Positron Emission Tomography
Cameron C. Foster
Bijan Bijan
David K. Shelton
Introduction
PET imaging is the basis of molecular imaging in today’s clinical practice. The new hybrid imaging instrument, PET-CT (PET plus CT), combines anatomic and physiologic imaging and opens a door to a new era in radiology and nuclear medicine. Currently the clinical applications of PET imaging are focused in four main areas: (1) oncology, comprising about 80% of the current practice of clinical PET; (2) neurologic applications (Alzheimer disease and epilepsy); (3) cardiac applications (coronary artery disease and myocardial viability); and (4) infection and inflammation imaging (fever of unknown origin and immunocompromised patients). With the expanding approval of reimbursement of PET for more indications, the number of PET scanners has increased dramatically throughout the United States.
PET Instrumentation. PET imaging is based upon positron emitters, which are used as labeling tracers for metabolic molecules. The most common positron-emitting radionuclides include fluorine-18 (F-18), nitrogen-13 (N-13), oxygen-15 (O-15), carbon-11 (C-11), and rubidium-82 (Rb-82). The bulk of current clinical PET imaging is based on F-18, an unstable radioisotope with a half-life of 109 minutes that is produced in a cyclotron. Its relatively short half-life requires that imaging be performed within relatively short-transit proximity to a cyclotron, though regional distribution centers now allow for the delivery of tracer material to the intended imaging center up to several hours away. Other positron emitters have even shorter half-lives (75 seconds to 20 minutes) and must be imaged at the cyclotron site within minutes of their production or closer still with a generator, in the case of rubidium-82, next to the scanner itself. The decay of positron-emitting atoms results in the release of a positron, which has the same mass as an electron but is positively charged. Within milliseconds of emission, the positron annihilates with a nearby electron to release two high-energy (511 keV) γ-ray photons. The distance the positron travels away from the parent atom prior to annihilation is directly proportional to the energy of the parent atom. Thus higher energy parent atoms such as Rb-82 will have a higher “positron travel” than lower energy parent atoms such as F-18. This directly influences image resolution. These photons move apart in opposite directions (a near 180° angle). Because of their high energy, these photons are highly penetrative in soft tissue and therefore leave the body with limited absorption or deflection.
The PET imaging system consists of a ring of scintillation detector set to detect coincident photons that strike the detectors within a very narrow time window. Noncoincident, mostly scattered, photons are rejected from the data set. Simultaneous detection of two 511-keV photons by any two detectors indicates that an annihilation event has occurred somewhere in the column of space between the two detectors. These raw data projections are reconstructed into cross-sectional images by algorithms similar to those used in CT and MR. PET scans viewed alone provide limited morphologic detail and can be difficult to interpret. Spatial resolution of current PET systems is 4 to 5 mm. Systems under development improve spatial resolution to 2 mm. Newer systems utilizing advancements in crystal design and electronics now allow for “Time of Flight” (TOF) imaging. TOF utilizes the timestamp of when each photon of a matched coincident pair reaches the detector. Using this timestamp, the site of annihilation can be narrowed down from existing along the line of coincidence to encompass a smaller subsection of the line of coincidence. This, when performed properly, can improve image resolution and lesion detection.
Hybrid instruments combine PET scanners with CT scanners and have now virtually supplanted all new scanner installations compared to dedicated PET systems. CT provides excellent anatomic detail but lacks functional information. PET provides metabolic measurements and functional information but lacks precise morphology. The union of the two allows correlation of complementary findings into a single comprehensive examination. A typical PET-CT scanner consists of a PET scanner immediately adjacent to an MDCT scanner. A patient couch, accurately calibrated for position, runs through both scanning assemblies. Scans may be obtained
either from instrument independently or from both simultaneously. Computer software is used to fuse the two sets of images into composite images.
either from instrument independently or from both simultaneously. Computer software is used to fuse the two sets of images into composite images.
Attenuation correction must be applied to PET images. Attenuation of either of the paired photons by absorption or scatter would result in rejection of data and nondetection of annihilation events. Attenuation is increased when the origin of the photons is from deeper within the body because of the greater thickness of intervening soft tissues.
Correspondingly, attenuation is less in the thorax because of the air-filled lungs than in the abdomen or pelvis. The CT transmission data is used to create an attenuation map that is applied to the PET images to compensate for attenuation defects. The attenuation correction process increases sensitivity for detection of positron activity; but, it may introduce artifacts into the images if there is motion which in turn creates misregistration between the PET and CT data sets. Therefore, PET optimal interpretation includes viewing of both attenuation-corrected and attenuation-uncorrected PET image.
Performing PET-CT. In the case of F-18 FDG scans, patients fast for 4 to 6 hours prior to the scan to limit metabolic activity with the GI tract as well as limiting the amount of circulating insulin. Blood glucose should be under good control (<150 mg/dL) to limit the competition for FDG uptake by glucose. Insulin administration and oral diabetic medication should be held prior to FDG injection to prevent shifting uptake into muscle tissue. The timing of the last insulin dose varies by the route of administration and the type of insulin being used. Strenuous activity should be limited for 24 hours prior to and immediately following radionuclide administration to limit muscle uptake of FDG. Speech should be curtailed after injection, especially in patients being studied for head and neck malignancy to limit FDG uptake in the muscles of the head and neck and larynx. The bladder is emptied by voiding or catheterization just prior to scanning. Manual or continuous irrigation of the bladder with saline and scanning the pelvis first is helpful in limiting bladder activity that may obscure disease activity in the uterus, ovaries, or pelvic lymph nodes. The usual dose is 10 to 20 mCi (0.22 mCi/kg body weight) given by IV injection. Pediatric patient’s minimum dose should not go below 2 mCi. Scanning is performed approximately 60 minutes after IV injection of FDG to allow time for cellular uptake of FDG and clearance of FDG from the blood to decrease background activity. The patient lies supine on the scanning table with arms overhead or at the sides. The arms-at-side position is preferred for head and neck scanning, whereas holding the arms overhead is best for body scanning. Patients scanned with the arms at the sides also may generate beam-hardening artifacts (see Fig. 63.5). Whole-body CT scans from the top or base of the skull through the neck, chest, abdomen, and pelvis are performed, usually without IV administration of CT-contrast agents. Some institutions prep the bowel with oral contrast as part of patient preparation. While administration of IV and/or oral-iodinated contrast agents would make the CT more diagnostic, it introduces artifacts in attenuation correction for the PET images and will alter standardized uptake values (SUVs). MDCT scanning generally takes less than 2 minutes. PET scanning is performed over 10 to 30 minutes, depending upon the area covered, number of acquisitions, and scanner speed. CT and PET images are reconstructed separately and then fused into composite images utilizing image readout software.
PET-CT Interpretation. Axial, coronal, and sagittal reformatted CT; attenuation-corrected PET; attenuation-uncorrected PET; and fused PET-CT images are viewed interactively on a workstation (Fig. 63.1). Software allows the rotation of maximum intensity projection (MIP) images to aid in the localization of tracer activity. Window width and level settings are optimized interactively. Assessment of normal and pathologic radiotracer uptake is made by visual inspection, by the standardized uptake value (SUV), and by glucose metabolic rate calculation.
F-18 FDG is currently the most widely used and applicable tracer in PET-CT imaging. Understanding its properties is fundamental for interpreting the bulk of PET-CT scans. F-18 is the radioisotope in the radiotracer molecule 2-[fluorine-18]fluoro-2 deoxy-D-glucose (FDG). FDG is an analog of glucose and tends to concentrate in areas of high metabolic activity everywhere in the human body. Predominantly, tumor cells with a high rate of mitosis are highly metabolically active and have an increased number of glucose transporters, thus concentrating FDG in tumor cells in higher concentrations than in normal tissue. FDG distributes and is taken up by active glucose transport through the cell membrane exactly like regular glucose. It is subsequently phosphorylated to F-18 FDG-6-phosphate. Unlike glucose, F-18 FDG-6-P is not further metabolized, neither forward nor reverse, and is thus concentrated in tissues in which it accumulates. The major exception to metabolic trapping is in the liver, where concentrated phosphatase enzymes dephosphorylate FCG-6-phosphate and clear FDG from the liver. FDG accumulation depends on the blood supply of the tissue and the level of the glycolytic metabolic activity of the tissue. Organs with higher metabolic activity, like the brain, will accumulate more FDG. Multiple factors, including blood sugar level, blood insulin level, and muscular activity, affect the biodistribution of FDG. FDG is excreted mainly in the urine, like glucose. However, in contrast to glucose, FDG cannot be reabsorbed in proximal convoluted tubules. Thus, the urinary system shows intense activity. Variable activity of the GI tract, liver, thymus, breast, salivary glands, and bone marrow is also commonly seen. The uptake by myocardium largely depends on the metabolic state of the heart at the time of the injection. Accumulation of FDG is also seen in interstitial body fluids, including pleural, peritoneal, and synovial fluids. Variable excretion from lacrimal, salivary, and sweat glands needs to be recognized as variants on PET images and not mistaken for hypermetabolic lesions.
FDG is an indiscriminate identifier of foci of high metabolic activity within the body. Its usefulness is based on the fact that most malignant tumors are more metabolically active and take up more glucose than normal tissues. Some nonmalignant pathologic processes, such as infections, foci of inflammation, and benign neoplasms, also concentrate FDG on the basis of their metabolic activity. The challenge to PET interpretation is the differentiation of pathologic activity from normal and normal variant FDG activity.
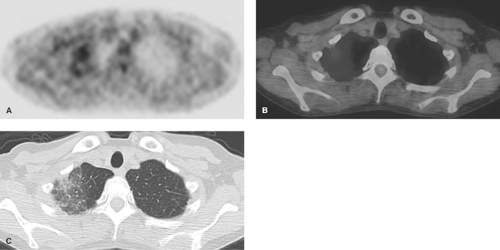
Skeletal muscle FDG uptake is dependent on muscle activity and insulin levels. In a resting state, muscle uptake of FDG is negligible. Heavy muscle activity in the 24 hours prior to imaging may result in high FDG uptake. Patients should minimize activity following FDG injection to minimize uptake by skeletal muscles. Patients with breathing difficulty may show prominent uptake in the muscles of the chest wall and diaphragm. Insulin injection by diabetics increases skeletal muscle FDG uptake as also seen with nonfasting patients. Talking and eye movement increase uptake in the ocular muscles, the larynx, and the muscles of mastication (Fig. 63.2).
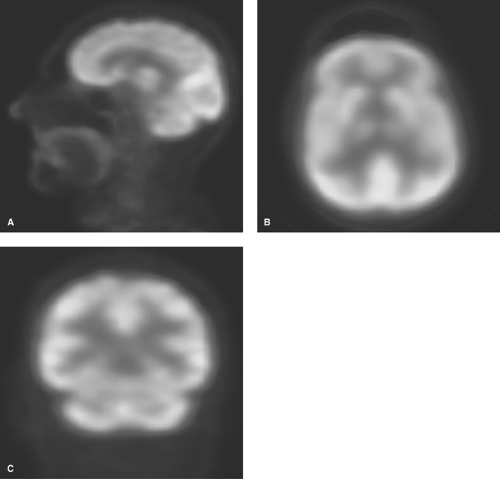
Brain uptake of FDG is always prominent because the brain uses glucose as its primary energy source (Fig. 63.3). Normal gray matter uptake is particularly avid and difficult to differentiate from malignant brain lesions. Focal low-level activity may be seen in areas that have been radiated or resected.
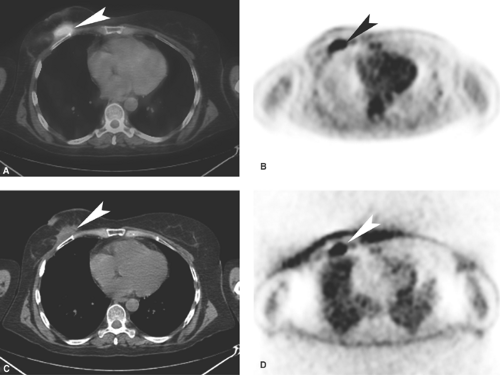
Cardiac muscle uptake is particularly prominent after eating. Fasting for 4 to 6 hours prior to FDG scanning decreases FDG uptake as the myocardium switches to fatty acid metabolism. Most patients show variable and nonuniform myocardial FDG activity, even after a fast, caused by nonuniform transition to fatty acid metabolism by the myocardium. Hibernating
myocardium will preferentially use glucose for metabolism and thus will have high uptake of FDG. FDG activity is most variable at the base of the LV (Fig. 63.4).
myocardium will preferentially use glucose for metabolism and thus will have high uptake of FDG. FDG activity is most variable at the base of the LV (Fig. 63.4).
