Etiology, Prevalence, and Epidemiology
Pneumomediastinum, also known as mediastinal emphysema, refers to the presence of free air or other gas in the mediastinal space. Pathologically, the major sources of entry of air to the mediastinum are (1) through the skin and chest wall, as commonly seen in penetrating trauma; (2) from the neck; (3) from a tear or defect in the esophagus or the trachea, allowing air to enter the mediastinum directly; (4) from ruptured alveoli; and (5) from the abdominal cavity.
Most cases of pneumomediastinum are related to alveolar rupture and can be clinically divided into two categories: (1) “spontaneous” pneumomediastinum and (2) “barotrauma,” or pneumomediastinum occurring during positive-pressure ventilation or associated with other externally applied distending pressures.
The term pneumomediastinum usually refers to the presence of abnormal air within the mediastinum without associated infection. However, gas can form in the mediastinum during acute bacterial mediastinitis caused by gas-producing microorganisms or resulting from communication with the esophagus (e.g., Boerhaave syndrome), respiratory tract (e.g., necrotizing pneumonia), or head-neck soft tissue infection (e.g., cervical adenitis). Moreover, acute mediastinitis may also occur with cardiovascular or other thoracic surgical procedures.
Primary pneumomediastinum, also known as spontaneous pneumomediastinum, is generally described as a benign condition, manifesting in young adults exposed to a sudden pressure change within the intrathoracic cavity. It may occur after involuntary alterations in the breathing pattern, such as asthma, violent coughing or vomiting, and athletic competition. Other conditions associated with spontaneous pneumomediastinum include seizures, croup, marijuana or crack cocaine smoking, nitrous oxide inhalation, pneumonia, diabetic ketoacidosis, diffuse interstitial pulmonary fibrosis, and parturition. The majority of patients with spontaneous pneumomediastinum have predisposing factors that cause a sudden rise in alveolar pressure leading to alveolar rupture.
Idiopathic spontaneous pneumomediastinum (Hamman syndrome or Macklin syndrome) is a rare self-limited condition described in young adult men without a history of a potential predisposing cause and normal lung parenchyma at computed tomography (CT). The physical examination usually reveals subcutaneous air in the suprasternal notch and the Hamman sign, which is a crunching or clicking noise synchronous with the heartbeat and is best heard in the left lateral decubitus position.
Mechanical ventilation with positive end-expiratory pressure has long been recognized as a traumatic source of pneumomediastinum in intensive care unit patients. In some cases extraalveolar air originating from disrupted alveoli may appear below the diaphragm as either pneumoperitoneum or pneumoretroperitoneum. In addition, gas from the anterior mediastinum can dissect through the diaphragm into the anterior abdominal extraperitoneal space resembling intraperitoneal air. Loculated thoracic air collections can develop in mechanically ventilated neonates with acute lung injury or acute respiratory distress syndrome. Barotrauma-associated posterior tension pneumomediastinum is a rare cause of cardiac tamponade in a ventilated neonate. Moreover, on the chest radiograph, the cardiac shadow may be obscured because of flattening of the heart from tension pneumomediastinum (“vanishing heart”).
Secondary pneumomediastinum has been identified as a result of a specific injury or pathologic condition, such as blunt or penetrating trauma, recent interventions in the esophageal or tracheobronchial tree, rupture of a hollow viscus, tissue dissection originating from a spontaneous pneumothorax, or pulmonary or mediastinal infection caused by gas-forming organisms.
The causes of pneumomediastinum are shown in Table 75.1 . The reported clinical settings associated with alveolar rupture are shown in Table 75.2 .
| HEAD AND NECK |
|
| MEDIASTINUM |
|
| ABDOMEN |
|
| PULMONARY |
| Associated With Abnormal Lung Parenchyma |
|
| Associated With Airway Anomalies |
|
| ELEVATED INTRAALVEOLAR PRESSURE ASSOCIATED WITH CLINICAL ABNORMALITIES |
|
| ELEVATING INTRAALVEOLAR PRESSURE WITHOUT CLINICAL ABNORMALITY |
|
| SPONTANEOUS |
| Deliberate Alteration in Breathing Pattern |
|
| Straining and Other Involuntary Alterations in Breathing Pattern |
|
| Associated Lung Diseases |
|
| CAUSED BY EXTERNAL PRESSURE CHANGES (BAROTRAUMA) |
| Decompression: Gas Expansion |
|
| Positive Intrathoracic Pressure of External Origin |
|
| Elevated Intraalveolar Pressure Associated With Clinical Abnormalities |
|
Clinical Presentation
Often misdiagnosed because of its vague manifestations, spontaneous pneumomediastinum must be part of the differential diagnosis of a patient presenting with chest pain or discomfort. Chest pain occurs in 80% to 90% of patients with spontaneous pneumomediastinum and represents the second most common cause of admission of young, healthy individuals experiencing sudden chest pain or shortness of breath. The clinical presentation depends on the amount of air in the mediastinum and on the presence or absence of associated infection. Chest pain is characteristically retrosternal and aggravated by breathing and position changes ; dyspnea is present in about 50% of the cases. On occasion, patients are asymptomatic. Pneumomediastinum occurring in a patient on mechanical ventilation is potentially disastrous because of its frequent association with tension pneumothorax. In this clinical setting the diagnosis may be suggested by a history of sudden deterioration marked by hypotension and increased pulmonary pressures.
Tension pneumomediastinum is a rare, potentially fatal complication caused by large amounts of air in the mediastinum and a substantial increase in intramediastinal pressure that can lead to hemodynamic compromise. Although uncommon, tension pneumomediastinum may result in acute diastolic dysfunction, cardiac tamponade, impaired venous return to the heart, and airway distortion that impedes air flow. Percutaneous CT-guided insertion of a mediastinal drainage catheter is a useful procedure to perform before the development of cardiac tamponade.
