Abstract
Polyhydramnios is an excessive amount of amniotic fluid, occurring in 1% of pregnant women. It can be defined by an absolute value or a gestational age–specific value utilizing single deepest pocket (SDP), or amniotic fluid index (AFI), or subjectively. Specific definitions commonly used include an AFI ≥24 cm or SDP ≥8 cm cutoffs. Approximately 50% to 60% are idiopathic; in the others, etiology includes diabetes, multiple gestations, fetal aneuploidy, and congenital defects such as fetal neurologic or musculoskeletal disorders, fetal anemia, and genetic syndromes. Polyhydramnios is usually chronic, but acute polyhydramnios with sudden severe increase in amniotic fluid may cause maternal dyspnea, with marked risks of premature delivery, neonatal morbidity, and neonatal mortality. Treatment, which is individualized and based on the etiology and gestational age, could include amnioreduction (if clinical symptomatology), diabetes diagnosis and management, prenatal diagnostic procedures, or cordocentesis with intrauterine blood transfusion or laser ablation of placental vascular anastomoses. Because of associated increased fetal morbidity and mortality with polyhydramnios, serial fetal monitoring is indicated. Intrapartum complications due to polyhydramnios include macrosomia, uterine atony malpresentation, preterm labor, placental abruption, cord prolapse, and cesarean delivery, which all further increase maternal and neonatal morbidity and require vigilance and appropriate management.
Keywords
amniotic fluid index, AFI, single deepest pocket, SDP, acute polyhydramnios, amnioreduction
Introduction
Polyhydramnios (also called hydramnios ) is defined as an excessive amount of amniotic fluid. Although idiopathic in more than 50% of cases, it may be associated with maternal and fetal disorders. Polyhydramnios should prompt a detailed fetal anatomic ultrasound (US) scan and maternal evaluation.
Disease
Definition
An amniotic fluid volume greater than 2000 mL constitutes polyhydramnios, but accurate measurement requires invasive study and is difficult to assess clinically. In practice, ultrasonography methods used for diagnosing polyhydramnios include subjective assessment, single deepest pocket (SDP), or amniotic fluid index (AFI). Polyhydramnios is defined by an absolute value or a gestational age–specific value. Some clinicians prefer the latter because the amniotic fluid volume changes throughout pregnancy, increasing linearly until the early third trimester and then remaining constant until term. A recent study of 482 AFI and 468 SDP pregnancies with dye-determined amniotic fluid volumes between 15 and 41 weeks, demonstrated that both AFI and SDP correlated with actual amniotic fluid volume.
Definitions of polyhydramnios vary and include AFI of ≥18 cm, ≥20 cm, ≥24 cm, ≥25 cm or SDP of ≥8 cm. Polyhydramnios has been further classified as mild (AFI 24–30 cm, SDP 8–11.9 cm), moderate (AFI 30.1–35 cm, SDP 12–15.9 cm), and severe (AFI > 35 cm, SDP 16 cm).
In gestational age–specific percentile charts, polyhydramnios is usually considered as ≥95th percentile or ≥97.5th percentile.
Prevalence and Epidemiology
Polyhydramnios affects approximately 1% of pregnancies (range 0.2%–3.9%) and has no apparent ethnic or geographic distribution. Prevalence is affected by diagnostic criteria, but it is seen more frequently with certain conditions including diabetes, multiple gestations, fetal aneuploidy, and congenital defects such as fetal neurologic or musculoskeletal disorders, fetal anemia, and some genetic syndromes.
Etiology and Pathophysiology
Excessive production or decreased uptake of amniotic fluid can cause polyhydramnios. The former may result from increased urination by the fetus or increased transudation of fluid from exposed fetal surfaces. Fetal diuresis in cases of high cardiac output or borderline cardiac failure may be caused by elevated atrial natriuretic peptide or brain natriuretic peptide. Decreased uptake may occur from decreased swallowing of amniotic fluid by the fetus, usually secondary to neurologic dysfunction, esophageal compression, or atresia or other gastrointestinal obstructions ( Table 119.1 ).
