PET and PET-CT of Testicular Cancer
Thomas F. Hany
Klaus Strobel
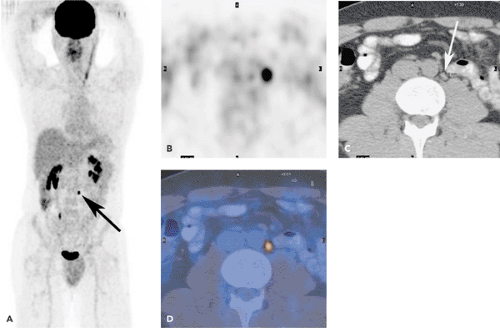
Testicular cancer consists of two general groups: seminomatous and nonseminomatous testicular cancers. Very much as in staging of other tumors, fluorodeoxyglucose (FDG) positron emission tomography (PET) of testicular cancer results in the detection of local and distant metastases and may allow for a more accurate staging than morphologic imaging modalities (see Fig. 48.1). FDG-PET is used not only in staging but also for restaging of testicular cancer. Well-differentiated teratomas are regarded as one of the few histologies in which FDG-PET is not useful because it does not show any FDG avidity. The introduction of integrated PET and computed tomography (CT) may improve the diagnostic accuracy in FDG-avid tumors owing to better differentiation from physiologic accumulations, especially in the retroperitoneum and pelvic region.
Introduction
In testicular neoplasms, two groups have to be differentiated: seminomatous and nonseminomatous testicular cancers. Essentially, tumors with a histologic mixture of seminoma and nonseminoma cell types should be managed as nonseminomas. Nonseminomas include embryonal carcinoma, teratoma, yolk sac carcinoma, and choriocarcinoma as well as various combinations of these cell subtypes. A tumor that appears to have seminoma histology but that has elevated serum levels of alpha fetoprotein (AFP) should be treated as nonseminoma. Elevation of the beta human chorionic gonadotropin (beta-hCG) alone is found in approximately 15% of the patients with seminoma.
In testicular cancer, the initial staging procedures are usually performed after surgical excision and histologic workup of the primary tumor (Fig. 48.1). Surgical staging procedures as well as morphologic imaging studies have been used extensively for staging and restaging of disease. Fluorodeoxyglucose (FDG) positron emission tomography (PET) holds substantial promise in the staging as well as restaging of these tumors. In PET-alone imaging, the lack of anatomic landmarks may hamper the diagnostic efficacy, since physiologic uptake of 18FDG is seen in the kidneys and ureters.
Testicular Cancer Subtypes
Testicular cancer is a well-treatable, often curable cancer that develops in young and middle-aged men. Germ cell tumors (GCT) are the most frequent solid tumors in men between the ages of 20 and 35 years. GCT are categorized histologically into two major subgroups: seminomatous and nonseminomatous testicular cancers.
Seminomas represent 50% of all GCT and are the most common tumors in individuals with undescended testes. Elevated human chorionic gonadotropin (hCG) is present in 15% to 20% of tumors. Seminomas are sensitive to radiation and chemotherapy. For all stages of seminoma combined, the cure rate exceeds 90% (1,2).
Nonseminomatous GCT are mostly mixed cancers, consisting of two or more cell types. The presence of any nonseminomatous cell type is responsible for the prognosis and management decisions. Embryonal cell carcinoma is the most important component of mixed testicular tumors and
the most aggressive GCT. Choriocarcinoma is usually associated with widespread hematogenous metastases and high levels of hCG. Teratomas consist of cell types from more than one germ cell layer (mature, immature, with malignant transformation). Although a mature teratoma may be histologically benign, it is derived from a totipotential, malignant precursor cell. Therefore, a teratoma in a postpubertal male must be considered to be a malignant GCT. PET/CT can also be used for staging of extragonadal GCT (Fig. 48.2).
the most aggressive GCT. Choriocarcinoma is usually associated with widespread hematogenous metastases and high levels of hCG. Teratomas consist of cell types from more than one germ cell layer (mature, immature, with malignant transformation). Although a mature teratoma may be histologically benign, it is derived from a totipotential, malignant precursor cell. Therefore, a teratoma in a postpubertal male must be considered to be a malignant GCT. PET/CT can also be used for staging of extragonadal GCT (Fig. 48.2).
Diagnostic Procedures and Treatment in Testicular Cancer
Diagnostic evaluation of retroperitoneal lymph nodes at the level of the kidneys is an important aspect of treatment planning as well as restaging in adults with testicular cancer. Lymphatic spread of testicular cancer is typically along the spermatic veins. These veins are discharging into the left renal vein and inferior vena cava on each side, respectively. Therefore, the typical localizations of the initial distant metastases by lymphatic spread are at the level of the kidneys in the retroperitoneum. Further organs of distant metastases of hematogenous spread are the lungs and liver (Fig. 48.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree