How to Image Nerves
- •
Coils and patient position: High-resolution images of the small peripheral nerves require the use of phased array surface coils. The large sciatic nerve can be evaluated without a surface coil, but better resolution is possible if surface coils are used. Positioning of the patient is determined by which nerve is being evaluated. Generally, the nerve can be imaged with the same surface coils, in the same position, and with the same field of view and section thickness as would be used for the nearby joint.
- •
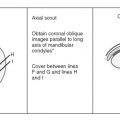
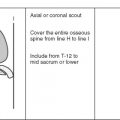
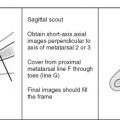
Image orientation: If possible, images of nerves should be obtained in two orthogonal planes. Images that run parallel to the long axis of the nerve (in-plane or longitudinal images) are good for an overview of the course of the nerve and to detect displacement or enlargement. Partial volume artifacts may complicate interpretation of these images, however. Images obtained with the nerve in cross section (perpendicular to the long axis of the nerve) avoid partial volume averaging artifacts and allow for assessment of the size, configuration, signal intensity, and fascicular pattern of the nerve.
- •
Pulse sequences: T1W and some types of T2W fat-suppressed (turbo T2 with fat suppression or STIR) images are best to evaluate the peripheral nerves. T1W images show the anatomy adjacent to the nerve, and T2W sequences are good for showing pathology of the nerve and the fascicular pattern. MR neurography is a specialized technique for depicting the anatomy and course of a nerve similar to how a vessel is displayed on an MR angiogram. The technique requires attention to certain technical details and sophisticated postprocessing of the imaging data. Although the images obtained can be impressive, we do not currently use this technique because of its cumbersome requirements. A few references have been provided, however, for the interested reader.
- •
Contrast: Contrast enhancement is generally of no added value in the evaluation of nerves with the exception of determining whether a mass is cystic or solid.
Normal and Abnormal
BACKGROUND
Electrophysiologic studies are a widely used invasive technique for detecting a conduction abnormality in peripheral nerves. These tests are sensitive, but they lack specificity and cannot show anatomic detail that would delineate the precise location of an abnormality, which often affects treatment planning. Microsurgery for repair of damaged nerves has gained acceptance, and a means of documenting the presence and extent of a nerve abnormality by direct visualization in a noninvasive way before surgery has value.
MRI is the best imaging technique available at this time to evaluate peripheral nerves. Given its ability to display directly the anatomy and course of a nerve and any compressive lesion or other adjacent pathology, MRI has proved to be a useful, complementary adjunct to electromyography. Additionally, if a nerve is difficult to assess directly on a given scan, abnormal signal intensity within the muscles it supplies is important, indirect evidence of nerve pathology.
Nerves are present on every MRI examination of an extremity, and it is important to be aware of the normal and abnormal appearances of peripheral nerves to be able to offer differential diagnoses for the findings.
NORMAL ANATOMY AND MRI APPEARANCE
The fundamental unit of a peripheral nerve is the axon, which may be either myelinated or unmyelinated, and which carries efferent (motor) or afferent (sensory) electrical impulses. Peripheral nerves have a mixture of myelinated and unmyelinated axons. A myelinated fiber exists when a single axon is encased by a single Schwann cell; unmyelinated fibers result if a single Schwann cell encases multiple axons. Layers of Schwann cells form the myelin sheaths.
Large peripheral nerves have three connective tissue sheaths that support and protect the axons and myelin sheaths ( Fig. 4-1 ). The innermost sheath is the endoneurium, which invests each individual myelinated axon. Several axons, along with their Schwann cells and endoneurial sheaths, are bundled together into fascicles that are each wrapped in a dense sheath of perineurium, which serves as a protective barrier to infectious agents or toxins. The third layer is the epineurium, which surrounds the entire peripheral nerve and protects the axons during stretching forces on the nerve. The connective tissue sheaths cannot be detected with MRI; nerve fascicles are the smallest units of nerves that currently can be identified.

