Chapter 15
Post-treatment changes in the liver
Ersan Altun1, Mohamed El-Azzazi1,2,3,4, and Richard C. Semelka1
1The University of North Carolina at Chapel Hill, Department of Radiology, Chapel Hill, NC, USA
2University of Dammam, Department of Radiology, Dammam, Saudi Arabia
3King Fahd Hospital of the University, Department of Radiology, Khobar, Saudi Arabia
4University of Al Azhar, Department of Radiology, Cairo, Egypt
- Malignant liver lesions may be treated by
- Surgical resection
- Liver transplantation
- Radiation therapy
- Systemic chemotherapy
- Transcatheter arterial chemoembolization
- Ablative therapies
- Surgical resection
Surgical resection
- Surgical removal with resection negative margins remains the optimal therapy for primary and secondary malignant liver tumors.
- Wedge resection, segmentectomy, and hepatectomy are the surgical resection techniques (Figures 15.1 and 15.2).
- Wedge resections and resection margins may show low attenuation on precontrast CT images and mildly high signal on T2-weighted and low signal intensity on T1-weighted precontrast MR sequences. A thin rim of enhancement may be seen along the resection margins in the hepatic arterial dominant phase, which fades to isointensity in later phases. In successful complete resection, by 6 months postprocedure negligible enhancement is seen in these resection areas on postcontrast images.
- Resection margin enhancement reflects leaky capillaries (early on), edema, and granulation tissue (>1 month) in the liver parenchyma. These changes are most prominent in the first 3 months after surgery and gradually decrease over the following 6 months.
- Hyperplasia/hypertrophy of the remaining liver may be appreciated as early as 3 months after surgery. Within 1 year, general enlargement of the remaining liver occurs. After right hepatectomy, hypertrophy of the medial segment may create the appearance of a pseudo right lobe.
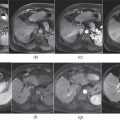
- Tumor recurrence has a similar appearance to untreated malignant lesions and may arise along the resection margin. The recurrence appears as a thick rim of mildly high T2 signal/low T1 signal which shows prominent enhancement, or as a nodular lesion with mildly high T2 signal/low T1 signal that shows prominent enhancement (Figure 15.3).
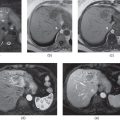
- Bilomas, hematomas, and fluid collections may be seen along the resection margins (Figure 15.4).
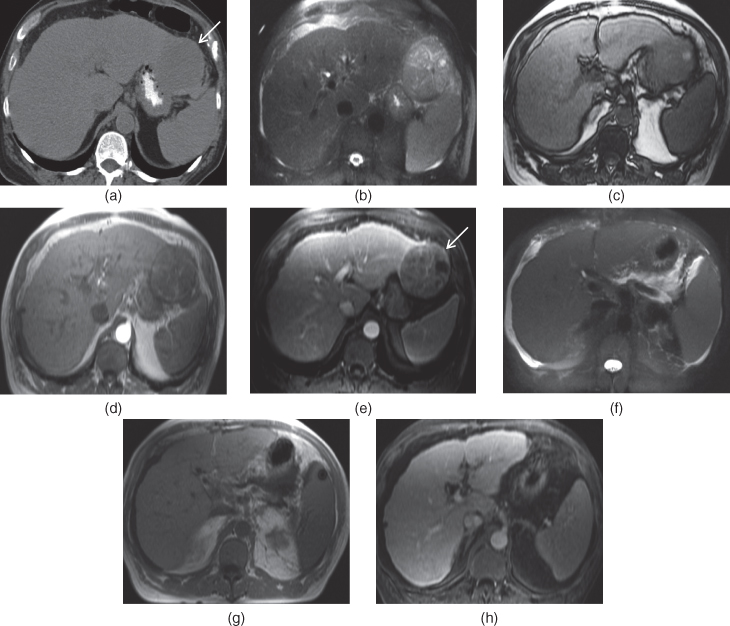
Figure 15.1 Transverse precontrast CT image (a), transverse T2-weighted fat-suppressed SS-ETSE (b), T1-weighted out-of-phase 2D-GE (c), T1-weighted postgadolinium arterial phase 2D-GE (d), fat-suppressed hepatic venous phase 3D-GE (e) images show a large heterogeneously enhancing exophytic HCC (arrows) arising from the left lobe of the liver in a patient with cirrhotic liver. The mass is surgically resected and no residual lesion is seen on postoperative MR images (f–h).
