Lymph nodes status is an important predictor of prognosis in head and neck squamous cell carcinoma, making accurate staging critical. The physical examination of the neck is highly inaccurate. CT, MR imaging, ultrasound (US), and positron emission tomography-CT (PET-CT) improve accuracy but have limitations. Size criteria, nodal shape and clustering, central necrosis, and findings of extracapsular spread and vascular encasement suggest metastatic involvement on CT and MR imaging. US features help differentiate benign from malignant nodes, aided by US-guided fine-needle aspiration for indeterminate cases. PET-CT is useful for staging the lymph nodes and detection of distant metastasis.
Key points
- •
Lymph nodes status is one or the most important predictors of prognosis in head and neck squamous cell carcinoma, making accurate staging critical.
- •
The physical examination of the neck is highly inaccurate.
- •
Imaging by CT, MR imaging, ultrasound (US), and positron emission tomography-CT (PET-CT) improve accuracy of staging, but all have limitations, particularly detection of small metastatic lymph nodes harboring microscopic metastatic disease.
- •
This article reviews the classification of cervical lymph nodes, findings that suggest metastatic involvement of lymph nodes, and the evidence for staging using CT, MR imaging, US, and PET-CT.
Introduction
Head and neck squamous cell carcinoma (HNSCC) comprises most head and neck malignancies. Regardless of the primary tumor site, the presence of a single metastatic lymph node in HNSCC reduces the 5-year survival rate by approximately 50%. The presence of bilateral metastatic lymph nodes in the neck reduces the survival rate to about 25% of that of patients without nodal metastasis. Cervical lymph node metastases influence not only the risk of local recurrence but also the risk of distant metastases, making lymph node status one of the most important predictors of prognosis in HNSCC.
It takes an estimated one billion malignant cells to create a 1 mm 3 mass. Although such tumors can be readily identified under microscopy, such minute foci of metastatic disease are not visible on gross inspection and cannot be reliably detected by any current imaging technique. Depending on the primary tumor site, lymph node metastasis will be histopathologically present in as high as 32% of patients with HNSCC. The inaccuracy of the physical examination for detection of metastatic cervical lymph nodes has been documented in several studies. The false-negative and false-positive rates of the physical examination are 15% to 20% and 30% to 50%, respectively, so the treatment of patients with a clinically negative neck stage of N0 remains controversial ( Fig. 1 ).
Up to 32% of patients with clinically negative lymph nodes who are not treated will develop lymph node metastasis in the neck, leading to a poorer outcome, making undertreatment of the N0 neck undesirable. Given the relatively high risk of clinically occult cervical lymph node metastasis, most head and neck surgeons promote elective treatment of the neck. About 75% of elective neck dissections, however, prove to be free of tumor at histopathologic examination. Although neck dissections have low complication rates in experienced hands, there is still considerable morbidity and mortality to both neck dissection and radiation therapy to the neck. Radiation therapy and chemotherapy are frequently used concurrently in the treatment of primaries such as oropharyngeal HNSCC to avoid the morbidity of surgical resection, but both of these treatments can also have severe local adverse effects and systemic toxicities. Furthermore, the use of radiation therapy precludes its future use for management of second head and neck primary cancers that occur in up to 25% of these patients. For these reasons, overtreatment of a high percentage of necks that are ultimately negative for metastatic lymph nodes is also not optimal.
So, what is the role of imaging in the staging of lymph nodes if we cannot identify and categorically exclude micrometastases, and the treatment of the neck by surgical dissection or radiation therapy may already be decided based on standard management of the primary tumor and the head and neck surgeon’s practice preferences? A major role of imaging lymph nodes in the staging of HNSCC is to guide decisions for unexpected lymph node metastasis present in the contralateral neck and detection of ipsilateral metastatic lymph nodes where they may not be suspected and may not otherwise be treated. In a patient with a left-sided primary tumor site who will be undergoing surgical resection of the primary and left-sided neck dissection, the detection of even a single metastatic contralateral neck lymph node on imaging alters the management substantially. Most standard neck dissections for HNSCC do not address lymph nodes in level V, some do not include level I, IIB, or IV, and retropharyngeal lymph nodes are not routinely addressed surgically. Therefore, the detection of metastatic lymph nodes in these locations also affects the extent of surgical management. Even when treatment is nonsurgical, the planning of radiation therapy is influenced by presence and location of metastatic lymph nodes on imaging. The preoperative detection of extracapsular spread (ECS) from lymph nodes and any resultant carotid arterial encasement affects whether or not surgery is performed at all, planning of the type of neck dissection performed (radical vs selective), and whether or not preoperative chemotherapy is used. Therefore, accurate assessment of lymph node status by imaging is critical for the management of HNSCC.
