Thyroid cancer includes several neoplasms originating from the thyroid gland—from indolent and curable histologies of differentiated thyroid carcinoma to aggressive anaplastic thyroid carcinoma. Differentiation of thyroid nodules is problematic on CT and MR imaging unless there is evidence of extrathyroidal extension. Evaluation of regional lymph nodes is often performed clinically or with ultrasound. The retropharyngeal and mediastinal lymph nodes are better evaluated by CT and MR imaging. Nuclear scintigraphy is useful for staging and treatment of distant metastasis in differentiated thyroid carcinoma. PET may have a role in aggressive cancers. Accurate staging affects surgical management and subsequent therapy.
Key points
- •
Thyroid cancer includes several neoplasms originating from the thyroid gland from indolent and curable histologies of differentiated thyroid carcinoma to aggressive anaplastic thyroid carcinoma.
- •
Differentiation of thyroid nodules is problematic on CT and MR imaging unless there is evidence of extrathyroidal extension.
- •
Nuclear scintigraphy is useful for staging and treatment of distant metastasis in differentiated thyroid carcinoma, and PET may have a role in aggressive cancers.
- •
Staging affects surgical management and subsequent therapy.
Introduction and epidemiology
The term thyroid cancer encompasses several neoplasms originating from the thyroid gland. Altogether, cancers of the thyroid gland currently have a yearly incidence of 37,000 in the United States, ranking tenth among solid organ malignancies. There is a strong female predominance. Papillary thyroid carcinoma (PTC) and follicular thyroid carcinoma (FTC) are tumors of the thyroid follicular cells collectively referred to as differentiated thyroid carcinoma (DTC). PTC is the most common thyroid malignancy, comprising approximately 85% of cases, and often has an indolent clinical course with low mortality and high likelihood for cure. There are, however, several other subtypes of PTC based on specific histologic features. The follicular variant has the typical cellular features of nuclear grooves and Orphan Annie eye nuclei, but it predominantly has a microfollicular pattern instead of the branching papilla of typical PTC. The tall cell variant of PTC histologically demonstrates cells that are twice as tall as wide and is associated with worse survival than classic PTC. Similarly, insular carcinoma, which is histologically characterized by solid cell clusters with small follicles similar to pancreatic islets, has a poorer prognosis than classic PTC.
FTC is often difficult to distinguish from benign follicular neoplasms on fine-needle aspiration (FNA). The criteria for malignancy are capsular or vascular invasion. In contrast to PTC, spread to lymph nodes in FTC is uncommon, occurring in only 8% to 13% of cases, with typical spread via hematogenous dissemination and distant metastases in 10% to 15% of patients, even with small primary tumors. Hürthle cell carcinoma is considered a subtype of FTC and is characterized pathologically by mitochondria-rich oncocytes. It has a higher rate of lymph node metastases compared with classic FTC, rarely presents with distant metastases, but has the highest incidence of late distant metastasis. Although the management of the various forms of DTC has many similarities, there are important differences in their diagnosis, treatment, and prognosis. Included in the poorly-differentiated thyroid cancers is medullary thyroid carcinoma (MTC), a tumor of the thyroid parafollicular C cells that secrete calcitonin, and anaplastic thyroid carcinoma (ATC), which is thought to arise from well-differentiated thyroid cancer and portends a significantly worse outcome.
Thyroid nodules are commonly recognized during routine physical examination, but are also increasingly incidentally detected on various imaging examinations including ultrasonography (US), CT and MR imaging. The routine work-up of palpable and incidental thyroid nodules has been reviewed in detail. In general, evaluation includes thorough physical examination of the neck, US for confirmation and characterization, which may identify other thyroid nodules or cervical lymphadenopathy, and FNA for evaluation of suspicious nodules. Appropriate diagnostic evaluation and interpretation is crucial to ensure timely treatment with patients with false-negative FNA eventually found to have higher rates of vascular and capsular invasion, and with a near doubling of 30-year mortality rate when therapy was delayed by more than 1 year from diagnosis.