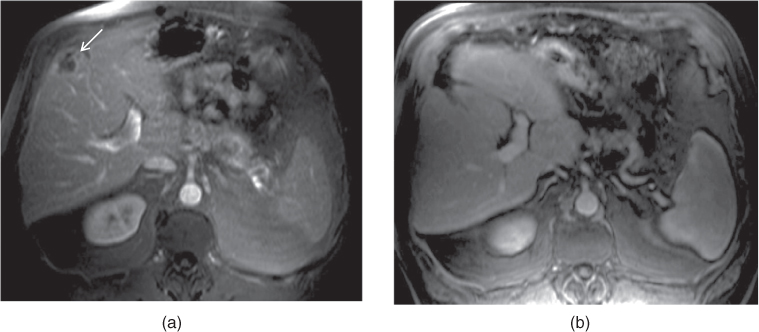
Figure 15.2 Transverse fat-suppressed T1-weighted postgadolinium 3D-GE images (a, b) show the successful interval resection of a colon carcinoma metastasis (arrow, a) located at the periphery of the liver. The lesion is not seen on the postoperative image (b).
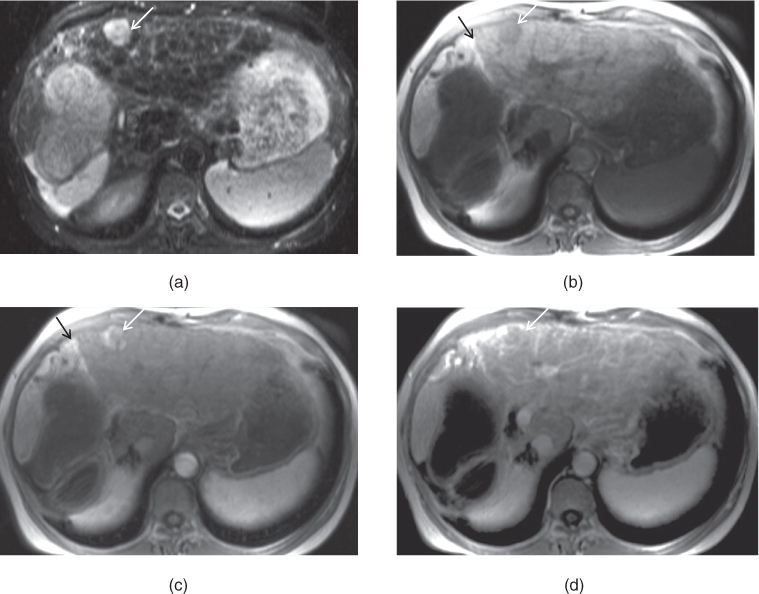
Figure 15.3 Transverse T2-weighted STIR (a), T1-weighted in-phase 2D-GE (b), T1-weighted postgadolinium hepatic arterial dominant phase 2D-GE (c), hepatic venous phase 3D-GE (d) images demonstrate the development of a recurrent enhancing HCC (white arrows, a–d) in a patient with right hepatectomy. Note that the liver is cirrhotic and the recurrent HCC is close to the resection margin (black arrows; b, c).
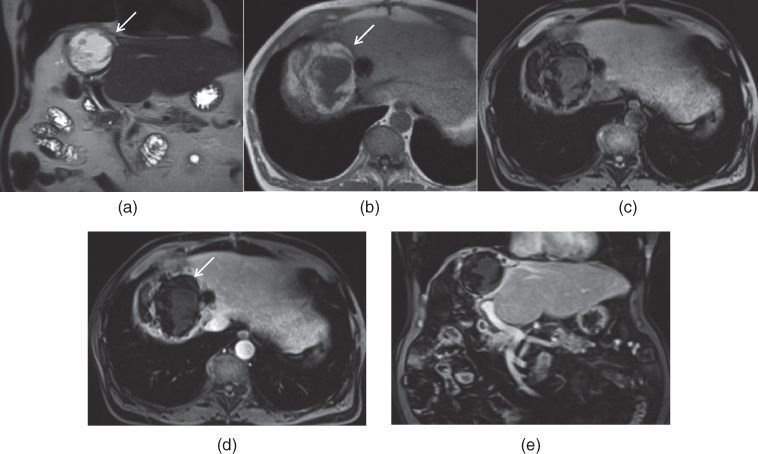
Figure 15.4 Coronal T2-weighted SS-ETSE (a), transverse T1-weighted 2D-GE (b), T1-weighted fat-suppressed 3D-GE (c), T1-weighted postgadolinium fat-suppressed hepatic venous phase (d) and coronal T1-weighted postgadolinium fat-suppressed hepatic venous phase (e) 3D-GE images show a large fluid collection (arrows) in a patient with right hepatectomy. A complex fluid collection with high T2 signal is seen along the resection margin, which represents a biloma. The fluid collection has irregular fat-containing borders, which represent the omentum. Mild stable wall enhancement is seen along the walls of the collection, which represents mild inflammation. The presence of significant wall enhancement, which is not seen in this case, may be a sign of infection and abscess. No residual disease is seen in the liver parenchyma. An oval susceptibility artifact secondary to surgical clips at the dome of the liver is seen.
Hepatic transplantation
- Donors and recipients may undergo a liver MR protocol with MRCP and MRA or CT with CTA for the evaluation of IVC, hepatic veins, portal vein, hepatic artery, and common bile duct.
- Recipients may receive living-related partial livers (lateral segment for small pediatric patients, right lobe for adult-to-adult recipients) or cadaveric whole or partial livers.