Introduction
Head and neck squamous cell carcinoma (HNSCC) comprises most head and neck malignancies. Regardless of the primary tumor site, the presence of a single metastatic lymph node in HNSCC reduces the 5-year survival rate by approximately 50%. The presence of bilateral metastatic lymph nodes in the neck reduces the survival rate to about 25% of that of patients without nodal metastasis. Cervical lymph node metastases influence not only the risk of local recurrence but also the risk of distant metastases, making lymph node status one of the most important predictors of prognosis in HNSCC.
It takes an estimated one billion malignant cells to create a 1 mm 3 mass. Although such tumors can be readily identified under microscopy, such minute foci of metastatic disease are not visible on gross inspection and cannot be reliably detected by any current imaging technique. Depending on the primary tumor site, lymph node metastasis will be histopathologically present in as high as 32% of patients with HNSCC. The inaccuracy of the physical examination for detection of metastatic cervical lymph nodes has been documented in several studies. The false-negative and false-positive rates of the physical examination are 15% to 20% and 30% to 50%, respectively, so the treatment of patients with a clinically negative neck stage of N0 remains controversial ( Fig. 1 ).
Up to 32% of patients with clinically negative lymph nodes who are not treated will develop lymph node metastasis in the neck, leading to a poorer outcome, making undertreatment of the N0 neck undesirable. Given the relatively high risk of clinically occult cervical lymph node metastasis, most head and neck surgeons promote elective treatment of the neck. About 75% of elective neck dissections, however, prove to be free of tumor at histopathologic examination. Although neck dissections have low complication rates in experienced hands, there is still considerable morbidity and mortality to both neck dissection and radiation therapy to the neck. Radiation therapy and chemotherapy are frequently used concurrently in the treatment of primaries such as oropharyngeal HNSCC to avoid the morbidity of surgical resection, but both of these treatments can also have severe local adverse effects and systemic toxicities. Furthermore, the use of radiation therapy precludes its future use for management of second head and neck primary cancers that occur in up to 25% of these patients. For these reasons, overtreatment of a high percentage of necks that are ultimately negative for metastatic lymph nodes is also not optimal.
So, what is the role of imaging in the staging of lymph nodes if we cannot identify and categorically exclude micrometastases, and the treatment of the neck by surgical dissection or radiation therapy may already be decided based on standard management of the primary tumor and the head and neck surgeon’s practice preferences? A major role of imaging lymph nodes in the staging of HNSCC is to guide decisions for unexpected lymph node metastasis present in the contralateral neck and detection of ipsilateral metastatic lymph nodes where they may not be suspected and may not otherwise be treated. In a patient with a left-sided primary tumor site who will be undergoing surgical resection of the primary and left-sided neck dissection, the detection of even a single metastatic contralateral neck lymph node on imaging alters the management substantially. Most standard neck dissections for HNSCC do not address lymph nodes in level V, some do not include level I, IIB, or IV, and retropharyngeal lymph nodes are not routinely addressed surgically. Therefore, the detection of metastatic lymph nodes in these locations also affects the extent of surgical management. Even when treatment is nonsurgical, the planning of radiation therapy is influenced by presence and location of metastatic lymph nodes on imaging. The preoperative detection of extracapsular spread (ECS) from lymph nodes and any resultant carotid arterial encasement affects whether or not surgery is performed at all, planning of the type of neck dissection performed (radical vs selective), and whether or not preoperative chemotherapy is used. Therefore, accurate assessment of lymph node status by imaging is critical for the management of HNSCC.
Cervical lymph node classification
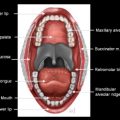
The imaging-based classification of lymph nodes in the neck has been described in detail previously by Som and colleagues The anatomic boundaries and locations of the lymph nodes in the neck are listed in Table 1 and depicted in Fig. 2 . This nodal scheme is universally accepted and used, and should be incorporated into cross-sectional neck imaging interpretations by the radiologist.