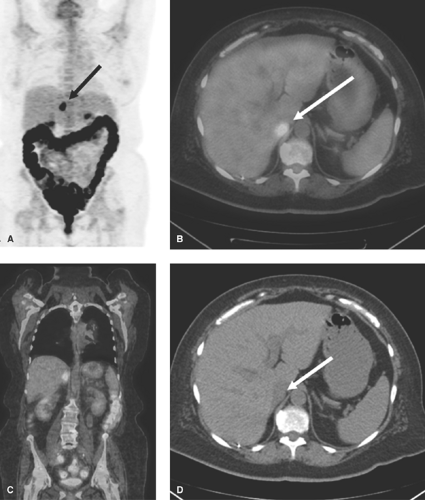
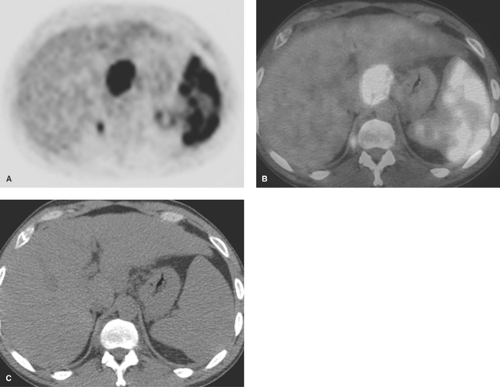
Liver. The entire liver demonstrates low-level FDG activity in nearly all patients. Most challenging is the fact that uptake often appears heterogeneous, mimicking the appearance of multiple small metastases (Fig. 63.5). Hepatic uptake of FDG is not surprising because the liver is a major site of carbohydrate metabolism, glycolysis, and glycogen storage. However, hepatocytes have high levels of FDG-6-phosphatase, which acts to clear FDG from hepatocytes. Primary liver tumors may demonstrate high FDG-6-phosphatase activity, have high rates of clearance of FDG, and be difficult to detect on PET images. In summary, FDG PET is limited to the detection of small liver metastases and small primary liver tumors. Detection of lesions below 1 cm in size can be problematic because of this.
Gallbladder activity is rarely seen. FDG activity in the gallbladder bed suggests acute or chronic cholecystitis, gallbladder cancer, or adjacent liver tumor.
Spleen activity is usually slightly greater than blood pool but normally less than liver. Spleen uptake is substantially increased by the activation of extramedullary hematopoiesis and can also be seen in the setting of postchemotherapy treatments.
Bone marrow radionuclide activity is mild to moderate, diffuse, and symmetric within the spine, pelvis, ribs, sternum, and proximal femurs. Asymmetric or heterogeneous uptake is caused by skeletal metastases, old fractures, effects of radiation therapy, and activation of hematopoiesis by severe anemia and marrow rebound postchemotherapy with or without marrow-stimulating medications.
Stomach activity is usually low level and best recognized on axial images by its characteristic position and shape. FDG activity is accentuated by stomach muscle contraction. Foci of uptake in the lower thorax may represent inflammation within a hiatal hernia or in the distal esophagus related to reflux.
Colon activity is highly variable and usually more intense than in the small bowel. Intense FDG uptake makes the recognition of pathologic sites in the abdomen difficult (Fig. 63.6). Colon activity varies with colon muscle contraction, mucosal inflammation, amount of lymphoid tissue in the colon wall, and possibly uptake by colon bacteria. Multifocal or segmental activity suggests inflammatory bowel disease, while intense focal activity suggests colon carcinoma, malignant peritoneal implants, or adjacent lymph node metastases. Focal activity can also be seen in benign entities such as hyperplastic polyps.
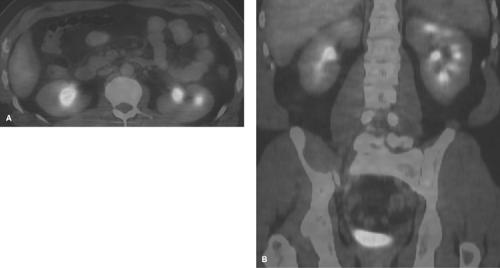
Urinary Tract. FDG is excreted by glomerular filtration without significant renal tubular reabsorption. This results in concentrated radionuclide activity in the urine (Fig. 63.7). The bladder should be emptied prior to PET imaging. Good hydration facilitates FDG clearance and decreases collecting system activity. High (but normal) renal collecting system activity impairs the detection of small renal lesions. Partial filling of the ureters resulting from normal peristalsis may show focal high FDG activity anywhere along the course of the ureters. Bladder diverticula commonly retain urine with FDG even after bladder emptying.
Uterus. The endometrium commonly demonstrates intense radionuclide activity during active menstruation. Activity may also be seen from menstrual blood in vaginal tampons. Pelvic endometriosis is a benign cause of high-activity foci in the pelvis. Fibroids may also have mild FDG activity in many patients.
Ovaries show uptake in functional ovarian cysts.
Salivary gland uptake is normally minimal to low. Radiation therapy, infection, and inflammation increase FDG activity.
Thyroid gland uptake is normally diffuse and low level. Intense diffuse activity is associated with Graves disease or thyroiditis. An asymmetric focus of activity suggests possible thyroid cancer and warrants US evaluation and consideration of biopsy.
