PET and PET-CT in Kidney Tumors and Bladder Cancer
Hossein Jadvar
Peter S. Conti
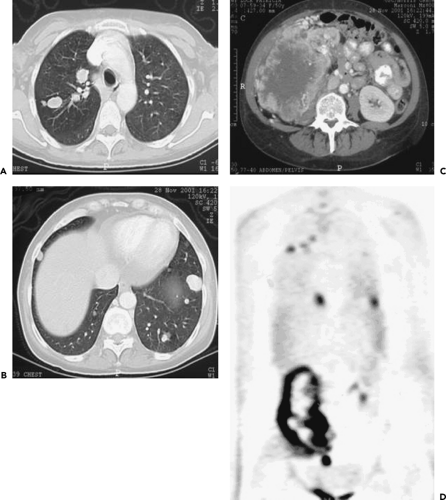
The role of positron emission tomography (PET) and integrated PET and computed tomography (CT) in the diagnosis and follow-up of renal cell carcinoma (RCC) is not clear, and the literature is controversial. The reason for this is twofold. RCC is not always a fast-growing tumor and thus may not result in high fluorodeoxyglucose (FDG) avidity, and FDG is excreted through the kidneys; thus contrast of potential tumor to background is lacking. Procedures to “rinse” the kidneys (e.g., by giving furosemide) should be used, but it has not been clearly demonstrated that this is advantageous. As with many tumors, FDG-PET is probably best for the detection of distant disease. Use of FDG-PET(-CT) should probably be restricted to staging of suspected metastatic disease and to monitor therapy effects when toxic drug regimens are applied (see Fig. 47.1). The situation with bladder cancer is similar in that local tumor manifestations are also obscured by the high FDG activity in the bladder. The use of FDG-PET and PET-CT in bladder cancer should be as restrictive at this time point as for RCC.
Renal Cancer
Renal cell carcinoma (RCC) arises from the renal tubular epithelium and accounts for most adult kidney tumors. The tumor is highly angioinvasive and results in widespread hematogenous and lymphatic metastases especially to the lung, liver, lymph nodes, bone, and brain. Metastases are present in about 50% of patients at initial presentation. Radical nephrectomy is the main treatment for the early stages of disease, although palliative nephrectomy may also be performed in advanced disease with intractable bleeding. Solitary metastasis may also be resected. RCC responds poorly to chemotherapy. Radiation therapy for RCC is used for palliation of metastatic sites, specifically, bone and brain. Immunotherapy with biologic response modifiers such as interleukin-2 and interferon alpha has the most impact on the treatment of metastatic disease. The 5-year survival may be as high as 80% to 90% for early stages of disease, although advanced disease carries a poor prognosis (1).
Current imaging tests, including computed tomography (CT), magnetic resonance imaging (MRI), and skeletal scintigraphy are not sufficiently accurate to detect recurrent and metastatic disease. Preliminary studies of positron emission tomography (PET) imaging of RCC with fluorodeoxyglucose (FDG) have revealed a promising role in the evaluation of indeterminate renal masses, in preoperative staging and assessment of tumor burden, in detection of osseous and nonosseous metastases, in restaging after therapy, and in the determination of the effect of imaging findings on clinical management (2,3,4,5,6,7,8,9,10,11,12) (Fig. 47.1). However, other FDG-PET studies have demonstrated less distinctive results and no advantage over standard imaging methods (13,14). Moreover, there is currently little experience with PET-CT in the evaluation of kidney masses, but as with the imaging evaluation of other cancers, PET-CT will likely provide valuable information on exact tumor localization, on definition of disease extent, and in avoiding potential pitfalls (e.g., urine in renal pelvis).
A relatively high false-negative rate has been reported with FDG-PET in the imaging evaluation of RCC when compared with histologic analysis of surgical specimens (14,15). Other studies have reported high accuracy in characterizing indeterminate renal masses with a mean tumor-to-kidney uptake ratio of 3.0 and average and maximum standardized uptake values (SUVs) of 7.9 ± 4.9 and 6.0 ± 3.6, respectively (4,16). The superiority of FDG-PET in detecting metastases as compared with CT and bone scintigraphy has also been shown (15,17,18). In a recent retrospective investigation of 66 patients with known or suspected RCC who had undergone both conventional and FDG-PET imaging evaluations, PET exhibited the following diagnostic performance: for primary tumor, sensitivity of
60% and specificity of 100% (compared with 92% sensitivity and 100% specificity for abdominal CT); for retroperitoneal lymph node metastases and renal bed recurrence, sensitivity of 75% and specificity of 100% (compared with 93% sensitivity and 98% specificity for abdominal CT); for metastatic lung disease, sensitivity of 75% and specificity of 97% (compared with 91% sensitivity and 73% specificity for chest CT); and for bone metastases, sensitivity of 77% and specificity of 100% (compared with 94% sensitivity and 87% specificity for combined CT and bone scan) (14).
60% and specificity of 100% (compared with 92% sensitivity and 100% specificity for abdominal CT); for retroperitoneal lymph node metastases and renal bed recurrence, sensitivity of 75% and specificity of 100% (compared with 93% sensitivity and 98% specificity for abdominal CT); for metastatic lung disease, sensitivity of 75% and specificity of 97% (compared with 91% sensitivity and 73% specificity for chest CT); and for bone metastases, sensitivity of 77% and specificity of 100% (compared with 94% sensitivity and 87% specificity for combined CT and bone scan) (14).
FDG-PET can also alter clinical management in up to 40% of patients with suspicious locally recurrent and metastatic renal cancer (14,19). In a recent study of the utility of FDG-PET in restaging RCC, a sensitivity of 87% was reported at a specificity of 100% (20). In another report of the diagnostic performance of FDG-PET in restaging RCC, a sensitivity of 71%, specificity of 75%, accuracy of 72%, negative predictive value of 33%, and positive predictive value of 94% were noted (21). A recent study reported positive and negative predictive values of 100% and 67%, respectively, for detection of distant RCC metastases (22). Therefore, FDG-PET appears to offer modest diagnostic accuracy in restaging and in detecting metastatic disease in RCC. A negative study may not exclude disease, whereas a positive study is highly suspicious for malignancy (21,23).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree