Laryngeal carcinoma is a devastating malignancy that severely affects patients’ quality of life, with compromise of ability to talk, breathe, and swallow. Accurate tumor staging is imperative, because treatment plans focus on laryngeal conservation therapy whenever possible. Although the mucosal extent of tumor and vocal cord mobility is best assessed with endoscopic evaluation, cross-sectional imaging is essential for accurate T-staging, because only cross-sectional imaging can assess the submucosal extent of the tumor, cartilage invasion, and extralaryngeal spread. This article reviews topics crucial for interpreting imaging studies of patients with laryngeal squamous cell carcinoma.
Key points
- •
Laryngeal carcinoma is a devastating malignancy that severely affects patients’ quality of life, with compromise of ability to talk, breathe, and swallow.
- •
Accurate tumor staging is imperative, because treatment plans focus on laryngeal conservation therapy whenever possible.
- •
Although the mucosal extent of tumor and vocal cord mobility is best assessed with endoscopic evaluation, cross-sectional imaging is essential for accurate T-staging, because only cross-sectional imaging can assess the submucosal extent of the tumor, cartilage invasion, and extralaryngeal spread.
- •
This article reviews topics crucial for interpreting imaging studies of patients with laryngeal squamous cell carcinoma.
Laryngeal carcinoma is a devastating malignancy that severely affects patients’ quality of life, with compromise of ability to talk, breathe, and swallow. Accurate tumor staging is imperative, because treatment plans focus on laryngeal conservation therapy, whenever possible. Although the mucosal extent of tumor and vocal cord mobility is best assessed with endoscopic evaluation, cross-sectional imaging is essential for accurate T-staging, because only cross-sectional imaging can assess the submucosal extent of the tumor, cartilage invasion, and extralaryngeal spread. This article reviews topics crucial for interpreting imaging studies of patients with laryngeal squamous cell carcinoma (SCC).
Epidemiology of laryngeal SCC
The incidence of laryngeal SCC ranges from 0.3 to 9.8 per 100,000 people annually and represents approximately 1% to 2% of all adult malignancies. Men are affected 3 times more frequently than women, and incidence increases with advancing age, with the median age at diagnosis of 65 years, from 2004 to 2008.
The patient population is similar to that affected by lung cancer, with a strong association with smoking and alcohol use in up to 95% of patients, and reported increased incidence in patients of low socioeconomic status. Other potential risk factors for laryngeal carcinoma include passive tobacco smoke exposure, occupational exposure to chemical irritants, chronic irritation caused by reflux, and possibly viral exposure (see later). Nonsmokers with laryngeal SCC are uncommon but tend to be older and the primary subsite is more often glottis, compared with smokers with SCC.
Laryngeal neoplasms are associated with human papillovirus (HPV) infection, particularly with benign laryngeal papillomatosis, most often associated with the low-risk HPV subtypes, HPV 6 and 11. Patients with laryngeal papillomatosis have an approximately 2% risk of developing laryngeal malignancy, particularly if the patient is diagnosed as an adult. The association of HPV infection with the development of SCC has not been well established, and this contrasts with oropharyngeal cancers, in which the clinical significance of and association with the development of SCC and HPV infection have been well documented. There is a broad range of prevalence of HPV infection in laryngeal carcinoma in the literature, present in up to 25% of patients on meta-analysis, with malignancy most commonly associated with the high-risk subtypes 16 and 18. However, the clinical significance and implication of these infections are unclear at this time and require further investigation.
Epidemiology of laryngeal SCC
The incidence of laryngeal SCC ranges from 0.3 to 9.8 per 100,000 people annually and represents approximately 1% to 2% of all adult malignancies. Men are affected 3 times more frequently than women, and incidence increases with advancing age, with the median age at diagnosis of 65 years, from 2004 to 2008.
The patient population is similar to that affected by lung cancer, with a strong association with smoking and alcohol use in up to 95% of patients, and reported increased incidence in patients of low socioeconomic status. Other potential risk factors for laryngeal carcinoma include passive tobacco smoke exposure, occupational exposure to chemical irritants, chronic irritation caused by reflux, and possibly viral exposure (see later). Nonsmokers with laryngeal SCC are uncommon but tend to be older and the primary subsite is more often glottis, compared with smokers with SCC.
Laryngeal neoplasms are associated with human papillovirus (HPV) infection, particularly with benign laryngeal papillomatosis, most often associated with the low-risk HPV subtypes, HPV 6 and 11. Patients with laryngeal papillomatosis have an approximately 2% risk of developing laryngeal malignancy, particularly if the patient is diagnosed as an adult. The association of HPV infection with the development of SCC has not been well established, and this contrasts with oropharyngeal cancers, in which the clinical significance of and association with the development of SCC and HPV infection have been well documented. There is a broad range of prevalence of HPV infection in laryngeal carcinoma in the literature, present in up to 25% of patients on meta-analysis, with malignancy most commonly associated with the high-risk subtypes 16 and 18. However, the clinical significance and implication of these infections are unclear at this time and require further investigation.
Anatomy and boundaries of the larynx
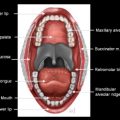
The larynx is a mucosa-lined tube that is responsible for phonation and airway protection. The laryngeal structural framework is composed of the thyroid, cricoid, and arytenoid cartilages; ligaments connecting the cartilaginous framework; and a series of 7 separate paired intrinsic laryngeal muscles, surrounded by fat-containing spaces and lined internally by squamous epithelial mucosa.
The superior border of the larynx is the free edge of the epiglottis, dividing it from the oropharynx, and the inferior extent is to the lower border of the cricoid cartilage. Posteriorly, the larynx is separated from the hypopharynx by the aryepiglottic (AE) folds. The larynx is divided into supraglottic, glottic, and infraglottic (or subglottic) components ( Fig. 1 A).
The supraglottic larynx extends from the tip of the epiglottis (lingual and laryngeal surfaces) and AE folds superiorly to the apex of the laryngeal ventricle (see Fig. 1 B, C). The supraglottic larynx can be subdivided into suprahyoid and infrahyoid regions, divided by the hyoid bone, and the suprahyoid epiglottis contains the free edge of the epiglottis. The petiole of the epiglottis is another term for the base of the infrahyoid epiglottis, at its attachment with the thyroid cartilage (overlying the thyroepiglottic ligament) ( Fig. 2 A). The subsites of the supraglottic larynx, therefore, include the epiglottis (suprahyoid and infrahyoid components), the AE folds, the arytenoids, and the false vocal cords. The AE folds sweep down laterally from the epiglottis and extend to the arytenoid cartilages, and contain 2 small prominences, which denote the location of the cuneiform and corniculate cartilages. The corniculate cartilage may be seen on imaging perched on top of the arytenoid cartilage; however, the cuneiform cartilage is often too small to resolve (see Fig. 2 B). The lateral aspect of the AE folds forms the medial wall of the piriform sinus, actually part of the hypopharynx. On axial cross-sectional imaging, the false vocal cords are at the level of the adjacent paraglottic fat ( Fig. 3 A). The interarytenoid space forms the posterior border of the larynx, dividing it from the hypopharynx.
The glottic larynx is composed of the true vocal folds, extending from the apex of the lateral ventricle (the inferior boundary of the supraglottic larynx and the superior margin of the true vocal fold) to the inferior margin of the true vocal folds (the beginning of the subglottic larynx). The glottis should be an area 1 cm in height, extending caudal to the plane of the mid ventricle (see Fig. 1 B, C). The subsites of the glottic larynx include the anterior and posterior commissures and the right and left true vocal cords.
Histologically, the vocal fold has a surface of stratified squamous epithelium, and beneath the epithelium is the lamina propria, formed of 3 layers. The most superficial layer, Reinke space, can be crucial for transoral laser resections. Beneath Reinke space are the intermediate and deep layers of the lamina propria, which make up the vocal ligament. The true vocal cord is made up of the epithelial layer, Reinke space, the vocal ligament (a thin fibrous band medially within the free margin of the vocal fold, extending the full length of the cord from the vocal process of the arytenoid cartilage to the anterior commissure), and the thyroarytenoid muscle, which also forms the vocalis muscle medially. The anterior commissure is the site of attachment of the vocal ligaments to the thyroid cartilage, via Broyles ligament. The area of anterior attachment is devoid of perichondrium and relatively vulnerable to early cartilaginous invasion. The posterior commissure is the posterior space between the vocal cords, at the vocal process of each arytenoid cartilage.
On axial cross-sectional imaging, the true vocal cord level is identified by the lack of adjacent submucosal fat and the presence of all 3 cartilages (thyroid, cricoid, and vocal process of the arytenoid cartilages) in 1 cross-sectional image (see Fig. 3 B).
The subglottic larynx extends from the inferior margin of the true vocal cord (approximately 1 cm below the laryngeal ventricle anteriorly), through the inferior border of the cricoid cartilage (see Fig. 1 B, C). On axial cross-sectional imaging, the immediate subglottic mucosa is usually smooth, thin, and symmetric, without any significant soft tissue between the cricoid cartilage and the air column (see Fig. 2 C). Any abnormal soft tissue in the subglottic lumen should raise the possibility of tumor extension. Subglottic tumor is difficult to assess endoscopically and is important for the radiologist to detect, because it will impact treatment planning and prognosis.
The preepiglottic space is a pyramid-shaped (in the sagittal plane) or C-shaped (in the axial plane), fat-containing, potential space anterior to the epiglottis, extending superiorly to the hyoid bone. It is bordered posteriorly by the infrahyoid epiglottis and anteriorly by the thyrohyoid membrane and anterior and superior lamina of the thyroid cartilage. Cranially, the preepiglottic space is bounded by the hyoepiglottic ligament and caudally by the petiole of the epiglottis. Inferiorly and laterally, the preepiglottic space is contiguous with the paraglottic space. Both spaces are important potential paths of submucosal tumor spread from both laryngeal and oropharyngeal tumors and cannot be identified on clinical examination, and involvement by tumor will upstage the lesion. Although this space can easily be seen in the axial plane, the preepiglottic space is best evaluated in the sagittal plane, on both reformatted contrast-enhanced computed tomography (CE-CT) and sagittal T1-weighted magnetic resonance (MR) imaging ( Fig. 4 ).
The paraglottic space is a paired, fat-filled potential space, between the mucosa and laryngeal cartilage framework, and is contiguous superiorly with the preepiglottic space. The paraglottic space is mostly fat containing at the level of the supraglottis, surrounding the laryngeal ventricle, and contains the thyroarytenoid (or vocalis) muscle at the level of the glottis, with a thin sliver of fat laterally deep to the thyroid cartilage. The paraglottic space can be seen in the axial plane but is seen better in the coronal plane on both CT reformations and MR imaging ( Fig. 5 ).
Two thin fibrous structures, the quadrangular membrane and the conus elasticus, are not resolved on imaging but dictate the pattern of tumor spread (see Fig. 1 B). The medial border of the paraglottic space is formed by the quadrangular membrane, a thin fibrous structure just beneath the mucosa of the supraglottic larynx, which gives support to the AE fold, and the conus elasticus inferiorly at the glottis and sublottic level, a thicker fibrous layer that extends inferiorly from the vocal ligament of the true cord and attaches along the upper inner margin of the cricoid cartilage, which becomes the cricothyroid membrane anteriorly.
