Peripheral Artery Disease
Patients may present with acute or chronic lower extremity arterial insufficiency. Chronic lower extremity arterial insufficiency is typically secondary to atherosclerosis. Atherosclerosis is a gradual, degenerative disease where plaque accumulates in the wall of the artery and typically causes gradual, progressive clinical manifestations. However, plaques may become unstable and result in acute ischemic symptoms as well. The two primary risk factors for chronic lower extremity arterial occlusive disease are tobacco use and diabetes mellitus. Tobacco use leads to plaque formation in the aortoiliac, femoral-popliteal, and infrapopliteal arterial segments; significant aortoiliac atherosclerosis is uncommon without a history of tobacco use. Diabetes leads to plaque formation in the femoral-popliteal and infrapopliteal arterial segments, frequently with severe involvement of the tibial and pedal arteries. Other less common causes of chronic lower extremity arterial insufficiency include popliteal artery entrapment syndrome, cystic adventitial disease, thrombosed femoral and popliteal aneurysms, and chronic aortic dissection.
Chronic lower extremity arterial occlusive disease may be asymptomatic, particularly in sedentary patients who have well-developed collateral arterial networks.
The mildest symptom of chronic lower extremity arterial occlusive disease is claudication, which is pain in the large muscle groups (gluteus, thigh, and/or calf) with walking. In claudication, the arterial supply is adequate to meet the resting demands of the lower extremity tissues but inadequate to meet the increased metabolic demands of the exercising muscle. The pain is manifested in any or all of the large muscle groups distal to the culprit arterial stenosis or occlusion. The pain typically is reproducible every time the patient walks a given distance at a given gait; the pain may occur earlier and/or be more severe if the patient walks up an incline or at a faster pace. The pain should rapidly resolve with rest.
The next level of symptomatic presentation of chronic lower extremity arterial occlusive disease is ischemic rest pain. With ischemic rest pain, the arterial supply is inadequate to meet even the minimal resting metabolic demands of the lower extremity nerves. The pain is located in the feet, particularly the toes and forefoot. It is worsened with elevation and improved with dependency. It is severe and unrelenting.
The most severe symptom of chronic lower extremity arterial occlusive disease is ischemic tissue loss, either ulceration or gangrene. With ischemic tissue loss, the arterial supply is inadequate to maintain viability of the skin. The tissue loss is frequently on the toes, which are at the distal limits of the arterial tree, or on areas subject to friction and pressure, including the skin over the metatarsal heads and heel ( Fig. 26.1 ).

Ischemic rest pain and tissue loss are considered critical limb ischemia , as progression to major amputation is likely without arterial reconstruction. Claudication is a relative indication for arterial reconstruction; critical limb ischemia is an absolute indication to arterial reconstruction.
Acute lower extremity arterial insufficiency most commonly is secondary to thromboembolization, with the heart being the most common source. Conditions that may predispose to formation of thrombus in the heart include atrial fibrillation; acute transmural myocardial infarction; and ventricular wall hypokinesis, akinesis, or dyskinesis. The thoracic aorta may also be a source of arterial thromboemboli. Other conditions that may result in acute lower extremity ischemia include acute aortic dissection, traumatic injury, disruption of atherosclerotic plaque, and thrombosis of femoral or popliteal aneurysms.
Clinical manifestations of acute lower extremity arterial insufficiency include pain, pallor, paresthesia, paralysis, and cold temperature ( Fig. 26.2 ). Temperature demarcation is typically at one segment distal to the arterial occlusion: occlusion of the popliteal artery bifurcation leads to a cold forefoot; occlusion of the femoral artery bifurcation leads to a cold distal calf and foot; and occlusion of the iliac artery bifurcation leads to a cold distal thigh, calf, and foot. Numbness and motor dysfunction are ominous signs; without prompt revascularization, permanent pain and paralysis or major amputation is likely.

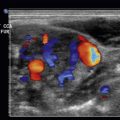
Pseudoaneurysms occur when there is disruption of the wall of an artery, with contained but persistent blood flow into the soft tissues surrounding the artery. Most pseudoaneurysms are traumatic, with iatrogenic trauma being a more common etiology than violent trauma. Anastomotic pseudoaneurysms develop when an arterial anastomosis breaks down, most typically due to the sutures pulling through the wall of the artery. Pseudoaneurysms may cause pain from irritation of local nerves, swelling from compression of adjacent veins, thrombosis of the parent artery, or pressure necrosis of the overlying skin and fat.
Arteriovenous fistulae may be congenital or acquired. Congenital fistulae are frequently complex, with multiple connections between the artery and vein. Acquired fistulae are secondary to trauma, either iatrogenic or violent. Acquired fistulae typically involve a single connection between the vein and artery. Arteriovenous fistulae are usually asymptomatic, but may cause swelling of the affected extremity, ischemia of the affected extremity, or high-output heart failure.
Normal Anatomy
The abdominal aorta bifurcates into the common iliac arteries at about the level of the umbilicus. In the midpelvis, the common iliac artery bifurcates into the internal and external iliac arteries. The internal iliac artery gives blood supply to the gluteal muscles, the organs of the pelvis, and the adductor muscles of the thigh. The external iliac artery provides flow to the lower extremity.
As it crosses deep to the inguinal ligament, the external iliac artery becomes the common femoral artery. The common femoral artery bifurcates into the deep and superficial femoral arteries. The deep femoral artery dives deep to the adductor longus muscle, medial to the femur; it supplies blood to the remaining muscles of the thigh. The superficial femoral artery courses deep to the sartorius muscle and through the adductor canal of the adductor magnus muscle. The superficial femoral artery is the conduit carrying blood to the leg.
After the superficial femoral artery exits the adductor canal, it becomes the popliteal artery. The popliteal artery passes posterior to the knee, between the heads of the gastrocnemius muscle. The popliteal artery bifurcates into the anterior tibial and tibioperoneal (posterior tibial) arteries at the distal edge of the popliteus muscle. The anterior tibial artery crosses the interosseous ligament and travels through the anterior compartment of the leg and, as it crosses the ankle, becomes the dorsal pedal artery on the medial dorsum of the foot. The tibioperoneal (posterior tibial) artery bifurcates in the midleg into the peroneal and posterior tibial arteries, both of which are located in the deep posterior compartment of the leg. The peroneal artery is more lateral, running along the fibula, and ends in the distal leg. The posterior tibial artery runs more medially, crosses posterior to the medial malleolus, and terminates in the plantar foot as the lateral and medial plantar arteries ( Fig. 26.3 ).

