Abstract
Placental abruption complicates a small fraction of pregnancies but has the potential to carry major maternal and fetal morbidity. As this entity is diagnosed clinically, imaging plays a limited role in diagnosis or management. Management varies based on gestational age and the severity of the abruption at the time of presentation.
Key words
abruption, antepartum bleeding, subchorionic hematoma
Introduction
Placental abruption complicates a small fraction of pregnancies but has the potential to carry major maternal and fetal morbidity. As this entity is diagnosed clinically, imaging plays a limited role in diagnosis and management, which varies based on gestational age and the severity of the abruption at the time of presentation.
Disease
Definition
Placental abruption is defined as the premature separation of a normally implanted placenta after 20 weeks’ gestation and before birth. The separation can be complete, where the entire placenta separates, typically resulting in fetal death, or partial, where only a portion of the placenta separates from the uterus. Abruptions can be “revealed” or “concealed.” A revealed abruption presents with vaginal bleeding as the blood tracks between the decidua and the membranes to the cervix and then to the vagina. A concealed abruption does not present with vaginal bleeding as the bleeding that occurs because of placental separation accumulates behind the placenta without tracking anywhere.
Prevalence and Epidemiology
Placental abruption is a clinical diagnosis that complicates approximately 1.2% of pregnancies in the United States. On pathologic examination of placentas, rates have been found to be as high as 2.1%–3.8%, however, as cases diagnosed solely on pathologic examination do not have clinical consequence, some have suggested that the term should apply to clinical diagnoses only.
The incidence in the United States has slowly increased over the past 30 years in contrast to European countries. The incidence of abruption in Canada was also increasing until the early 2000s when it began to decrease. Over half of cases of abruption occur before 37 weeks’ gestation, with the highest incidence occurring between 24 and 26 weeks’ gestation and decreasing with advancing gestational age.
Many risk factors for placental abruption have been identified, some of which can be adjusted by patient behavior. A history of abruption in a prior pregnancy is the most important nonmodifiable risk factor and increases the risk up to 15- to 20-fold. Additional modifiable and nonmodifiable risk factors are listed in Table 96.1 . Thrombophilia, amniocentesis, chorionic villus sampling, and genetic factors have been implicated; but results from multiple studies are inconsistent, and they are generally not considered to be major risk factors for abruption.
| Nonmodifiable Risk Factors | Modifiable Risk Factors |
|---|---|
|
|
Etiology and Pathophysiology
The physiology behind placental abruption is unknown in many cases, but a few of the risk factors have identifiable pathophysiologic mechanisms. In some cases there are shearing forces that cause the placenta to separate from the wall of the uterus and lead to bleeding, such as in cases of trauma or rapid decompression of the uterus, as seen in delivery of the first infant in a multifetal pregnancy or after rupture of membranes with polyhydramnios. Vasospasm and vasoconstriction of the small arterioles at the decidual-placental interface may lead to areas of hypoxia and necrosis in the decidua. This necrosis leads to venous hemorrhage and causes more of the placenta to separate from the uterine wall, causing more bleeding. This is thought to be the cause in cases where cocaine, shock/sepsis, or hypertensive urgency are the etiology of the abruption.
The majority of cases seem to suggest a long-standing process starting at the time of trophoblastic invasion in the first trimester. This inadequate invasion leads to the lack of adequate remodeling of the uterine arterioles, similar to what is seen in pregnancies complicated by preeclampsia. This correlates with the abnormal serum analytes seen in cases of placental abruption, particularly low pregnancy-associated plasma protein A and increased alpha-fetoprotein that are associated with abnormally formed or damaged villi. This theory is further supported by the association between preeclampsia and growth restriction in pregnancies complicated by abruption. In addition, there is an association between a history of abruption and an increased risk of hypertensive disorders in a subsequent pregnancy. Regardless of the initial cause, the end of the pathophysiologic pathway involves separation between the placenta and the decidua because of retroplacental bleeding, which decreases the functional surface area of the placenta and can lead to further separation and bleeding.
Manifestations of Disease
Clinical Presentation
The classic presentation of placental abruption is abdominal pain and bleeding, but the presence or absence of symptoms is not necessarily indicative of the severity of the abruption. In cases of concealed abruption, there will be no bleeding in approximately 10% of cases. Back pain can also be the presenting symptom if there is a posterior placenta. Physical examination findings range from a benign exam to findings of a firm, tender uterus or uterine tenderness and evidence of preterm labor. Tocography may show uterine contractions, which may be seen as high-frequency, low-amplitude contractions. When more than 50% of the placenta has separated, the fetal heart rate may show minimal to absent variability and/or recurrent variable and late decelerations.
Maternal complications associated with abruption are related to hypovolemia and blood loss. In cases of mild abruptions there may be no maternal sequelae. With more significant abruptions and increased blood loss, maternal complications can include hypotension, shock, disseminated intravascular coagulopathy, and associated end-organ damage. The retroplacental bleeding can cause uterine irritation and contractions leading to preterm labor. Bleeding into the uterus can cause uterine atony and can give the uterus a bluish hue, known as a Couvelaire uterus. This atony can increase the risk of blood loss caused by atony and associated complications. In rare cases, large amounts of bleeding can lead to maternal death.
Fetal complications are secondary to decreased functional capacity of the placenta. Decreased functional surface area of the placenta can lead to fetal hypoxia and morbidity related to preterm delivery. In cases where greater than 50% of the placenta is separated from the wall of the uterus, intrauterine fetal demise can occur. Perinatal mortality can approach 20% to 30%, and persists after accounting for mortality related to preterm delivery. Pregnancies complicated by chronic abruption may be complicated by preterm labor, preterm premature rupture of membranes, oligohydramnios, and fetal growth restriction.
Imaging Technique and Findings
Ultrasound.
Placental abruption is a clinical diagnosis, and the main role of imaging in abruption is to rule out placenta previa or other abnormal placentation as a cause of vaginal bleeding.
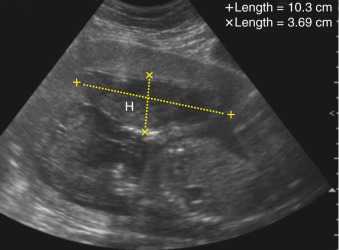
The hematoma formed from an abruption is most commonly visualized in the subchorionic area ( Fig. 96.1 ). This hematoma is believed to be secondary to abruption at the placental margin and correlates with the fact that first-trimester bleeding and subchorionic hematomas increase the risk for placental abruption ( Fig. 96.2 ). A retroplacental location for bleeding and clot formation is more common after 20 weeks’ gestation ( Fig. 96.3 ). A preplacental hematoma is the least common, occurring only in about 1% of cases ( Fig. 96.4 ). The echotexture of the blood varies with time compared to the initial abruption. Blood initially appears hyperechoic to isoechoic when compared to the placenta and may be interpreted as a thick placenta. By 1 week from the initial event, the blood becomes hypoechoic ( Fig. 96.5 ), and by 2 weeks it is usually sonolucent.