Brown Fat. A pattern of symmetric uptake in the paraspinal regions, mediastinum, neck, and supraclavicular area may be localized on the CT images as coming from fat. When a patient is cold or anxious, increased levels of catecholamines increase glycolytic activity in brown fat. This may be very difficult to differentiate from lymphadenopathy without coregistered CT images. Keeping the scan room warm and sedating anxious patients may diminish this activity.
In an attempt to semiquantitatively assess the uptake of radiotracer, the SUV was introduced to take into consideration the weight of the patient as well as the administered dose. Software to calculate SUV is available with most imaging systems. SUV is calculated by placing a region of interest over the lesion to measure tracer activity in microcuries/cubic centimeter. This value is divided by the administered dose (in microcuries) divided by the patient’s body weight (in grams).
Most malignant tumors have an SUV of 2.5 to 3.0, but this can be variable based upon the tumor type such as bronchoalveolar carcinoma where SUVs tend to be near physiologic. Physiologic activity usually has an SUV of 0.5 to 2.5 depending on the organ system. Relying on SUV has limitations.
Many factors affect the uptake of radiotracer in a given lesion, including lean body weight, state of hydration, insulin level, blood sugar level, distribution of nontarget organs and space, etc. Taking into consideration only body weight limits the accurate assessment of the accumulated activity, especially for purposes of comparison; however, it does have advantages over pure visual evaluation.
Many factors affect the uptake of radiotracer in a given lesion, including lean body weight, state of hydration, insulin level, blood sugar level, distribution of nontarget organs and space, etc. Taking into consideration only body weight limits the accurate assessment of the accumulated activity, especially for purposes of comparison; however, it does have advantages over pure visual evaluation.
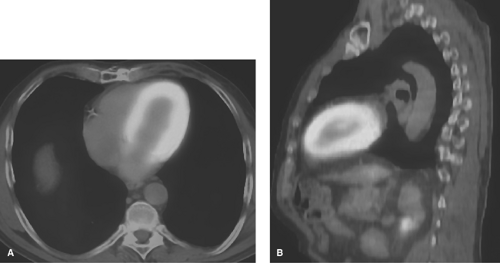 Figure 63.4. Physiologic Fluorodeoxyglucose Activity in the Heart. Fused PET-CT images in axial (A) and sagittal (B) planes demonstrate normal prominent myocardial uptake by the LV. |
Oncologic Pet Imaging
Currently PET is utilized in oncology for three major indications: initial staging, evaluation of response to treatment, and assessment for recurrence. Recent literature also cites emerging application of PET for predicting the prognosis of a few malignancies based on uptake values. In addition, primary assessment of single pulmonary nodule by PET is an acceptable next step in the evaluation of malignancy. Although there are a few hypometabolic malignancies causing false-negative PET cases, the majority of common cancers are highly metabolically active and glucose avid. In addition, there are a few nonmalignant processes with high metabolic activity, which should be recognized to avoid false-positive results. These include infectious and inflammatory conditions, as well as a few benign neoplastic processes.
Lung Cancer. Traditionally, lung cancer has been classified into small cell lung cancer (15%) and nonsmall cell lung cancer (85%). Nonsmall cell lung cancer is subdivided into the histologic subtypes adenocarcinoma (including bronchoalveolar cell carcinoma) (50%), squamous cell carcinoma (30%), and large cell carcinoma (5%). PET has been proven to be most useful with both small cell and nonsmall cell cancers, most of which are highly avid for FDG. Early detection and accurate staging have immense impact on the survival of all subtypes of lung cancer.