| Level | Description |
|---|---|
| I | The submental and submandibular nodes, located above the hyoid bone, below the mylohyoid muscle, and anterior to the back of the submandibular gland (SMGs) |
| IA | The submental nodes. These lie between the medial margins of the anterior bellies of the digastric muscles. |
| IB | The submandibular nodes. These lie lateral to the IA nodes and anterior to the back of the SMGs |
| II | The upper internal jugular nodes, lying from the skull base to the bottom of the body of the hyoid bone, posterior to the back of the SMG, and anterior to the back of the sternocleidomastiod muscle (SCM) |
| IIA | The level II nodes anterior, medial, lateral, and immediately posterior to the internal jugular vein (IJV) |
| IIB | The level II nodes posterior to the IJV separated by a fat plane |
| III | The midjugular nodes, located from the bottom of the body of the hyoid bone to the level of the bottom of the cricoid arch. These lie anterior to the back of the SCM. |
| IV | The low jugular nodes, located from the bottom of the cricoid arch to the level of the clavicle. These lie anterior to the back of the SCM and the posterolateral margin of the anterior scalene muscle. |
| V | The posterior triangle nodes, located posterior to the back of the SCM from the skull base to the level of the clavicles. |
| VA | Upper level V nodes from skull base to the bottom of the cricoid arch posterior to the SCM. |
| VB | Lower level V nodes from the bottom of the cricoid arch to the level of the clavicles as seen on axial images. These are posterior to a line connecting the back of the SCM and the posterolateral margin of the anterior scalene muscle. |
| VI | The visceral nodes, located between the carotid arteries from the level of the bottom of the body of the hyoid bone to the top of the manubrium. |
| VII | The superior mediastinal nodes, located between the carotid arteries below the level of the manubrium and above the level of the innominate vein. |
| Supraclavicular | These are located caudal to the level of the clavicle on axial images and lateral to the carotid arteries on each side of the neck. |
| Retropharyngeal | These are located within 2 cm of the skull base and medial to the internal carotid arteries. |
CT staging of cervical lymph node metastases and pitfalls
CT is commonly the imaging modality used for staging the primary site of HNSCC and is, therefore, used to stage the lymph nodes in the neck. CT has improved the accuracy of nodal staging over physical examination, allowing for evaluation of retropharyngeal, tracheoesophageal, and lymph nodes deep to the sternocleidomastoid muscle, decreasing the error rate of palpation by 7.5% to 19%. CT criteria for assessing nodal metastases are nodal size, shape, presence of central necrosis, and grouping of nodes in an expected draining nodal station for a specific primary tumor ( Table 2 ).
| Pitfall | Advice |
|---|---|
| Understaging of HNSCC due to reliance on clinical palpation | CT, MR imaging, US, and PET-CT all can detect nonpalpable deep and small lymph nodes |
| Understaging of clustered small lymph nodes | Clustered nonnecrotic lymph nodes not meeting size-criteria are still suspicious for nodal metastasis when in the primary drainage pathway for the primary site |
| Misdiagnosis of necrotic infectious lymphadenitis as metastatic disease | Always consider the clinical context and use UG-FNA to troubleshoot, when needed |
| Overdiagnosis of a hilar fat as necrosis on thick-section CT images | For small lymph nodes review the thinnest image dataset obtained and use pixel analysis to identify fat density |
| Misdiagnosis of the thoracic duct as a cystic level IV lymph node | Consider a prominent thoracic duct when dealing with a left level IV lymph node and use coronal reformatted images to identify the characteristic location at the junction of the IJV and subclavian vein |
| Overdiagnosis of ECS | Review the medical record for any recent biopsy or local infection that may falsely result in the appearance of ECS |
| Understaging of small necrotic lymph nodes on PET | Use CE-CT for attenuation correction for PET to identify small necrotic or cystic hypometabolic metastatic lymph nodes |
Lymph Node Size
A multicenter study of nodal size in 100 neck dissections for HNSCC showed that 46% of metastatic nodes were less than 10 mm and 22% of metastatic nodes were between 10 and 15 mm in diameter. Another pathologic analysis of 750 lymph nodes in subjects with HNSCC demonstrated that most normal nodes are less than 5 mm in diameter but that metastatic nodes vary in size without having any peak in size distribution. Many different size criteria for metastatic nodes have been proposed for CT and MR imaging. Some investigators consider any node greater than 10 mm as abnormal, whereas other investigators have used varying size criteria according to the location of lymph nodes. Frequently used criteria for the greatest transaxial nodal diameter (long axis) is 15 mm for level I and II lymph nodes and 10 mm for all other cervical nodes. Using these criteria, lymph nodes that exceed these dimensions are metastatic about 80% of the time. Other studies have found slightly different size criteria, with different balances of sensitivity and specificity. Regardless of the size criteria used, there will always be borderline sized nodes without evidence of necrosis that remain indeterminate ( Fig. 3 ).