Introduction and epidemiology
The term thyroid cancer encompasses several neoplasms originating from the thyroid gland. Altogether, cancers of the thyroid gland currently have a yearly incidence of 37,000 in the United States, ranking tenth among solid organ malignancies. There is a strong female predominance. Papillary thyroid carcinoma (PTC) and follicular thyroid carcinoma (FTC) are tumors of the thyroid follicular cells collectively referred to as differentiated thyroid carcinoma (DTC). PTC is the most common thyroid malignancy, comprising approximately 85% of cases, and often has an indolent clinical course with low mortality and high likelihood for cure. There are, however, several other subtypes of PTC based on specific histologic features. The follicular variant has the typical cellular features of nuclear grooves and Orphan Annie eye nuclei, but it predominantly has a microfollicular pattern instead of the branching papilla of typical PTC. The tall cell variant of PTC histologically demonstrates cells that are twice as tall as wide and is associated with worse survival than classic PTC. Similarly, insular carcinoma, which is histologically characterized by solid cell clusters with small follicles similar to pancreatic islets, has a poorer prognosis than classic PTC.
FTC is often difficult to distinguish from benign follicular neoplasms on fine-needle aspiration (FNA). The criteria for malignancy are capsular or vascular invasion. In contrast to PTC, spread to lymph nodes in FTC is uncommon, occurring in only 8% to 13% of cases, with typical spread via hematogenous dissemination and distant metastases in 10% to 15% of patients, even with small primary tumors. Hürthle cell carcinoma is considered a subtype of FTC and is characterized pathologically by mitochondria-rich oncocytes. It has a higher rate of lymph node metastases compared with classic FTC, rarely presents with distant metastases, but has the highest incidence of late distant metastasis. Although the management of the various forms of DTC has many similarities, there are important differences in their diagnosis, treatment, and prognosis. Included in the poorly-differentiated thyroid cancers is medullary thyroid carcinoma (MTC), a tumor of the thyroid parafollicular C cells that secrete calcitonin, and anaplastic thyroid carcinoma (ATC), which is thought to arise from well-differentiated thyroid cancer and portends a significantly worse outcome.
Thyroid nodules are commonly recognized during routine physical examination, but are also increasingly incidentally detected on various imaging examinations including ultrasonography (US), CT and MR imaging. The routine work-up of palpable and incidental thyroid nodules has been reviewed in detail. In general, evaluation includes thorough physical examination of the neck, US for confirmation and characterization, which may identify other thyroid nodules or cervical lymphadenopathy, and FNA for evaluation of suspicious nodules. Appropriate diagnostic evaluation and interpretation is crucial to ensure timely treatment with patients with false-negative FNA eventually found to have higher rates of vascular and capsular invasion, and with a near doubling of 30-year mortality rate when therapy was delayed by more than 1 year from diagnosis.
Thyroid embryology and anatomy
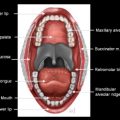
Embryologically, the thyroid gland develops as an epithelial proliferation from the floor of the pharynx in the dorsal tongue at the level of the foramen cecum. At approximately 5 weeks, fetal development the thyroid descends caudally around the hyoid bone, deep to the strap musculature, and to its expected location below the level of the laryngeal primordium, where it forms lateral lobes and isthmus. The embryologic pathway from the foramen cecum to the isthmus of the thyroid is the thyroglossal duct, which subsequently involutes. Arrest of migration of part or all of the thyroid gland can result in ectopic thyroid tissue or cysts anywhere along this thyroglossal duct.
The thyroid gland resides in the lower portion of the infrahyoid neck within the visceral space (level VI), which is bounded superiorly by the hyoid bone, laterally by the carotid arteries and inferiorly by the sternal notch ( Figs. 1 and 2 ). The visceral space is encompassed by the middle layer of deep cervical fascia and also envelops the thyroid strap musculature, the parathyroid glands, larynx, hypopharynx, trachea, and esophagus. The isthmus of the thyroid gland generally lies anterior to the second to fourth tracheal rings, with the lateral thyroid lobes anterolateral to the lower thyroid cartilage, cricoid cartilage, and upper trachea. A small pyramidal lobe may be present, extending superiorly from the isthmus anterior to the thyroid cartilage, where it may connect with a thyroglossal duct remnant.
The outer surface of the thyroid gland is incompletely covered by a thin connective tissue layer in direct continuity with the stroma that defines lobules of thyroid parenchyma. This discontinuous fibroadipose connective tissue layer has been described as the internal thyroid capsule. The external thyroid capsule or surgical capsule is mainly derived from the pretracheal deep cervical fascia, is adherent to the deep surface of the strap muscles, and posterolaterally continuous with the carotid sheath. This external thyroid capsule is deficient in the anterior midline, so the thyroid isthmus is connected directly to the subcutaneous fat and superficial cervical fascia.