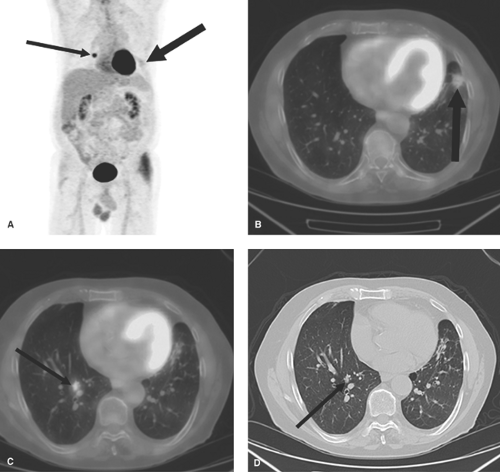
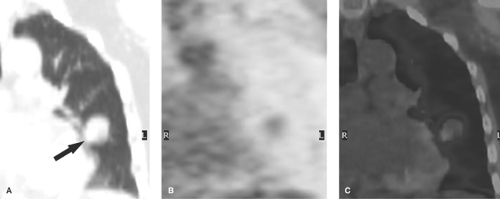
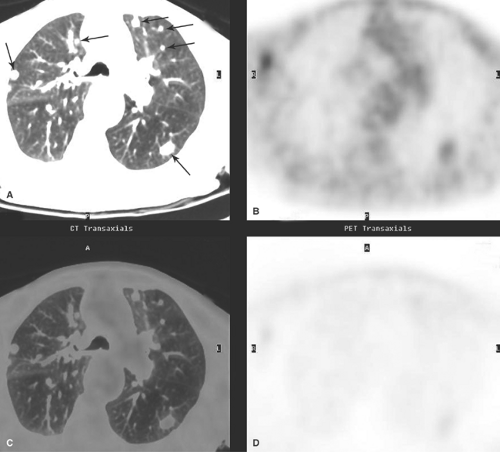
Solitary Pulmonary Nodule. FDG-PET is one of the most valuable modalities in the workup of a solitary pulmonary nodule detected by CT or radiographs. Most cancers have high metabolic activity and are hyperintense on PET (Figs. 63.8, 63.9). Most benign lesions, including non-active granulomas, other inflammatory nodules, and hamartomas, do not accumulate FDG and appear hypointense on PET imaging. PET is reported to be 97% sensitive and 78% specific for the diagnosis of malignant pulmonary nodules. PET can also be used for the assessment of multiple pulmonary lesions (Fig. 63.10) of unknown etiology, although the efficacy of this application is currently under investigation. If a solitary pulmonary nodule is a metastasis, PET can potentially detect the extrapulmonary primary cancer in the same study. Despite its limitations, SUV is commonly used to estimate the likelihood of malignancy. An SUV of 2.5 or greater is considered indicative of malignancy although active granulomas may be FDG avid. An SUV under 1.5 is suggestive of a benign nodule (bronchoalveolar carcinoma is an exception to this). SUV may be artifactually lowered by smearing artifact produced by breathing during the prolonged acquisition of the PET study over several minutes. Respiratory gating and corrective algorithms for the PET data, based on CT images, can be used to further enhance the accuracy of the SUV (cSUV = corrected SUV). With small nodules (<1.5 cm), the partial volume-averaging effect may falsely lower the SUV below 2.5, even though the nodule is malignant. False-positive results occur with tuberculosis, fungal infections, and sarcoidosis. However, most PET-positive nodules are malignant, and hypermetabolic lesions should be considered malignant until proven benign. PET-negative nodules can generally be followed rather than biopsied. The reported false-negative cases are usually hypometabolic malignancies, including bronchoalveolar carcinoma and carcinoid tumor. Analysis of CT characteristics of the nodule is crucial in making the correct diagnosis.
Staging. Lymph nodes that are normal by CT size criteria can still harbor metabolically active malignant cells, which are detectable by PET. FDG-PET is 80% to 90% sensitive and 85% to 100% specific for malignancy in mediastinal nodes and 75% sensitive and specific for malignancy in hilar nodes (Fig. 63.11). The negative predictive value of PET for mediastinal involvement is 95%, allowing surgical resection of lung cancer with a high degree of confidence. Inflammatory changes in hilar and mediastinal lymph nodes cause false-positive PET scans. PET demonstration of distant metastases in bones, brain, liver, or adrenal glands precludes surgery for cure. PET
may demonstrate sites of tumor involvement not suspected by CT in 11% of patients with nonsmall cell lung cancer. CT can overestimate the size of the pulmonary lesion because of perilesional inflammation, necrosis, and distal atelectasis. PET is useful in demonstrating the metabolically active tumor within hypometabolic areas of consolidation or atelectasis. Increased FDG activity within a pleural effusion is indicative of malignant pleural effusion, with an accuracy of 92%. Inflammatory changes postpleurodesis may also result in FDG activity indefinitely.
may demonstrate sites of tumor involvement not suspected by CT in 11% of patients with nonsmall cell lung cancer. CT can overestimate the size of the pulmonary lesion because of perilesional inflammation, necrosis, and distal atelectasis. PET is useful in demonstrating the metabolically active tumor within hypometabolic areas of consolidation or atelectasis. Increased FDG activity within a pleural effusion is indicative of malignant pleural effusion, with an accuracy of 92%. Inflammatory changes postpleurodesis may also result in FDG activity indefinitely.