The thyroid cartilage is a triangular shield-shaped cartilage made of paired edges called the thyroid ala, which may or may not be fused anteriorly. It is connected to the hyoid bone by the thyrohyoid membrane, through which the paired external laryngeal arteries and nerves pierce laterally to provide sensation to the supraglottic larynx for airway protection. The cricoid cartilage is a round, ring-shaped cartilage inferior to the thyroid cartilage, separated from the thyroid cartilage by the cricothyroid membrane. The cricoid is the only complete cartilaginous ring in the airway, is much thicker posteriorly, and provides the foundation for the larynx. The paired arytenoid cartilages are triangular in shape and articulate with the cricoid cartilage via the cricoarytenoid joint, a synovial joint. The vocal process of the arytenoid attaches to the true vocal cord, and its mobility is necessary for phonation.
The thyroid, cricoid, and arytenoid cartilages are made of varying amounts of ossified and nonossified hyaline cartilage. Ossified cartilage appears similar to bone on CT, with a peripheral hyperdense cortex and central hypodense medullary cavity, whereas nonossified bone has an appearance of soft tissue. On MR imaging, ossified cartilage is hypointense peripherally on all sequences (similar to cortical bone), with the medullary cavity similar to fat on all sequences. Conversely, nonossified hyaline cartilage appears intermediate to low signal on both T1- and T2-weighted sequences. On MR imaging, there should be no postcontrast enhancement within the medullary cavity of either ossified or nonossifed cartilage. The trend is toward increased cartilage ossification with advancing age; however, these findings are extremely variable and irregular, often making determination of laryngeal cartilage erosion or penetration by adjacent tumor difficult, particularly on CT ( Fig. 6 ). The epiglottis and vocal process of the arytenoid are composed of yellow fibrocartilage and do not ossify.
Lymphatic drainage
There is often significant and bilateral supraglottic lymphatic drainage to the high jugular nodes (levels II and III). Rarely, supraglottic neoplasms can involve submandibular and retropharyngeal nodes. The subglottic larynx initially may also drain in a cephalad direction, and a characteristic lymph node draining the subglottic region is the node anterior to the cricothyroid membrane, the delphian node ( Fig. 7 ). However, the low subglottic lymphatics drain to the paratracheal and pretracheal lymph nodes (level VI). There is almost no lymphatic drainage of the submucosa of the true vocal cord, but once tumor infiltrates the preepiglottic or paraglottic spaces, there is a higher likelihood of nodal disease.
American Joint Commission on Cancer Staging and Changes from the 6th Edition to the 7th Edition
Clinically, tumors are staged by the tumor-nodes-metastasis (TNM) staging system, a classification system developed by the American Joint Committee on Cancer and used to define treatment and quantify prognosis for patients. The committee periodically updates the staging system, taking into account changes in clinical practice, and the new 7th edition has been in effect since January 1, 2010. Although staging is done primarily via laryngoscopy, imaging is important in staging the deep extent of tumor and nodal and distant disease. Refer to Table 1 for the most recent TNM staging for laryngeal SCC ( Table 1 ).