The arterial supply to the thyroid gland is from the paired superior thyroidal arteries arising from the external carotid arteries and from the paired inferior thyroidal arteries arising from the thyrocervical trunks of the subclavian arteries. A rare persistent embryonic vessel called the thyroidea ima artery may arise directly from the aortic arch to supply the lower thyroid gland. Both superior and middle thyroidal veins drain the very vascular thyroid tissues via the internal jugular veins, whereas the inferior thyroidal veins drain into the brachiocephalic veins.
The lymphatic pathways in the thyroid gland are intricate and interconnected with those of the larynx, trachea, recurrent laryngeal nerve (RLN), and cervical great vessels (see Fig. 2 ). There is an extensive intrathyroidal lymphatic network that joins subcapsular lymphatic trunks, which generally drain the thyroid along the course of thyroidal veins. The lymph nodes in the visceral space can be subdivided into the pretracheal, prelaryngeal (delphian), and paratracheal nodes. The upper poles, isthmus, and the pyramidal lobe drain into level II and III nodal zones. The lateral aspects of the thyroid lobes drain along the middle thyroid veins into level III and IV nodal zones. The lower poles drain into the pretracheal and paratracheal lymph nodes within the level VI nodal zone, which then drain into levels IV and VII. There are also direct lymphatic communications in levels II, III, and IV, which then drain into level VII via level VI. These lymphatic pathways are variable and lymphatics draining into the capsule may cross-communicate with the isthmus and the contralateral lobe.
Imaging techniques in thyroid cancer
US
US has demonstrated its utility in characterizing palpable or incidentally found thyroid nodules preoperatively into groups based on benign or malignant features. Based on such determination of relative risk for thyroid malignancy, US also facilitates detection of additional nonpalpable nodules, evaluation of lymph nodes in the central and lateral neck, and performance of US-guided (UG-FNA).
A variety of US characteristics are thought to differentiate benign from malignant thyroid lesions. Whereas smooth margins of a thyroid nodule may indicate benignity, irregular or ill-defined lesions suggest a malignant lesion. Some malignant nodules may have a cystic component, but many are solid and appear hypoechoic relative to adjacent thyroid tissue. Most benign lesions result in acoustic shadowing or enhancement. A thyroid nodule that is greater in its anteroposterior than in its transverse dimension has also been described more likely to represent a malignant instead of a benign lesion. Microcalcifications are more strongly associated with malignancy compared with coarse or no calcifications. Central vascularity is more likely to be present in malignant thyroid nodules, whereas peripheral vascularity is associated with benign lesions.
The typical US findings of metastatic lymph nodes in thyroid cancer include a homogenous hypoechoic or heterogeneous pattern, an irregular cystic appearance, the presence of internal calcification, loss of reniform shape, and increased anteroposterior diameter. Cystic change is said to be highly suggestive of PTC and is well-demonstrated by US. Occasionally this can appear as a cyst and thus mimic a branchial cleft cyst in younger patients ( Fig. 3 ). US demonstrates a high positive predictive value for lateral node metastasis, which can be increased further by UG-FNA of suspected metastasis ; however, there are many false negatives with US for both central compartment and lateral lymph nodes. US has additional value in the postoperative surveillance of patients treated for thyroid cancer. Routinely, patients undergo an initial cervical US in the first year following resection of their thyroid cancer with subsequent US performed according to patient’s risk of locoregional recurrence.
CT
CT optimally requires the use of intravenous iodinated contrast agents to opacify normal vascular structures and to delineate abnormal enhancement. The iodine load may alter radioactive iodine uptake for 6 weeks after its administration and is, therefore, generally not ideal in initial presurgical evaluation of thyroid cancer. Characterization of thyroid nodules as benign or malignant is highly problematic on CT unless features of gross extrathyroidal extension (ETE) are present ( Fig. 4 ). Both CT and MR imaging are useful tools for the evaluation of ETE into the surrounding organs such as larynx and trachea, and CT may be particularly useful in defining invasion of the cartilaginous framework of the laryngotracheal complex. Complete evaluation of cervical lymph nodes is offered by both CT and MR imaging, including retropharyngeal, deep cervical, and substernal regions. Metastatic nodes can appear as cystic masses, have multiple punctate calcifications, or enhance avidly. Metastatic lymph nodes may be of high attenuation even before intravenous contrast administration because of the presence of intranodal hemorrhage or thyroglobulin.