Detecting Recurrence. Recurrent disease, whether locally within the thorax or as distant metastases, is common in lung cancer. PET serves as a comprehensive imaging modality in screening the whole body for all potential sites of recurrence (see Fig. 63.26). FDG-PET accurately differentiates postsurgical changes in the thorax from recurrent malignancy. Radiation pneumonitis is metabolically active in the first 6 months following radiotherapy, making detection of tumor recurrence by PET difficult (Fig. 63.12). Interpretation of FDG activity in a radiation port must be interpreted cautiously and in correlation with CT findings.
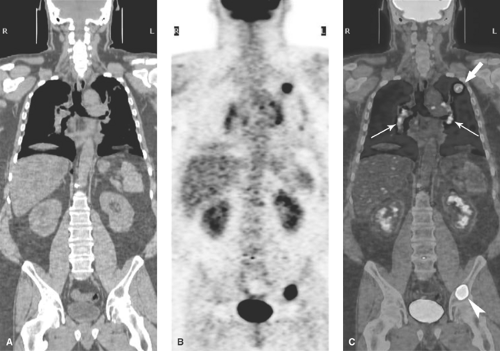
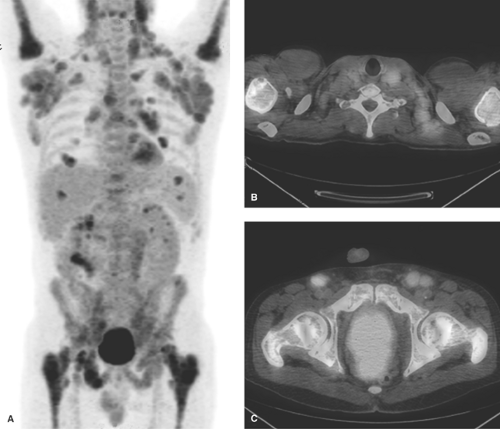
Lymphoma. Staging determines therapy in lymphoma (Fig. 63.13). Staging is based on the presence of disease above or below the diaphragm, involvement of single or multiple nodal basins, and confinement to lymph nodes or spread to extranodal tissues. Because of its ability to detect disease in nodes that are not enlarged, FDG-PET is more sensitive and more specific than CT in lymphoma staging (86% vs. 81% sensitive and 96% vs. 41% specific). FDG uptake correlates with histologic grade and the degree of the proliferative activity of the lymphomatous tissue. Some cases of malignant lymphoma are not highly metabolically active and therefore produce a false-negative result on PET. Low-grade lymphomas show limited PET activity, and mucosal-associated lymphoid tissue lymphomas are easily overlooked because of the background activity of the GI tract. False-positive PET scans occur with hypermetabolic sarcoidosis, tuberculosis, pyogenic abscesses, histoplasmosis and other fungal infections, and discitis. In practice, hypermetabolic lymph nodes are considered malignant until proven benign, usually by biopsy.
Initial Staging. PET is an excellent modality for the initial assessment of Hodgkin disease and aggressive non–Hodgkin lymphoma (NHL) but is less useful for low-grade follicular NHL. For nodal disease assessment, FDG-PET is superior to CT in the thorax and abdomen. For extranodal disease, which is present in 40% of lymphoma patients, PET is also excellent but has the following limitations. Diffuse lymphomatous involvement of the spleen is a challenge for all
imaging modalities, including PET. Diffuse splenic activity greater than that of liver activity is consistent with diffuse lymphomatous infiltration of the spleen. Focal hyperactivity in the spleen suggests focal lymphoma, whether or not a corresponding mass is shown on CT (Fig. 63.14). Assessment of bone marrow is also limited, as a variable degree of activity is always present in normal marrow spaces. However, PET can provide a map for hypermetabolic marrow foci to increase the yield of marrow biopsy. Hyperactive marrow on PET images could be caused by hyperplasia of normal marrow after chemotherapy, rather than representing lymphomatous tissue. Increased activity in the spleen usually accompanies hyperplasia of the marrow and may provide a clue to the correct diagnosis. An osteolytic bone lesion in NHL may be a cold lesion on Tc99m-MDP radionuclide bone scans. FDG-PET can demonstrate significant metabolic activity in cold osteolytic lesions characterizing them accurately as aggressive active disease.
imaging modalities, including PET. Diffuse splenic activity greater than that of liver activity is consistent with diffuse lymphomatous infiltration of the spleen. Focal hyperactivity in the spleen suggests focal lymphoma, whether or not a corresponding mass is shown on CT (Fig. 63.14). Assessment of bone marrow is also limited, as a variable degree of activity is always present in normal marrow spaces. However, PET can provide a map for hypermetabolic marrow foci to increase the yield of marrow biopsy. Hyperactive marrow on PET images could be caused by hyperplasia of normal marrow after chemotherapy, rather than representing lymphomatous tissue. Increased activity in the spleen usually accompanies hyperplasia of the marrow and may provide a clue to the correct diagnosis. An osteolytic bone lesion in NHL may be a cold lesion on Tc99m-MDP radionuclide bone scans. FDG-PET can demonstrate significant metabolic activity in cold osteolytic lesions characterizing them accurately as aggressive active disease.
Early Assessment of Treatment Response. Conventionally, the response to the treatment is evaluated by cross-sectional anatomic imaging modalities, using nodal size criteria. PET is able to detect appreciable decreases in FDG activity even before the completion of the first course of chemotherapy (Fig. 63.15). This application can save significant time and resources by early confirmation of the effectiveness or failure of applied therapy. SUV measurements before, during, and after treatment provide semiquantitative measurements of the response to therapy.
Posttherapy Residual Mass. If no residual activity is detected on PET after the completion of the course of treatment, we can conclude that the patient is in remission with favorable prognosis. Residual masses, demonstrated by CT, are common after the completion of therapy. Lack of FDG metabolic activity in these masses is evidence of the absence of viable tumor. However, residual activity needs to be interpreted with caution, as it may represent either residual hypermetabolic neoplastic tissue or active inflammation with ongoing necrosis. These cases may require biopsy or short-term repeat FDG-PET imaging to confirm the diagnosis.
Detection of Recurrence. Periodic PET scanning is reliable for the assessment of continuing remission. Comparison with initial (pretherapy) and posttherapy PET and CT scans is of utmost importance. FDG activity is highly indicative of active tumor, whereas the absence of FDG activity indicates continued remission. Sources of error in the use of PET for staging and follow-up of lymphoma include infection, drug toxicity, effects of radiation therapy and surgery, and physiologic activity. Infections are common in bone marrow-suppressed patients, especially in the respiratory and GI tracts. Active infection and inflammation show PET activity that may be
mistaken for lymphomatous involvement. Drugs, such as bleomycin, may injure the lungs, resulting in diffuse FDG lung activity. Granulocyte colony-stimulating factor therapy used to stimulate proliferation of granulocytes may cause focal marrow activity, mimicking lymphoma involvement. Inflammatory response and healing induced by radiation therapy or surgical procedures cause PET activity. False-positive FDG uptake in the thymus, associated with thymic enlargement on CT, owing to thymic rebound, commonly occurs in children undergoing treatment for lymphoma.
mistaken for lymphomatous involvement. Drugs, such as bleomycin, may injure the lungs, resulting in diffuse FDG lung activity. Granulocyte colony-stimulating factor therapy used to stimulate proliferation of granulocytes may cause focal marrow activity, mimicking lymphoma involvement. Inflammatory response and healing induced by radiation therapy or surgical procedures cause PET activity. False-positive FDG uptake in the thymus, associated with thymic enlargement on CT, owing to thymic rebound, commonly occurs in children undergoing treatment for lymphoma.
Melanoma. Early-stage melanoma (85% of patients) is curable by surgery, whereas 15% of patients have advanced local disease or metastases. Diagnosis is usually made by physical examination and biopsy. It is currently unknown whether PET can differentiate melanoma from atypical nevi or benign pigmented skin lesions. Melanoma is highly avid for FDG, but the volume of tumor in nodal metastases is small, limiting the usefulness of PET for regional staging. Acne and carbuncles show FDG hyperactivity and may mimic melanomas or skin metastases.
Sentinel lymph node mapping is safe and accurate in regional node staging of melanoma. A small amount of technetium-99m (Tc-99m)-labeled sulfur colloid is injected intradermally around the tumor. The colloid particles are cleared by the local lymphatics, and the radioactive colloid is trapped in regional lymph nodes that drain the tumor site. These nodes can be located by a gamma probe and removed at surgery. Although it is highly specific (97%), FDG-PET is relatively insensitive for these regional node metastases (as low as 17% sensitivity); thus Sentinel lymph node mapping is preferred. PET is highly useful in the demonstration of distant metastases, which occur most commonly in the lungs, liver, adrenal glands, GI tract, and bone, as well as in unusual sites such as the spleen, thyroid, gallbladder, pancreas, and skin. Whole-body PET is 92% sensitive and 90% specific in the detection of distant metastases. Limitations are small lung and brain metastases, which may not be detected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree