The major salivary glands consist of the parotid, submandibular, and sublingual glands. Most neoplasms in other subsites in the head and neck are squamous cell carcinoma, but tumors of the salivary glands may be benign or malignant. Surgical treatment differs if the lesion is benign, and therefore preoperative fine needle aspiration is important in salivary neoplasms. The role of imaging is to attempt to determine histology, predict likelihood of a lesion being malignant, and report an imaging stage. This article reviews the various histologies, imaging features, and staging of major salivary gland neoplasms.
Key points
- •
The major salivary glands consist of the parotid, submandibular, and sublingual glands.
- •
Most neoplasms in other subsites in the head and neck are squamous cell carcinoma, but tumors of the salivary glands may be benign or malignant.
- •
Surgical treatment differs if the lesion is benign, and therefore preoperative fine-needle aspiration is important in salivary neoplasms.
- •
The role of imaging is to attempt to determine histology, predict likelihood of a lesion being malignant, and report an imaging stage.
- •
This article reviews the various histologies, imaging features, and staging of major salivary gland neoplasms.
Anatomy and boundaries
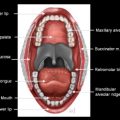
The major salivary glands consist of the parotid, submandibular, and sublingual glands. Submucosal clusters of salivary tissue located in the palate, oral cavity, paranasal sinuses, and upper aerodigestive tract are minor salivary glands, and are variable in distribution. Primary neoplasms arising in the minor salivary glands are staged according to the anatomic site of origin.
The parotid gland is the largest of the salivary glands, the bulk of which lies superficial to the masseter muscle and mandibular ramus and angle ( Fig. 1 ). The investing fascia arises from the superficial layer of the deep cervical fascia. The deep portion of the gland extends through the stylomandibular tunnel into the prestyloid compartment of the parapharyngeal space. The stylomandibular tunnel is formed by the skull base, posterior margin of the mandibular ramus, and styloid process and stylomandibular ligament. Although the parotid gland is a single contiguous structure, for surgical convenience it has been divided into superficial and deep lobes by the course of the facial nerve, which courses lateral to the retromandibular vein. Most neoplasms arise in the superficial portion of the gland. Considerable variation in intraparotid facial nerve anatomy exists, but most commonly the nerve enters the posteromedial aspect of the gland and divides into 2 main trunks before dividing into 5 main branches: temporal, zygomatic, buccal, mandibular, and cervical. The auriculotemporal nerve, which curves around the mandibular neck, embedded in the gland capsule, connects the mandibular branch of the trigeminal nerve with the facial nerve and serves as a potential route of perineural tumor spread.
Accessory parotid tissue is found in approximately 20% of the population, anterior to the parotid gland, typically overlying the masseter muscle between the zygomatic arch and parotid duct. In distinction to other salivary glands, between 3 and 24 lymph nodes are found within the parotid gland, almost all within the superficial portion of the gland. Parotid lymph nodes drain into the level IIA and IIB upper cervical chains. The main parotid duct, Stensen’s duct, is approximately 7 cm in length, exiting the anterior aspect of the gland, passing horizontally lateral to the masseter muscle and medial to the zygomaticus major muscle, pierces the buccinator muscle, and opens on a papilla in the buccal mucosa opposite the second maxillary molar tooth.
The submandibular gland occupies most of the submandibular triangle, which is formed by the inferior border of the mandibular body and anterior and posterior bellies of the digastric muscle ( Fig. 2 ). The stylohyoid muscle also forms part of the posterior boundary. The submandibular gland is enveloped by a thin fibrous capsule. The stylomandibular ligament, a reflection of the deep cervical fascia, separates the parotid and submandibular glands. The submandibular gland is arbitrarily divided into superficial and deep lobes based on its extension around the posterior margin of the mylohyoid muscle, which divides the submandibular space from the floor of the mouth. No lymph nodes or large nerves are present within the submandibular gland. Lymphatic drainage is into IB or submandibular nodes and deep cervical lymph nodes, particularly IIA nodes. Wharton’s duct, the primary excretory duct, courses anteriorly and superiorly between the genioglossus muscle and sublingual gland to open in the floor of mouth on the sublingual papilla on the side of the tongue.
The anterior facial vein, which runs along the lateral margin of the submandibular gland, can be used to distinguish exophytic submandibular masses from extrinsic lesions, such as lymphadenopathy or soft tissue tumors, that arise adjacent to the gland. A mass separated by the facial vein from the gland must be an extrinsic lesion.
The sublingual gland is the smallest of the major salivary glands and is situated above the mylohyoid muscle, covered by mucosa of the floor of the mouth. No well-defined capsule exists. Numerous small excretory ducts, the Rivinus ducts, open directly into the floor of the mouth. A large duct, Bartholin duct, may empty into the submandibular duct near its orifice. Primary lymphatic drainage is into level I lymph nodes.