MR Imaging
Unlike iodinated contrast for CT, gadolinium-based contrast agents for MR imaging do not affect thyroid iodine uptake. On MR imaging, both benign thyroid nodules and malignant tumors are generally well-defined and often indistinguishable, or may be occult. Most malignant thyroid tumors demonstrate isointense signal to normal thyroid tissue on T1-weighted images and hyperintense signal on T2-weighted images, with avid enhancement making the signal characteristics nonspecific ( Fig. 5 ). Microcalcifications representing psammoma bodies are readily detected on US and sometimes on CT, but are poorly seen on MR imaging. Tumor invasion into the posterior paratracheal tissues and substernal area is better visualized on MR imaging than US because of obscuration due to the bone and lung. MR imaging offers the best option for assessing soft tissue invasion, in particular when pharyngoesophageal invasion is suspected.
On MR imaging, metastatic lymph nodes can have low to intermediate signal intensity on T1-weighted and hyperintensity on T2-weighted images, or hyperintensity on both T1-weighted and T2-weighted images, reflecting a high thyroglobulin content or hemorrhage ( Fig. 6 ). Metastatic nodes may enhance markedly. A cystic or necrotic appearance is helpful to raise suspicion for metastasis but may simulate a second branchial cleft cyst or metastasis from an oropharyngeal primary. MR imaging has been shown to be highly specific for nodal metastasis but with low sensitivity. The retropharyngeal and mediastinal regions are not amenable to imaging on US, but are well-evaluated on MR imaging.
Nuclear Scintigraphy and Positron Emission Tomography
Radioiodine scintigraphy provides functional information about the thyroid gland and is useful for patients with abnormal thyroid function. For focal thyroid masses, however, most nodules are hypofunctioning (cold) and the risk of malignancy in such a nodule is between 8% to 25%, so radioiodine scintigraphy does not play a major role in the diagnostic workup. It is generally performed as part of postoperative radioactive iodine ablation (RAI) and may detect occult metastasis or residual disease postoperatively. In patients who have intermediate or high risk for disease recurrence, or who have elevated thyroglobulin levels, radioactive iodine scanning may be helpful in identifying foci of thyroid cancer. This modality has low sensitivity in low-risk patients who have undergone complete resection and adjuvant radioactive iodine. In patients with MTC, imaging with octreotide or m-iodobenzylguanidine (MIBG) may be useful.
Fluorodeoxyglucose F 18 positron-emission tomography (FDG-PET) is of limited utility for characterization of primary thyroid nodules because they may or may not be FDG-avid, ( Fig. 7 ). In the thyroglobulin-positive but radioactive iodine scan–negative patient, FDG-PET has a role in defining the location of persistent or recurrent disease but, despite a reproducible ability to detect recurrent thyroid cancer, use of FDG-PET rarely alters treatment. However, it has prognostic value because the number of FDG-avid lesions and their intensity helps identify patients at highest risk for rapid disease progression and disease specific mortality.
Staging of DTC and pitfalls
The clinical and pathologic factors associated with disease recurrence and/or disease-free survival have been described. The main clinical factors are increased age and male gender. Among the postoperative pathologic factors, tumor size, ETE, tumor histology, and presence of metastatic disease all have prognostic value. Various staging systems have been proposed to stage DTC. The American Joint Commission on Cancer (AJCC) scheme depends on age and a standardized TNM (tumor, node, metastasis) classification described in Table 1 . The pitfalls in staging of thyroid cancer are described in Table 2 ).