| Primary Tumor (T) | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| Tis | Carcinoma in situ |
| Supraglottis | |
| T1 | Tumor limited to one subsite of supraglottis with normal vocal cord mobility |
| T2 | Tumor invades mucosa of more than one adjacent subsite of supraglottis or glottis or region outside the supraglottis (eg, mucosa of base of tongue, vallecula, medial wall of pyriformsinus) without fixation of the larynx |
| T3 | Tumor limited to larynx with vocal cord fixation and/or invades any of the following: postcricoid area, pre-epiglottic space, paraglottic space, and/or inner cortex of thyroid cartilage |
| T4a | Moderately advanced local disease. Tumor invades through the thyroid cartilage and/or invades tissues beyond the larynx (eg, trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus) |
| T4b | Very advanced local disease. Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures |
| Glottis | |
| T1 | Tumor limited to the vocal cord(s) (may involve anterior or posterior commissure) with normal mobility |
| T1a | Tumor limited to one vocal cord |
| T1b | Tumor involves both vocal cords |
| T2 | Tumor extends to supraglottis and/or subglottis, and/or with impaired vocal cord mobility |
| T3 | Tumor limited to the larynx with vocal cord fixation and/or invasion of paraglottic space, and/or inner cortex of the thyroid cartilage |
| T4a | Moderately advanced local disease. Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (eg, trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus) |
| T4b | Very advanced local disease. Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures |
| Subglottis | |
| T1 | Tumor limited to the subglottis |
| T2 | Tumor extends to vocal cord(s) with normal or impaired mobility |
| T3 | Tumor limited to larynx with vocal cord fixation |
| T4a | Moderately advanced local disease. Tumor invades cricoid or thyroid cartilage and/or invades tissues beyond the larynx (eg, trachea, soft tissues of neck including deep extrinsic muscles of the tongue, strap muscles, thyroid, or esophagus) |
| T4b | Very advanced local disease. Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures |
| Regional Lymph Nodes (N) | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension |
| N2 | Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension; or in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension; or in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension |
| N2a | Metastasis in single ipsilateral lymph node more than 3 cm but not more than 6 cm in greatest dimension |
| N2b | Metastasis in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension |
| N2c | Metastasis in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension |
| N3 | Metastasis in a lymph node more than 6 cm in greatest dimension |
| Distant Metastasis (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
The primary change in staging of laryngeal carcinoma is the division of T4 lesions into T4a (resectable lesions, with cartilage penetration and/or extralaryngeal spread of tumor) and T4b (unresectable lesions, invading prevertebral space, encasing carotid artery, or invading the mediastinum), leading to development of stage IVA (any T4a primary or any N2 nodal disease), stage IVB (any T4b), and stage IVC (any M1). Additionally, there has been clarification of cartilage involvement and T4 disease. Prior staging systems were vague with regard to cartilage involvement, because patients with any cartilage involvement were potentially overstaged as T4 and underwent laryngectomy. With the current staging system, tumors involving only the inner cortex of thyroid cartilage (previously termed “minor cartilage erosion”) are classified as T3, but through-and-through cartilage penetration (both inner and outer cortex involvement) and/or extralaryngeal tumor spread are classified as T4a.
Treatment trends
The major focus in the management of laryngeal cancer is voice retention. This is precluded when the larynx is functionless or there is aspiration despite working with a speech pathologist. Classic voice preservation operations are the open supraglottic laryngectomy (reserved for those patients with only supraglottic involvement) and the vertical hemilaryngectomy (reserved for patients with lesions predominantly involving one true vocal cord). However, in the past 10 years, there has been a significant decline in the use of open surgery, primarily because of the development of transoral endoscopic laser microsurgery, improvements in radiation therapy, and new combined modality chemotherapy and radiation therapy regimens. Oncologic results, both local control and survival results, are similar to more conventional open surgeries, however, with less morbidity and, overall, improved postoperative function and laryngeal preservation rates. In general, open surgery is now primarily reserved for those patients with persistent or recurrent disease post therapy or for those patients with bulky extralaryngeal extension or cartilage invasion on initial presentation. Specific treatment trends are further discussed with regard to the laryngeal site of involvement.
Site-Specific Evaluation with Imaging
General considerations/pitfalls
The larynx is one of the most difficult organs to image, because the structures are small, it is subject to motion from respiration and swallowing, and early mucosal lesions are difficult to resolve on imaging. Performing thin section images through the larynx (both CT and MR imaging), making every effort to suspend swallowing, and angling the gantry through the plane of the larynx can help with these limitations. Additionally, on CE-CT, delayed imaging after contrast may help improve mucosal enhancement to aid in delineating the extent of tumor.
One of the greatest pitfalls in staging any head and neck cancer is either overstaging or understaging tumors. In the larynx, overstaging may result in unnecessary laryngectomy; however, understaging can result in local treatment failure after radiation ( Table 2 ). A study in 2008 demonstrated a false diagnosis rate for detecting the extent of supraglottic laryngeal cancers, and up to 25% of the time, the tumor was overstaged by imaging. Becoming familiar with the American Joint Committee on Cancer staging system for the different subsites and the common patterns of spread of laryngeal cancer and pitfalls associated with staging will help the radiologist to avoid these mistakes.
| Pitfall | Advice |
|---|---|
| Understaging of a T2 supraglottic tumor as a T1 from failure to recognize BOT extension. | Carefully evaluate the BOT and vallecula on sagittal images. |
| Understaging from failure to recognize paraglottic space involvement | Look for replacement of the fat just above and lateral to the thyroarytenoid muscle on axial and coronal images |
| Overstaging of cartilage invasion on CT | Recognize that there is considerable variability and asymmetry in cartilage ossification on CT. Consider MR imaging for further evaluation. |
| Overstaging of cartilage invasion and extralaryngeal extension on MR imaging | Look for areas isointense in signal to the tumor on T1-, T2-, and fat-suppressed T2-weighted images. Reactive edema will be T2 hyperintense to tumor. |
| Failure to recognize extralaryngeal tumor extension without laryngeal penetration | Carefully evaluate the thyroid notch, thyrohyoid membrane, and thyroaretenoid gaps. Consider MR imaging for further evaluation. |
| Understaging of nodal metastasis by PET-CT | Use intravenous CE-CT along with the PET to evaluate for small abnormal lymph nodes that may be below the resolution of PET or have low FDG uptake as a result of necrosis. |
Supraglottic SCC
Because they are initially clinically occult, supraglottic tumors often present later than glottic tumors and are often large. As with other early laryngeal lesions, the T1 and T2 lesions are often best staged with endoscopy. However, imaging is critical for showing the cranial, caudal, and deep extension of supraglottic SCC. Patterns of extension can be anticipated by knowing common pathways of spread.
Small tumors involving the free edge of the epiglottis may be treated with endoscopic surgery, with conservation of a portion of the supraglottic larynx. However, the radiologist must assess the full extent of the tumor and detect submucosal extension. Superior extension with involvement of the vallecula or base of tongue is extremely important to note, because it will upstage to T2 and will likely alter management. Tumor may reach the base of tongue, and even the extrinsic tongue muscles via extension through the preepiglottic space ( Fig. 8 ). Spread anteriorly along the glossoepiglottic fold, which overlies the hyoepiglottic ligament, results in extension to the vallecula and base of tongue.
Tumors can extend from the suprahyoid epiglottis laterally along the pharyngoepiglottic fold to reach the lateral pharyngeal wall. If there is greater than 2 cm of involvement of the base of tongue, the patient may no longer be a candidate for a supraglottic laryngectomy. Additionally, a patient with any advanced laryngeal tumor (T3 or T4) with greater than 1 cm of extension to the base of tongue may not be considered a candidate for laryngeal conservation therapy, and in the event that the patient is undergoing a total laryngectomy, tumor at the base of tongue will require a more extensive resection, possibly a glossectomy, and reconstruction of the neopharynx.
Both suprahyoid and infrahyoid supraglottic tumors are at risk for involvement of the preepiglottic space, because the epiglottis is a poor barrier to tumor spread. Submucosal involvement of the preepiglottic space by tumor cannot be assessed clinically and involvement will upstage a tumor to T3 status. Preepiglottic space spread is associated with a worse prognosis after radiation and an increased risk of nodal metastasis. Although not precluding a supraglottic laryngectomy, involvement of the preepiglottic space may alter the surgical approach, because the surgeon would likely also apply treatment to the neck. Infiltration of the fat within the preepiglottic space is easy to detect on both CT and T1-weighted MR imaging, in both the axial and sagittal plane, with a reported sensitivity of 100% ( Fig. 9 ).