| Pathophysiology | Etiology |
|---|---|
| EXCESSIVE PRODUCTION OF AMNIOTIC FLUID | |
| Increased fetal cardiac output and/or polyuria | Uncontrolled maternal diabetes |
| Twin transfusion syndrome | |
| Macrosomia | |
| Fetal hydrops | |
| Congenital infections | |
| Fetal anemia (e.g., isoimmunization, parvovirus infection) | |
| Fetal tumors (e.g., sacrococcygeal tumors) | |
| Placental tumors (e.g., chorioangioma) | |
| Congenital cardiac defects | |
| Fetal Bartter syndrome | |
| Anencephaly (lack of antidiuretic hormone) | |
| Fetal diarrhea | Congenital chloride diarrhea |
| Congenital sodium diarrhea | |
| Increased transudation from exposed fetal surfaces | Anencephaly |
| Spina bifida | |
| DECREASED UPTAKE OF AMNIOTIC FLUID | |
| Neurologic dysfunction most likely causing decreased swallowing | Encephalopathy (white matter atrophy) |
| Anencephaly (lack of swallowing reflex) | |
| Fetal akinesia deformation sequence | |
| Chromosomal anomalies (trisomies 21, 13, and 18) | |
| Craniofacial dysfunction or obstruction | Pharyngeal teratoma (epignathus) |
| Cleft lip | |
| Choanal atresia | |
| Fetal goiter | |
| Gastrointestinal obstruction | Tracheoesophageal fistula |
| Esophageal atresia | |
| Duodenal atresia | |
| Other intestinal atresia | |
| Midgut volvulus | |
| Gastroschisis | |
| Omphalocele | |
| Mesenteric cysts | |
| Imperforate anus | |
| External gastrointestinal compression | Congenital diaphragmatic hernia |
| Cystic adenomatoid malformation | |
| Skeletal dysplasia | |
| Unilateral massive multidysplastic kidney | |
Common causes of polyhydramnios include congenital anomalies or aneuploidy or genetic disorders (6%–45%), maternal diabetes (5%–25%), multiple gestations (7%–10%), and fetal anemia (1%–11%). In one review of 672 pregnancies complicated by polyhydramnios, maternal diabetes accounted for 7% of cases; aneuploidy, 2%; and congenital anomalies, 11%. In addition, the rate of anomalies was associated with the degree of polyhydramnios; 31% of fetuses with severe polyhydramnios (≥30 cm) had anomalies compared with 12% of fetuses with moderate polyhydramnios (25–29.9 cm), and 8% with mild polyhydramnios (20–24.9 cm).
Idiopathic polyhydramnios is defined as polyhydramnios, or excess amniotic fluid volume, which is not associated with congenital fetal anomalies, maternal diabetes, isoimmunization, fetal infection, placental tumors, or multiple gestations. Approximately 50%–60% of all cases of polyhydramnios are classified as idiopathic in etiology. A review of literature on idiopathic polyhydramnios from 1950 to 2007 revealed an increase in the risk of adverse pregnancy outcomes, and a two- to fivefold increase in the risk of perinatal mortality when compared to pregnancies without polyhydramnios.
Manifestations of Disease
Clinical Presentation
Polyhydramnios should be suspected when uterine size is larger than expected dates. It is usually gradual and chronic and associated with mild maternal discomfort. However, acute polyhydramnios is a potentially critical situation in which a sudden severe increase in amniotic fluid results in rapid increase of maternal abdominal size, often causing dyspnea, abdominal discomfort, uterine tenderness, and contractions. The prognosis for untreated acute polyhydramnios is worse than for chronic polyhydramnios, with marked risks of premature delivery, neonatal morbidity, and mortality. Amnioreduction (serial large-volume amniocentesis) is indicated if clinical symptoms would be improved by removing amniotic fluid (see later) or for disorders such as twin transfusion syndrome ( Chapter 162 ).
Imaging Technique and Findings
Ultrasound.
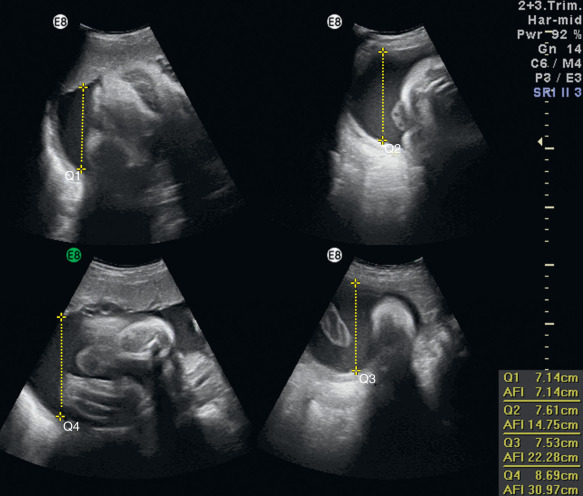
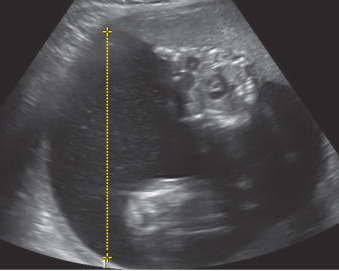
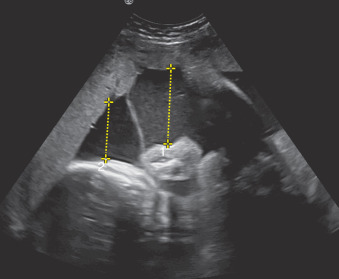
Amniotic fluid volume is evaluated via AFI or SDP. AFI is a sum of the deepest vertical pocket in each quadrant of the uterus excluding umbilical cord loops or fetal parts ( Fig. 119.1 ). SDP is a measure of the SDP of fluid ( Fig. 119.2 ). In multiple pregnancies, SDP for each fetus is typically reported ( Fig. 119.3 ).