| Primary Tumor (T) | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| T1 | Tumor 2 cm or less in greatest dimension limited to the thyroid |
| T1a | Tumor 1 cm or less, limited to the thyroid |
| T1b | Tumor more than 1 cm but not more than 2 cm in greatest dimension, limited to the thyroid |
| T2 | Tumor more than 2 cm but not more than 4 cm in greatest dimension, limited to the thyroid |
| T3 | Tumor more than 4 cm in greatest dimension limited to the thyroid, or any tumor with minimal extrathyroid extension (eg, extension to sternothyroid muscle or perithyroid soft tissues) |
| T4a | Moderately advanced disease Tumor of any size extending beyond the thyroid capsule to invade subcutaneous soft tissues, larynx, trachea, esophagus, or RLN |
| T4b | Very advanced disease Tumor invades prevertebral fascia or encases carotid artery or mediastinal vessels |
| All anaplastic carcinomas are considered T4 tumors | |
| T4a | Intrathyroidal anaplastic carcinoma |
| T4b | Anaplastic carcinoma with gross extrathyroid extension |
| Regional Lymph Nodes (N) | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Regional lymph node metastasis |
| N1a | Metastasis to level VI (pretracheal, paratracheal, and prelaryngeal/Delphian lymph nodes) |
| N1b | Metastasis to unilateral, bilateral, or contralateral cervical (levels I, II, III, IVor V) or retropharyngeal or superior mediastinal lymph nodes (level VII) |
| Distant Metastasis (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| Pitfall | Advice |
|---|---|
| Misdiagnosis of cystic neck mass as second branchial cleft cyst | Consider metastatic PTC (as well as oropharyngeal squamous cell carcinoma ) and carefully evaluate the thyroid gland. |
| Misdiagnosis of thyroid nodule on PET as benign due to low FDG uptake | Evaluate incidental nodules on PET with US and UG-FNA |
| Misdiagnosis of thyroid nodule on CT or MR imaging as benign due to presence of multiple nodules suggestive of goiter | Evaluate any dominant nodule on CT or MRimaging with US and carefully assess for any features of ETE |
| Understaging due to failure to recognize ETE to the RLN | Recognize the CT/MR imaging signs of VCP and scrutinize the tracheoesophageal groove region |
| Upstaging to T4a: overcalling tracheal wall involvement on CT | Consider MR imaging in absence of gross intraluminal tumor to better evaluate the tracheal wall |
| Understaging of N stage from retropharyngeal lymph node metastasis clinically or with US | Carefully evaluate retropharyngeal lymph nodes on CT and MR imaging |
| Understaging of distant metastasis on neck MR imaging and CT | Evaluate the lung apices for nodules and osseous structures for lytic lesions |
The primary tumor (T) classification is based on tumor size and extracapsular extension. In some cases the primary tumor is not evident on any imaging modality or even on pathologic study, representing a T0 lesion ( Fig. 8 ). A T1 lesion is up to 2 cm in the largest dimension, a T2 primary tumor is more than 2 cm but less than 4 cm, and T3 includes an intrathyroidal lesion more than 4 cm. A T3 lesion also includes any tumor with minimal ETE, defined as extension to the sternothyroid muscle or perithyroid soft tissues. Tumors with further extension become T4, subdivided into T4a and T4b. T4a refers to tumors invading subcutaneous soft tissues, the larynx, trachea, esophagus, or RLN. T4b lesions are the lesions invading the prevertebral fascia or carotid artery or mediastinal vessels.
Regional lymph node spread from DTC is common. The central compartment (level VI) lymph nodes are the primary locations for thyroid node metastasis. The lateral cervical nodes include levels II to V, although levels II and V are less commonly involved than III and IV. Upper mediastinal (level VII) lymph node involvement is common. NX is designated when regional nodes cannot be assessed. N0 indicates no regional lymph node metastasis. N1 indicates regional lymph node metastasis, with N1a indicating metastasis to the central compartment and N1b indicating involvement of any lymph node in lateral compartment or superior mediastinum. There is no difference between ipsilateral and contralateral lymph node metastasis in staging for thyroid cancer nodal classification. M0 and M1 indicate the absence or presence of distal metastases, respectively.
Tumor Size
In DTC, primary tumor size correlates with outcome, with larger tumors more likely to present with locoregional and distant metastases. Tumors less than 1 cm are rarely associated with mortality ; however, the risk of recurrent local disease and mortality increases linearly with tumor size. In one study, primary tumors less than 1.5 cm had 30-year cancer-specific mortality rates of 0.4% compared with 22% in tumors measuring greater than 4.5 cm. The presence of underlying thyroiditis or multinodular goiter may cause difficulty in detection of small thyroid lesions ( Fig. 9 ) or the presence of coexistent benign and malignant lesions ( Fig. 10 ). Total thyroidectomy is the recommended surgical approach for nearly all patients with DTC. Furthermore, by surgically removing the entire gland, total thyroidectomy facilitates the use of radioactive iodine for adjuvant therapy, serial measurement of serum thyroglobulin for surveillance, and neck US identify residual or recurrent disease. Thyroid lobectomy is an acceptable alternative for those patients with tumors less than 1 cm confined to one thyroid lobe without nodules within the contralateral lobe. This more limited procedure avoids injury to structures in the contralateral neck without effect on long-term survival. PTC is multifocal in 18% to 46% of cases, and can arise as independent tumors or because of intrathyroidal metastasis via the rich lymphatic network within the thyroid.