PET-CT and SPECT-CT of Malignant Bone Tumors
Janet F. Eary
Bone sarcomas present a number of diagnostic and treatment challenges. These tumors occur most frequently in older children and young adults, but present in almost every age group. Younger patients generally have better prognoses than adults. Although many of this varied group of tumors have classic appearance on plain x-ray and computed tomography (CT) examinations, their biologic assessment for malignant potential remains an important problem for patient diagnosis and treatment planning. The most common bone sarcomas are osteosarcomas, which occur primarily in the extremities. Although needle or incisional biopsy can provide an accurate histologic diagnosis for treatment planning, sampling errors can result in an error of tumor grade designation or description of histologic type.
Positron emission tomography (PET) imaging using fluorodeoxyglucose (FDG) is currently being evaluated in bone sarcoma diagnosis and patient treatment response assessment. Studies are showing that it can be used to distinguish low-grade from high-grade tumors and to assess whether there is tumor recurrence. As a whole-body imaging technique, it can easily identify synchronous tumor as in the case of Ewing sarcoma and metastases from other tumor types can easily be identified. Figure 51.1 shows some examples of bone sarcoma appearance on FDG-PET. The tumor uptake is usually intense, and the extent of tumors is easily distinguished. The use of PET and single-photon emission computed tomography (SPECT) in benign bone tumors is discussed in Chapter 65.
Introduction
Similar to the soft tissue sarcomas (see Chapter 53), malignant bone tumors constitute a heterogenous group and originate from mesenchymal tissues. They arise in bony or cartilage tissue and may have variable calcification and soft tissue extension at presentation. Osteosarcoma and the Ewing sarcoma family of tumors (ESFT), which include peripheral neuroectodermal tumors (PNET), are important childhood cancers and account for approximately one third of them. Adult bone tumors may include the same diagnoses, although adults are more likely to present with osteosarcoma and chondrosarcomas. Generally, younger patients have overall better outcomes than adults with bone and cartilage tumors. Newer limb salvage surgical procedures have enabled the current generation of patients to have excellent functional results after resection and treatment (1,2). Positron emission tomography (PET) imaging experience has contributed to characterization of these tumors and patient follow-up. The use of PET and single-photon emission computed tomography (SPECT) in the diagnosis of benign bone tumors is discussed in Chapter 65.
Osteosarcoma
Background
These tumors have a peak incidence in the second decade of life, with very few patients younger than 10 years of age or older than 50 years of age (3). Most osteosarcomas are present in the extremities, with 15% to 20% of patients presenting with pulmonary metastases (the main site). Occasional metastases are present in the bone, lymph nodes, and brain. Osteosarcomas are metaphyseal tumors. Risk factors for osteosarcoma include prior radiation therapy (3% of tumors), germ line retinoblastoma gene (Rb) mutation, germ line p53 mutations, and Rothmund-Thomson syndrome. Other associations with osteosarcoma have been described for growth abnormalities, trauma, fetal x-ray exposure, fluoride in water, and parental x-ray exposure. Table 51.1 shows the frequency for occurrence at different sites of primary osteosarcomas. Patients with metastatic disease have a significantly worse prognosis (4). There are many subtypes of osteosarcomas. Table 51.2 lists the histologic types of osteosarcoma and their frequencies of occurrence. They are classified according to the French or FNCLCC grading system for sarcomas (5).
The classic osteosarcomas are treated with neoadjuvant chemotherapy. Standard chemotherapy consists of intensive use of doxorubicin, cisplatin, and high-dose methotrexate. Prognostic factors at presentation include the presence of metastases and the presence of chemotherapy resistance. Five-year survival, depending on the level of chemotherapy resistance, is 60% to 80%. Survival for this period without chemotherapy is closer to 50%. Postresection treatment may include radiation therapy to the tumor bed and likely includes additional chemotherapy. This later aspect of treatment is included if there was significant tumor response to neoadjuvant chemotherapy (prior to resection). The low-grade types are treated with wide resection and typically only recur in 5% of cases. Five-year survival is high unless a degeneration to a higher-grade malignant process takes place in a local recurrence.
Table 51.1 Osteosarcoma Primary Tumor Sites | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Table 51.2 Bone Tumor Histologic Types | |
|---|---|
|
Patient Evaluation
This process consists of a standard, careful patient assessment for the presence of malignancy and ability to tolerate chemotherapy for patients with high-grade tumors. To characterize the primary tumor site, plain film, magnetic resonance imaging (MRI), and computed tomography (CT) are usually performed. A whole body bone scan and chest CT scan are performed to detect lung metastases.
Patients also receive a hearing test to determine baseline function before possible ototoxicity from cisplatin. Renal and liver function at baseline also are assessed to help monitor likely toxic effects of chemotherapy.
Patients also receive a hearing test to determine baseline function before possible ototoxicity from cisplatin. Renal and liver function at baseline also are assessed to help monitor likely toxic effects of chemotherapy.
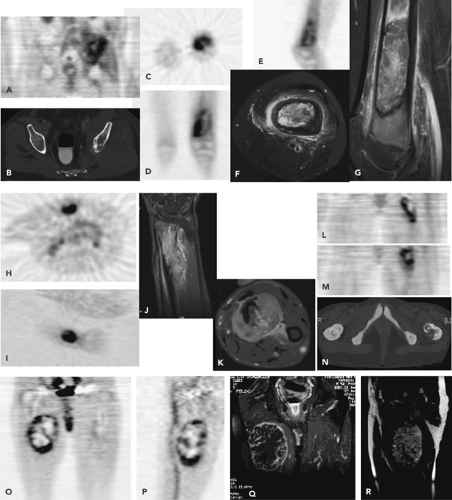 Figure 51.1 FDG-PET bone sarcoma examples. These display the heterogeneity in tumor uptake and skeletal locations of these tumors. Primary osteosarcoma in the left pelvis (A,B) in a coronal PET (A) and on axial CT (B), showing bone destruction. Telangiectatic osteosarcoma in the left distal femur (C–G). Diagnostic FDG-PET (C: axial; D: coronal; and E: sagittal views) and MRI images (F: axial; G: sagittal) show heterogeneity. The areas with less uptake on FDG-PET images are likely necrotic. Fibroblastic osteosarcoma in the wrist (H–K). This is a small tumor with relatively homogenous uptake in PET (H: axial; I: coronal), although MRI (J: coronal; K: axial) shows more complexity. This later aspect is likely owing to tumor edema. Leiomyosarcoma of bone in the left proximal femur (L–N), showing bony destruction on CT (L) and intense FDG activity on two coronal sections (M,N). Parosteal osteosarcoma in the right proximal femur. Diagnostic FDG-PET (O,P) and MRI images (Q,R). The FDG uptake pattern shows it to be a highly heterogenous tumor.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