Imaging
Duplex ultrasound is accurate in the analysis of the lower extremity arteries. Color flow imaging is helpful to identify the arteries quickly and to identify segments of occlusion and reconstituted flow. Transducer frequencies of 2 to 3 MHz are ideal to evaluate the aorta and iliac arteries, and of 5 MHz for the lower extremity arteries. A Doppler angle of 60 degrees is optimal. B-mode images and spectral analysis of pulsed Doppler data should be obtained at all levels.
Imaging of the aorta and iliac arteries may be limited by overlying bowel gas; ideally, the patient should fast 8 to 12 hours before evaluating the arteries of the abdomen and pelvis.
With the patient supine, the aorta is imaged from just inferior to the xyphoid to the umbilicus, with a 2- to 3-MHz transducer, in a longitudinal plane. The aortic bifurcation is evaluated with the transducer angulated obliquely on the left side of the umbilicus. The distal common iliac and proximal external iliac arteries are visualized with the transducer angled medially at the level of the iliac crests.
A 5-MHz transducer pointed cephalad at the groin is used to evaluate the distal external iliac artery, and then the transducer is moved distally along the thigh to evaluate the common, deep, and superficial femoral arteries. The distal superficial femoral and popliteal arteries may need to be evaluated with the transducer on the posterior thigh and popliteal fossa; this may be accomplished by flexing the patient’s knee or placing the patient in the prone position.
The anterior tibial artery is located at the dorsum of the ankle and then followed up the anterolateral leg. The posterior tibial artery is identified posterior to the medial malleolus and then followed up the medial leg. The peroneal artery is located posterior to the lateral malleolus and then followed up the posterolateral leg.
Pathology
Chronic Lower Extremity Atherosclerosis
The diagnosis of chronic lower extremity atherosclerosis is typically made on the basis of the history (claudication, rest pain, foot ulceration, or gangrene) and physical examination (pulse deficits, bruits, skin changes, etc.). In the presence of diagnostic uncertainty, measurement of the blood pressure at the ankle and/or toes and/or calculating an ankle–brachial index is typically sufficient to confirm or exclude the diagnosis of chronic lower extremity atherosclerosis. Duplex ultrasound is rarely needed in the diagnosis. Duplex ultrasound is indicated when a more precise assessment of the arterial anatomy is needed, such as treatment planning or surveillance after prior treatment.
A normal arterial Doppler signal in a lower extremity artery will have a triphasic signal with a brisk systolic upstroke ( Fig. 26.4A ). The first phase, with antegrade acceleration and deceleration, is due to contraction of the left ventricle ( Fig. 26.4B–E ). The second phase, with retrograde flow, is due to reflection of the pressure wave off the distal resistance arteries. The third phase, with brief antegrade flow, is due to elastic recoil of the aortic root. As the aorta becomes stiffer with age, the third phase may be lost; a biphasic signal in an artery of the lower extremity may be normal in an elderly individual ( Fig. 26.5 ).



The normal peak systolic velocity decreases from the proximal to the distal arteries of the lower extremity. The peak systolic velocity in the iliac arteries is typically about 120 cm/sec, and in the popliteal artery about 70 cm/sec, but the values vary substantially from patient to patient.
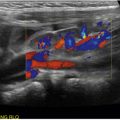
Stenosis is diagnosed primarily by an increase in the peak systolic velocity at the level of stenosis; a doubling or tripling of the peak systolic velocity usually correlates with a >50% diameter stenosis ( Fig. 26.6 ). With a severe stenosis, peak systolic velocities may decrease and resistance increase proximal to the stenosis ( Fig. 26.7 ). Turbulence is commonly seen immediately distal to the stenosis, and the distal waveforms may become monophasic ( Fig. 26.8 ). Plaque in the wall and luminal narrowing may be seen on B-mode or color flow imaging ( Fig. 26.9 ), but peak systolic velocity elevation is the most reliable criterion to diagnose stenosis.




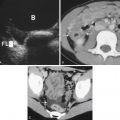
Occlusion is diagnosed by the absence of flow in the artery; waveforms distal to the occlusion typically are monophasic with low peak systolic velocity ( Fig. 26.10 ). Heavy calcification of the arterial wall, commonly seen in patients with diabetes and/or renal failure, may limit the ability of the ultrasound waves to penetrate the arterial wall and may lead to an erroneous diagnosis of arterial occlusion ( Fig. 26.11 ).