Variable amounts of fat are present between fascicles, with more being present in nerves of the lower extremities than in nerves of the upper extremities. Large peripheral nerves contain about 10 fascicles. Each fascicle is composed of motor, sensory, and sympathetic fibers.
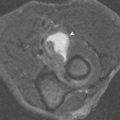
MRI shows normal nerves as round or oval in cross section ( Fig. 4-2 ). The rodlike fascicles in the nerves are seen end on in transverse images as a stippled or honeycomb-like appearance, called a fascicular pattern . The fascicles are uniform in size and similar to, or slightly hyperintense to, muscle on T2W images. On T1W images, the fascicles are similar in signal intensity to muscle with intervening areas of relatively high signal similar to fat (see Fig. 4-2 ). The fascicular pattern is much easier to detect on T2W than on T1W images, especially in small nerves ( Fig. 4-3 ).


Large nerves, such as the sciatic nerve, may have a striated appearance when imaged longitudinally (resembling strands of hair or spaghetti), with signal intensity typical of fat separating the fascicles (see Fig. 4-2 ). Nerves are easy to identify if they are surrounded by fat; however, if they lie adjacent to muscle, without intervening fat, they can be difficult to detect. T2W images in the axial plane give the best chance of identifying and following the nerve in the latter situation.
ABNORMALITIES OF NERVES
Peripheral nerves can be affected by trauma, compression or encasement by an adjacent mass or infiltrative process, nerve entrapment syndromes, nerve sheath tumors, inflammatory neuritis, radiation, hereditary hypertrophic neuropathies, and inflammatory pseudotumors. Nerve problems are evaluated on MRI by directly imaging the nerve and looking for abnormalities in position, size, or signal intensity, and by looking for abnormalities that would indicate denervation in the muscles supplied by the nerve ( Fig. 4-4 ).

Nerves are abnormal if they have diffuse or focal enlargement or diffuse or focal high signal intensity on T2W images. Determining if the signal intensity is too high is a subjective exercise. Alteration in the fascicular pattern also may occur in an abnormal nerve (see Fig. 4-4 ). Fascicles in an abnormal nerve may be difficult to identify, even if enlarged or hyperintense. A nonuniform pattern of fascicles results, which is also virtually always accompanied by increased signal intensity in the nerve on T2W images. Nerves have limited ways to appear abnormal on MRI, and the findings are usually nonspecific, requiring a differential diagnosis, but MRI still adds significant information that can help in the management of patients ( Box 4-1 ).
Primary Signs (Nerve)
- •
Increased size
- •
Increased signal, T2
- •
Abnormal position (displacement) due to mass, subluxation, osteophyte
- •
Fascicular pattern abnormal (nonuniform, enlarged)
Secondary Signs (Muscle)
- •
Denervation of muscle supplied by nerve
- •
<1 yr: high signal in muscle on T2 from intramuscular edema
- •
>1 yr: high signal in muscle on T1 from fat infiltration
- •
Traumatic Nerve Injury
Neurologic symptoms may be present after a nerve injury from disruption of axonal conduction, but the nerve remains intact (neurapraxia). MRI generally is not performed in this setting.
More severe trauma to nerves can result in partial or complete transection of the nerve. With an acute injury, MRI can show the precise location of the nerve abnormality because of the presence of high signal intensity edema on T2W images, and it can show the site of nerve disruption. The nerve may respond by forming a neuroma within the first year after the injury, which is sometimes painful.
Trauma to a nerve may result in a focal neuritis with nerve swelling and surrounding soft tissue edema in the acute setting; this appears as focal nerve enlargement with intraneural and perineural high signal intensity on T2W MR images ( Fig. 4-5 ). Enlargement of the nerve can be recognized by comparing the caliber from proximal to distal because it should gradually decrease in size as images progress distally. Similarly, if both sides of the body are imaged (eg, in the spine or pelvis), a side-to-side comparison can be helpful for recognizing pathologic enlargement ( Fig. 4-6 ).


Additionally, when a peripheral nerve is severely injured, the muscles it serves undergoes denervation changes, which manifest on MR images as high signal intensity (“edema”) on fat-saturated T2W images in the acute to subacute phases, and fatty atrophy (high signal on T1W images) later if the nerve does not regenerate. The detection of these signal abnormalities within muscles served by one nerve is a useful secondary sign of probable nerve injury, and the specific nerve can be evaluated more closely ( Fig. 4-7 ).