Chapter Outline
Careful use of descriptive terms aids in the radiologic analysis of perceived abnormalities. By describing the radiographic characteristics of a lesion, a radiologist can localize the lesion to the mucosa, bowel wall, or tissue extrinsic to bowel. This radiographic description, in conjunction with the site and size of the lesion, age of the patient, and clinical history, enables the radiologist to make a specific diagnosis or formulate a graded differential diagnosis of the most likely possibilities. In addition, precise use of descriptive terms enhances communication between the radiologist and clinician. A radiologist should be able to describe an abnormality so that the person reading or listening to the radiographic report can visualize the lesion without looking at the images.
This chapter is a pictorial glossary that visually defines common descriptive terms in gastrointestinal radiology. The terms are divided according to whether they refer to mucosal lesions, wall lesions (i.e., submucosal, intramural, or extramucosal ), or extrinsic lesions.
Surface Patterns
Villous Pattern
The villi of the small intestine are at the radiographic limits of resolution. Some villi may be seen if the mucosa is well coated and slightly magnified. This villous pattern is manifested as barely perceptible radiolucencies surrounded by barium in the interstices between villi ( Fig. 3-1 ).

Reticular Pattern
The term reticular means netlike ( Fig. 3-2 ). This net is formed by barium in the interstices of normal columnar mucosa, such as the areae gastricae of the stomach (see Fig. 3-2A ), or in the interstices of a mucosal lesion, such as a carpet lesion. The intervening radiolucent mucosa may be round, ovoid, or polygonal. A reticular pattern typically occurs in abnormalities arising in columnar mucosa. For example, a reticular pattern is seen in the columnar metaplasia of Barrett’s esophagus or in a colonic urticarial pattern (see Fig. 3-2B ).

Granularity
Granularity implies subtle elevation of the mucosal surface seen en face as small radiolucencies in the shallow barium pool or as punctate dots of barium between lucencies ( Fig. 3-3 ). The “granules” are barely perceptible elevations, with indistinct borders, as if salt had been sprinkled on a plate. Granularity implies mucosa elevated by edema, inflammatory exudate, or tumor. Barium flocculated on an inflamed mucosal surface can mimic a granular mucosa.

Nodularity
Mucosal nodules are relatively well-circumscribed elevations seen en face as round to ovoid radiolucencies in the barium pool or as small rings etched in white ( Fig. 3-4 ). In profile, nodules are seen as small hemispheric or sharp-edged elevations of the contour. Nodules may arise in the mucosa itself, lamina propria, or adjacent submucosa. If a mucosal nodule involves a bowel fold, especially the rugae of the stomach or valvulae conniventes of the small bowel, the fold is eccentrically enlarged. Submucosal nodules involving a bowel fold, seen en face, symmetrically splay the parallel surfaces of the fold. Mucosal nodularity may be described as fine or coarse. The distinction between fine nodularity and mucosal granularity is somewhat arbitrary, although mucosal nodules are generally larger and more discrete than granules.

Shaggy
Shaggy describes such severe mucosal disease that it is difficult to distinguish ulcerated mucosa from sloughed epithelium and inflammatory detritus ( Fig. 3-5 ). In profile, the contour is jagged. En face, numerous lines reflect barium filling the interstices between ulcerated mucosa and debris. Shaggy is frequently used to describe the radiographic findings in severe Candida esophagitis (see Fig. 3-5 ) and ulcerative colitis.

Cobblestoning
Transverse and longitudinal fissuring of the mucosal surface with extension of knifelike clefts into the submucosa and muscularis propria results in cobblestoning, typically seen in Crohn’s disease ( Fig. 3-6 ). The cobblestones appear as a carpet of nodules on the luminal surface. The cobblestones represent residual tissue between the transverse and longitudinal clefts.

Fold Patterns
The folds in the gastrointestinal (GI) tract are composed of mucosa—epithelium, lamina propria, and muscularis mucosae—and submucosa. When a radiograph demonstrates enlarged or nodular folds, the process therefore involves the mucosal or submucosal layers, or both. A desmoplastic process involving the serosa or adventitia of the bowel or the adjacent mesenteric or omental fat can secondarily pull on the bowel wall so that the smooth mucosal surface is thrown into an abnormal fold pattern.
Striae
When a viscus is less than fully distended, transverse striations may be seen perpendicular to the longitudinal axis of the bowel. Examples of this phenomenon include the so-called feline esophagus, gastric striae ( Fig. 3-7 ), and innominate grooves of the colon.

Web
A web is a thin band of mucosa (with or without submucosa) that traverses a variable portion of the intestinal lumen. Webs vary from small shelflike lesions to hemispheric bars and circumferential rings ( Fig. 3-8 ). Webs may be normal variants or the sequelae of inflammatory disease.

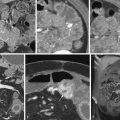
Coil Spring Sign
If barium is forced between one loop of bowel intussuscepting into another loop, the barium may coat the mucosal folds of the outer loop. The result is the radiographic appearance of concentric rings of barium said to resemble a coil spring ( Fig. 3-9 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree