric spaces: Subcapsular, perirenal, anterior and posterior pararenal
Imaging
- •
Avascular solid or cystic masses in 1 or more perinephric spaces
- •
Echogenicity of blood changes over time
- •
Sonographic features vary over time
- ○
Acute: Highly echogenic perinephric mass
- ○
Subacute: Partial liquefaction, echogenic debris, retractile clot with thick septa
- ○
Chronic: May be almost anechoic
- ○
- •
Useful to assess perfusion in compressed kidney
- •
Sometimes reveals etiologies such as pseudoaneurysm
Top Differential Diagnoses
- •
Lymphoma infiltration
- •
Cystic lymphangioma
- •
Perinephric abscess
Pathology
- •
Causes include trauma, renal biopsy, renal cyst or tumor rupture, anticoagulation, aneurysm rupture
Clinical Issues
- •
Treatment varies with etiology
- •
Hematoma without underlying significant pathology usually resolves spontaneously
- •
Flank pain, often severe, palpable mass, shock
- •
Diminished hematocrit may prompt evaluation
- •
Subcapsular hematoma may cause hypertension due to renin-angiotensin-aldosterone cascade (Page kidney)
Scanning Tips
- •
Look for underlying malignancy, which can often be cause of spontaneous perinephric hematoma
- •
Use power Doppler to show perinephric hematoma is avascular and to distinguish from adjacent renal cortex
- •
Perinephric fat in diabetic patients (often hypoechoic) may mimic perinephric hematoma; compare with contralateral side to demonstrate bilaterality
- •
When gain is too low, hypoechoic hematoma may be missed; when gain is too high, echogenic hematoma may be missed