Nodal Shape and Grouping
The addition of nodal shape as a criterion to nodal size only minimally improves the sensitivity of CT diagnosis. This criterion is based on the pathologic observation that reactive lymph nodes are generally kidney-bean shaped, whereas most metastatic nodes are spherical. If a lymph node is borderline pathologic by size criteria but is spherical, it is slightly more likely to truly contain metastatic tumor. Nodal grouping refers to three or more contiguous and confluent lymph nodes, each of which has a maximal diameter of 8 to 15 mm. Such a grouping in the lymphatic drainage chain of the tumor is highly suggestive of metastatic lymph node involvement ( Fig. 4 ). Close and colleagues evaluated 61 subjects with HNSCC by CT and reported that the presence of multiple otherwise benign looking nodes in a high risk lymphatic station correctly predicted metastases in 61%.
Central Necrosis
The most accurate CT finding for the presence of metastatic lymphadenopathy from HNSCC is central necrosis. Tumor cells initially replace the medulla of the node, which later undergoes necrosis, so the medullary region of lymph nodes contain tumor cells as well as necrotic tissue, both of which result in central low attention on CT in contrast to the cortical portions of the node that enhance with iodinated contrast material. In a large clinical series, however, 74% of metastatic nodes contained central necrosis on pathologic study, whereas central necrosis was seen in only 32% of metastatic lymph nodes on imaging. Therefore, a homogeneous appearance of lymph nodes on CT or MR imaging does not exclude the presence of nodal metastasis. Particularly, the percentage of central nodal necrosis is greatly reduced in smaller nodes. Contrast-enhanced CT (CE-CT) is considered to be the best imaging modality for identification of necrosis, with a sensitivity of 74% and a specificity of 94% reported for areas of necrosis larger than 3 mm.
Both lipid metaplasia and infection resulting in nodal abscess formation can simulate necrosis due to metastasis on CT ( Fig. 5 ). Lipid metaplasia or fatty degeneration can rarely occur in lymph nodes after severe inflammatory disease or after radiation therapy. In most cases, such fat is peripheral, corresponding to the hilum instead of central, but this may be difficult to determine on CT. The lower attenuation of fat compared with necrosis may also be difficult to differentiate for small nodes due to partial volume effects ( Fig. 6 ). A node with abscess formation is almost always accompanied by corresponding signs and symptoms of infection. Such a lymph node can have central low attenuation and irregular enhancing margins, all of which simulate a metastatic node. Evaluation for associated adjacent cellulitis to assist in diagnosis may be problematic in a patient who has been incompletely treated with antibiotics, or recently postsurgical or postradiation therapy.
Cystic lymph nodes are frequently seen in the setting of human papilloma virus–positive oropharyngeal carcinoma. When located in level II, these may be mistaken for second branchial cleft cyst ( Fig. 7 ) or a cystic nerve sheath tumor ( Fig. 8 ) leading to misdiagnosis. When located in left level IV, the thoracic duct as it enters the confluence of the left internal jugular vein and subclavian vein may simulate a cystic lymph node, potentially leading to a false positive for metastatic lymphadenopathy ( Fig. 9 ).
ECS
Extension of metastatic tumor beyond the lymph node capsule, or ECS is the best prognostic factor for local treatment failure in the neck and an indicator of reduction of survival rate by an additional 50%. Postoperative radiation therapy is usually indicated for treatment of the neck if ECS is demonstrated by histology. Studies have also established histologically-identified ECS as a major determinant of whether a patient would benefit from adjuvant chemotherapy because patients with distant metastasis have higher rates of ECS.
On CT, ECS is diagnosed when there is enhancement of the nodal periphery with poorly defined margins, infiltration of adjacent fat or muscle planes, and capsular contour irregularity. These criteria are accurate only if the patient has not recently had surgery, irradiation, or an active infection in the area. ( Fig. 10 ). Although it was initially believed that ECS occurred only in lymph nodes larger than 3 cm in greatest diameter, studies correlating CT and histologic findings have shown that such extension actually occurs in 23% of nodes less than 1 cm in greatest diameter, in 53% of nodes 2 to 3 cm in greatest diameter, and in 74% of nodes greater than 3 cm in greatest diameter. Woolgar and colleagues reported histologic evidence of ECS in 16% of HNSCC subjects staged as N0 by CT.