Anatomy and boundaries
The major salivary glands consist of the parotid, submandibular, and sublingual glands. Submucosal clusters of salivary tissue located in the palate, oral cavity, paranasal sinuses, and upper aerodigestive tract are minor salivary glands, and are variable in distribution. Primary neoplasms arising in the minor salivary glands are staged according to the anatomic site of origin.
The parotid gland is the largest of the salivary glands, the bulk of which lies superficial to the masseter muscle and mandibular ramus and angle ( Fig. 1 ). The investing fascia arises from the superficial layer of the deep cervical fascia. The deep portion of the gland extends through the stylomandibular tunnel into the prestyloid compartment of the parapharyngeal space. The stylomandibular tunnel is formed by the skull base, posterior margin of the mandibular ramus, and styloid process and stylomandibular ligament. Although the parotid gland is a single contiguous structure, for surgical convenience it has been divided into superficial and deep lobes by the course of the facial nerve, which courses lateral to the retromandibular vein. Most neoplasms arise in the superficial portion of the gland. Considerable variation in intraparotid facial nerve anatomy exists, but most commonly the nerve enters the posteromedial aspect of the gland and divides into 2 main trunks before dividing into 5 main branches: temporal, zygomatic, buccal, mandibular, and cervical. The auriculotemporal nerve, which curves around the mandibular neck, embedded in the gland capsule, connects the mandibular branch of the trigeminal nerve with the facial nerve and serves as a potential route of perineural tumor spread.
Accessory parotid tissue is found in approximately 20% of the population, anterior to the parotid gland, typically overlying the masseter muscle between the zygomatic arch and parotid duct. In distinction to other salivary glands, between 3 and 24 lymph nodes are found within the parotid gland, almost all within the superficial portion of the gland. Parotid lymph nodes drain into the level IIA and IIB upper cervical chains. The main parotid duct, Stensen’s duct, is approximately 7 cm in length, exiting the anterior aspect of the gland, passing horizontally lateral to the masseter muscle and medial to the zygomaticus major muscle, pierces the buccinator muscle, and opens on a papilla in the buccal mucosa opposite the second maxillary molar tooth.
The submandibular gland occupies most of the submandibular triangle, which is formed by the inferior border of the mandibular body and anterior and posterior bellies of the digastric muscle ( Fig. 2 ). The stylohyoid muscle also forms part of the posterior boundary. The submandibular gland is enveloped by a thin fibrous capsule. The stylomandibular ligament, a reflection of the deep cervical fascia, separates the parotid and submandibular glands. The submandibular gland is arbitrarily divided into superficial and deep lobes based on its extension around the posterior margin of the mylohyoid muscle, which divides the submandibular space from the floor of the mouth. No lymph nodes or large nerves are present within the submandibular gland. Lymphatic drainage is into IB or submandibular nodes and deep cervical lymph nodes, particularly IIA nodes. Wharton’s duct, the primary excretory duct, courses anteriorly and superiorly between the genioglossus muscle and sublingual gland to open in the floor of mouth on the sublingual papilla on the side of the tongue.
The anterior facial vein, which runs along the lateral margin of the submandibular gland, can be used to distinguish exophytic submandibular masses from extrinsic lesions, such as lymphadenopathy or soft tissue tumors, that arise adjacent to the gland. A mass separated by the facial vein from the gland must be an extrinsic lesion.
The sublingual gland is the smallest of the major salivary glands and is situated above the mylohyoid muscle, covered by mucosa of the floor of the mouth. No well-defined capsule exists. Numerous small excretory ducts, the Rivinus ducts, open directly into the floor of the mouth. A large duct, Bartholin duct, may empty into the submandibular duct near its orifice. Primary lymphatic drainage is into level I lymph nodes.
Imaging workup
MR imaging is the preferred cross-sectional imaging modality to assess a noninflammatory salivary gland mass. Rarely, imaging will be definitive of a diagnosis ( Fig. 3 ); however, histologic differentiation of neoplasm is generally not possible on CT or T1-weighted images with or without contrast, although noncontrast T1-weighted images are helpful to assess tumor size, margins, depth, and extent. Certain imaging features may suggest malignancy. Bone invasion, perineural spread, and deep extension into the parapharyngeal space or muscles are highly indicative of malignancy. Although infiltrative margins suggest malignancy, hemorrhage or inflammatory changes on CT can create false-positive results for malignancy ( Fig. 4 ).
Benign and low-grade malignant lesions are likely to exhibit more hyperintense T2 signal, whereas high-grade malignancies tend to have intermediate or lower T2 signal. T2 signal is influenced by intracellular water content and cellularity. Differentiated benign or low-grade malignant lesions are more likely to produce serous or mucous secretions, which have a high water content. Unfortunately, although elevated T2 signal suggests that a lesion is not high-grade, it does not reliably distinguish between benign and low-grade malignant lesions ( Fig. 5 ). Low-grade malignancies, particularly mucoepidermoid and adenoid cystic carcinomas, may exhibit high T2 signal. Some benign lesions can have low T2 signal, including Warthin tumor, which is the second most common benign tumor of the parotid gland, granulomas, and fibrosis. However, for practical purposes, low T2 signal should serve as a warning that a high-grade lesion may be present. T1-weighted gadolinium-enhanced fat-saturated sequences should be included to assess for perineural spread, bone invasion, or meningeal involvement if intracranial extension is present. Effacement of fat in the neural foramen on noncontrast T1-weighted images allows for assessment of perineural spread while avoiding artifactual degradation that can be present at the skull base on fat-saturated sequences ( Fig. 6 ). Because almost all salivary gland neoplasms enhance, an important role of contrast in assessing the tumor is distinguishing a T2 hyperintense mass from a cyst.