Pathologic Findings and Pathophysiology
The pathophysiology of pneumomediastinum depends on the different clinical scenarios in which it is seen. Anatomically, the mediastinum communicates with several structures, including the submandibular space, the retropharyngeal space, and the vascular sheaths in the neck. There is a tissue plane that extends anteriorly from the mediastinum to the retroperitoneal space through the sternocostal attachment of the diaphragm. This space is continuous with the flanks and extends to the pelvis. The mediastinum also communicates directly with the retroperitoneum by way of the periaortic and periesophageal fascial planes.
In the presence of a pressure gradient between an alveolus and the interstitium, air ruptures from the alveolus into the perivascular and peribronchial fascial sheath. The Macklin effect relates to a three-step pathophysiologic process: blunt traumatic alveolar rupture, air dissection along bronchovascular sheaths, and spreading of this pulmonary interstitial air into the mediastinum. Because the mean pressure in the mediastinum is always somewhat negative with respect to the pressure in the pulmonary parenchyma, air tends to move centrally, perhaps facilitated by the pumping action of breathing. On occasion, air will dissect peripherally, resulting in subpleural air cysts. Pulmonary interstitial emphysema is typically a transient phenomenon; it rarely persists, and CT is helpful in making this diagnosis.
Spontaneous pneumomediastinum commonly occurs in healthy young men in whom an increased intraalveolar pressure (e.g., Valsalva maneuver, cough, emesis) leads to the rupture of marginal pulmonary alveoli. On occasion, asymptomatic spontaneous epidural emphysema has been incidentally described in asthmatic patients.
Blunt thoracic trauma is usually associated with simultaneous injuries to adjacent structures, such as great vessels, the esophagus, and osseous structures. Tracheobronchial injuries occur in less than 1% of blunt chest trauma patients. Pneumomediastinum in trauma patients may occur from alveolar rupture or fracture of a central airway. Isolated tracheobronchial injury is unusual because of the proximity of other major structures, such as great vessels, but has been reported in young individuals in whom the blood vessels are more compliant. Sudden deceleration injury resulting from a motor vehicle accident or fall from great heights may result in a tear or a total disruption of either the right or left main bronchus. Because of the relative fixation at the carina, the majority of airway injuries are within 3 cm of the carina. Pneumomediastinum may also be a consequence of airway or bronchial laceration during bronchoscopy, tracheotomy, endotracheal intubation, and overinflation of the endotracheal tube cuff.
Pneumomediastinum may occur with esophageal perforation during upper gastrointestinal endoscopy, after the ingestion of a caustic substance such as paraquat, or from spontaneous esophageal rupture as occurs in Boerhaave syndrome. Pneumomediastinum has also been described after treating esophageal varices with endoscopic intravascular sclerotherapy.
A continuum of fascial planes connects cervical soft tissues with the mediastinum and retroperitoneum, permitting aberrant air arising in any one of these areas to spread elsewhere. Air dissecting downward into the mediastinum may be secondary to different head-neck infections. The most common causes include retropharyngeal or dental abscess, cervical adenitis, salivary gland infection, tonsillitis, and osteomyelitis of the facial bones. Surgical procedures involving the upper respiratory tract may produce air in the neck through breaches either in the oropharyngeal mucosa or in the trachea.
Mediastinal air can also arise from below the diaphragm. Air may dissect into the mediastinum from the retroperitoneal space after perforation of a hollow viscus, ulcerative colitis, sigmoid diverticulitis, pneumatosis cystoides intestinalis, “rectal barotrauma,” and procedures such as sigmoidoscopy, colonoscopy, and barium enema.
Imaging Findings
Radiographic Findings
Chest radiography has a low sensitivity to detect pneumomediastinum. The typical radiographic appearance is that of linear interstitial air collections. Dissection of air along tissue planes may be more obvious on the lateral projection, showing an increase in the depth and lucency of the retrosternal space. It is also recognized by streaks of gray-black density separating portions of mediastinal pleura from mediastinal contents or focal bubble-like or larger collections of gas outlining the mediastinal structures ( Fig. 75.1 ). Abnormal mediastinal air appears as vertical streaks of radiolucency just within the lateral borders of the mediastinal shadow. The parietal pleura is peeled off from the mediastinal structures and is seen as a line, parallel to and separated from the heart and mediastinum by a band of translucent air ; this line is best seen on the left side but may be easily overlooked ( Figs. 75.2 and 75.3 ). In addition, the borders of the heart, aorta, and thymus appear more sharply outlined. Streak-like areas of radiolucency produced by mediastinal air are sometimes more clearly appreciated on the lateral view.



Sometimes, air in the peribronchial sheaths can be detected radiographically, most commonly in premature infants with surfactant deficiency. Unlike air bronchograms, pulmonary interstitial emphysema does not branch and is usually subtle and disorganized. In neonates a loculated mediastinal air collection appears as a rounded hyperlucent cystic lesion adjacent or overlying the mediastinum ( Fig. 75.4 ).

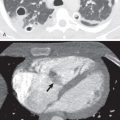
Alveolar rupture from the high airway pressures used in the treatment of acute respiratory distress syndrome (ARDS) may cause interstitial dissection of gas peripherally and the formation of “subpleural air cysts.” These thin-walled, rounded air collections are occasionally detected radiographically, and their recognition is an early manifestation of pulmonary barotrauma. Although these findings are difficult to identify on radiographs, they can be easily seen on CT scans ( Figs. 75.5 and 75.6 ).