Abstract
Placenta previa is present in approximately 5 in 1000 pregnancies at the time of delivery, with a higher prevalence noted at midgestation. The diagnosis is made by ultrasound, and patients presenting with vaginal bleeding after 20 weeks’ gestation should be evaluated by transvaginal ultrasound for this condition. Persistent placenta previa at term, within 1 cm of the internal os, necessitates delivery via cesarean section. This diagnosis carries a risk of hemorrhage that persists into the immediate postpartum period.
Keywords
previa, antepartum bleeding, abnormal placentation
Disease
Definition
Placenta previa refers to a placenta located either fully or partially in the lower uterine segment and covering the internal cervical os. Historically, terms such as complete, marginal, and partial were used to describe how much of the placenta was covering the internal os. Transvaginal ultrasonography has improved sonographic description of the precise location of the placenta, and these terms have been abandoned. Any placenta overlying the internal os is now referred to as a placenta previa , negating the need for the complete or partial previa designation. Placentas that are near but not overlying the os are now designated as “low-lying.”
Prevalence and Epidemiology
Placenta previa is estimated to occur in approximately 5 : 1000 pregnancies. Worldwide, the incidence has been found to vary, with a higher incidence noted in Asian studies (12.2:1000 pregnancies) and lower incidences in European, North American, and African studies (2.7:1000–3.6:1000 pregnancies). The incidence of placenta previa is much higher before the third trimester and may exceed 5%; however, upward of 90% of cases resolve as the pregnancy progresses through a process called trophotropism, where the placenta remodels and grows toward the area in the uterus with the best blood supply.
One of the primary risk factors for placenta previa is prior cesarean delivery, and the risk increases with increasing numbers of cesarean deliveries. In these cases, the risk for placenta accreta is also increased, and careful attention should be taken to assess for this condition ( Chapter 98 ). Additional risk factors include a history of placenta previa in a prior pregnancy, advanced maternal age, multiparity, multiple pregnancy, smoking, cocaine use, and previous uterine surgery (i.e., curettage, abortion).
Etiology and Pathophysiology
The exact etiology is unknown, but prior endometrial damage and uterine scarring seem to be associated with development of placenta previa. The presence of a lower uterine scar from a prior cesarean has been suggested to prevent development and growth of the lower uterine segment leading to delayed migration of the placenta away from the internal os. An association with hypoxia has also been suggested. It is known that placentas from women who smoke during pregnancy have a larger surface area to facilitate effective gas exchange and therefore may be more likely to cover the os.
Manifestations of Disease
Clinical Presentation
Classically, placenta previa has been associated with painless vaginal bleeding, although bleeding from a placenta previa can be associated with contractions and abdominal pain. Antepartum bleeding is the most common finding with placenta previa, with 50%–60% of women with placenta previa reporting bleeding during pregnancy. Some women will remain asymptomatic and may only be diagnosed on US or at the onset of labor. Any woman presenting with vaginal bleeding in the second half of pregnancy, especially if painless, should undergo a US, including a transvaginal approach if necessary, to assess for placenta previa before any digital vaginal examination. Measurement of the cervical length via transvaginal US may help predict if women are at increased risk for massive hemorrhage and preterm delivery with placenta previa. One study demonstrated that a cervical length less than 30 mm was significantly associated with increased risk of antepartum hemorrhage necessitating emergency cesarean delivery before 34 weeks’ gestation.
Neonatal complications associated with placenta previa are primarily related to prematurity and include risks such as death, intraventricular hemorrhage, low Apgar scores, anemia, and respiratory distress syndrome. A population-based cohort study from the United States found that approximately 55% of women with a previa deliver before 37 weeks’ gestation, with 17% delivering less than 34 weeks’ gestation. Even controlling for gestational age, at delivery, neonatal risk for respiratory distress syndrome and anemia is increased with placenta previa.
Imaging Technique and Findings
Ultrasound.
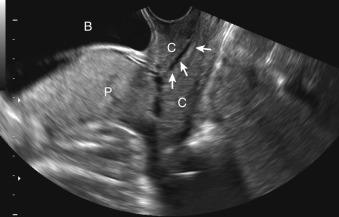
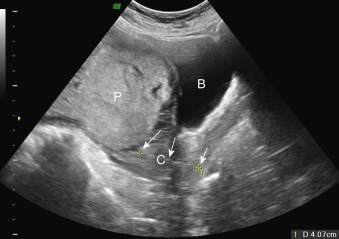
US is the gold standard for diagnosing placenta previa. The vast majority of women in high-income countries undergo routine US screening. Transabdominal US can be used in most cases as a reliable screening exam ( Fig. 106.1 ). One study that found a cutoff of 4.2 cm between the placenta edge and the internal os measured on transabdominal US had a negative predictive value of 99.8%, specificity of 76.7%, and a sensitivity of 93.3% in evaluating placenta previa. Transabdominal US cannot be reliably used in all cases because of uterine contractions, fibroids, overdistended urinary bladder, and fetal positioning, all of which can obscure the placental edge and make measurements inaccurate. Low-lying placentas may be missed on transabdominal US ( Fig. 106.2 ). A false-positive rate of up to 8%–9% has been reported in screening for previa with transabdominal US. Transperineal US has also been used to accurately screen for placenta previa and remains an alternative if patients are resistant to transvaginal US.
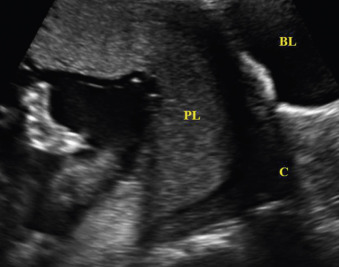
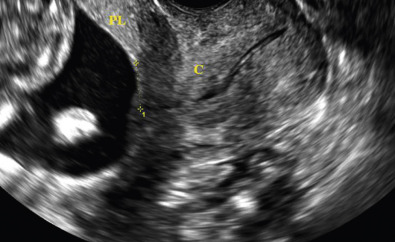
Transvaginal US is the most accurate way to diagnose placenta previa and the true distance from the placental edge to the internal os, especially in cases that are concerning via transabdominal US ( Figs. 106.3 and 106.4 ). This screening method can be used during routine screening of asymptomatic women and must be used before digital examination of women with vaginal bleeding in the second half of pregnancy. The vaginal probe should be inserted while watching the on-screen image to avoid placental manipulation in the case of cervical dilation. The probe should be positioned 2–3 cm away from the cervix so the operator can clearly show the relationship of the placenta to the cervix and internal os. Where there is no placenta previa, the distance between the placental edge and the internal os should be measured.