MR imaging can delineate the intraparotid course of the facial nerve and parotid ducts. One technique acquires T1-weighted images through a 3-dimensional (3D) Fourier transform gradient-echo sequence (3D GRASS) using a head and neck coil at 1.5 T. Optimal results were obtained with a 20-cm field of view, 512 × 288 matrix, flip angle of 30 ° , repetition time of 30 ms, and effective echo time of 4.2 ms, and acquiring 60 sections at 1.5-mm thickness without gaps. Facial nerve and intraparotid ducts have lower T1 signal intensity than glandular tissue. Signal intensity within vessels varies with saturation. Curved, orthogonal, and volumetric reconstructed images of the 3D data allow the facial nerve and its branches to be followed in most patients from the stylomastoid foramen through the posterior superior aspect of the gland to the level of the retromandibular vein, and assessment of the parotid ducts at the hilum and in the anteroinferior portion of the gland. This technique is not routine in the authors’ practice, because facial nerve branches are each isolated intraoperatively if a local resection is being performed. The course of the nerve is also not relevant if a total parotidectomy is necessary for treatment.
The primary role of fluorodeoxyglucose (FDG) positron emission tomography (PET) is to detect locoregional and distant metastatic disease. The standardized uptake value (SUV) on PET does not reliably distinguish between benign and malignant salivary tumors. Although high-grade tumors tend to have higher FDG uptake than low- or intermediate-grade salivary gland malignancies, benign mixed tumors and Warthin tumors may also have high FDG uptake, resulting in false-positive results ( Fig. 7 ). FDG uptake in salivary gland malignancies has also not been shown to be useful in predicting patient survival. Sensitivity of FDG-PET for detecting salivary gland primary malignant tumors has been reported to be between 75% and 100%. False-negative PET results do occur, most frequently in low-grade malignancies wherein lower SUVs may be masked by physiologic FDG uptake in the salivary glands. Studies have shown FDG-PET to be more accurate than conventional imaging modalities in detecting locoregional and distant metastatic disease. MR imaging is superior to PET in depicting perineural spread of tumor.
Epidemiology
A painless, enlarging mass in the major salivary glands is most likely caused by a neoplasm, a cyst, or an enlarged lymph node. In general, the rate of malignancy of salivary gland neoplasms is inversely proportional to the gland size. The rate of malignancy is approximately 15% to 32% in the parotid gland, 41% to 45% in the submandibular gland, and 70% to 90% in the sublingual and minor salivary glands.
Cross-sectional imaging of salivary gland neoplasms is typically nonspecific; however, imaging patterns may suggest that a mass is either benign or low-grade malignant, or a higher-grade malignancy. Patterns of disease may help establish a differential diagnosis. Multiple parotid masses may be from lymphadenopathy, Warthin tumors, Sjögren syndrome, benign lymphoepithelial lesions of HIV, lymphoma, sarcoidosis, or multiple pleomorphic adenomas (usually in the setting of prior surgery or biopsy) ( Fig. 8 ).
Benign mixed tumor (BMT), or pleomorphic adenoma, is the most common salivary gland neoplasm, accounting for 60% to 70% of parotid tumors, with approximately 90% arising in the superficial lobe. Pleomorphic adenomas are most commonly well-defined, encapsulated, solitary, T2 hyperintense, enhancing lesions. Larger lesions characteristically assume a lobular contour and are more likely to be heterogeneous in composition. Although no single imaging feature is pathognomonic for BMT, a T2 hyperintense parotid mass with a complete capsule and lobulated margins is most likely to be a BMT ( Fig. 9 ). Areas of internal hemorrhage, cystic change, or calcification may be present. Dystrophic calcifications, when present, are highly suggestive of BMT. Malignancy may arise in association with primary or recurrent BMT, a risk that increases with tumor duration. Carcinoma ex pleomorphic adenoma (CXPA) accounts for approximately 5% to 15% of all salivary gland malignancies. It has been estimated that malignant degeneration may eventually occur in as many as 25% of untreated BMTs. Imaging features that suggest the possibility of CXPA include areas of low T2 signal and ill-defined infiltrative margins arising within a BMT or in the region of prior resection ( Fig. 10 ). BMT of a deep parotid gland may be clinically silent, so CXPA is a consideration if an unusual or irregular-appearing mass presents in the deep lobe.