- In living-related hemiliver transplantation, the usual surgical procedure involves resecting the right lobe for donation and retaining the left lobe in the donor.
- In the donor liver, the resection plane is approximately 1 cm into the right lobe from the middle hepatic vein and extends inferiorly to the bifurcation between the right and left portal veins, so that the donor retains the middle hepatic vein.
- Living related transplants have decreased in frequency because of the risks to the donor due to the failure of the remaining liver tissue.
- The presence of malignant disease in the recipient individual’s native liver is an important determination for eligibility for transplant. Currently, the most common indication for transplantation is the presence of limited HCC disease as determined by UNOS (The United Network for Organ Sharing)/OPTN (The Organ Procurement and Transplantation Network) criteria. The patients having a single HCC < 5 cm or not more than three HCCs, with none > 3 cm, in the absence of vascular invasion and metastases, represent the patients having limited disease and are candidates for liver transplantation.
- Complications of liver transplant surgery include fluid collections including biloma, seroma, or abscess (Figure 15.5), hematoma, vascular complications such as hepatic artery, portal vein, hepatic vein thrombosis and anastomotic strictures (Figure 15.6); biliary complications such as infection (Figure 15.7), and biliary anastomotic strictures (Figure 15.8).
- Bile leaks may develop at the anastomosis for technical reasons or may be secondary to bile duct necrosis in those patients with hepatic artery thrombosis.
- Strictures of the biliary tree are often a late complication of liver transplantation and usually occur at the anastomosis secondary to scar formation.
- Bile duct dilatation may be seen due to rejection. The differential diagnosis of rejection includes biliary obstruction, cholangitis, ischemic injury, viral infection, and drug toxicity.
- Periportal signal showing low signal intensity on T1-weighted images and high signal intensity on T2-weighted images may also be seen after transplantation and the differential includes lymphatic leak (due to failure of development of lymphatic channel continuity), lymphocytic infiltration due to rejection, and posttransplant lymphoproliferative disease (PTLD).
- Living related transplants have decreased in frequency because of the risks to the donor due to the failure of the remaining liver tissue.
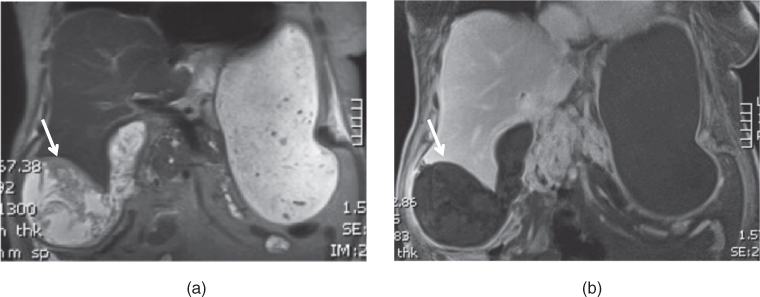
Figure 15.5 Coronal T2-weighted SS-ETSE, T1-weighted fat-suppressed hepatic venous phase 3D-GE images show a subhepatic complex fluid collection (arrow; a, b) in a patient following liver transplantation. The collection shows moderate wall enhancement, which is suggestive of infection – abscess.
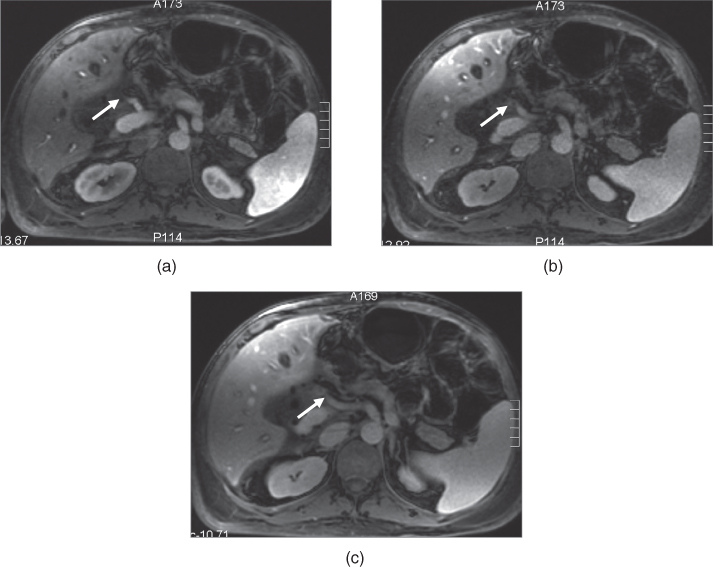
Figure 15.6 Transverse T1-weighted fat-suppressed postgadolinium hepatic arterial dominant phase (a), hepatic venous phase (b, c) 3D-GE images show significant hepatic arterial stenosis (arrows) in a patient with liver transplantation. The common hepatic artery shows significant narrowing at its midportion and its distal part cannot be visualized. Note the presence of periportal edema in the liver around the portal tracts.
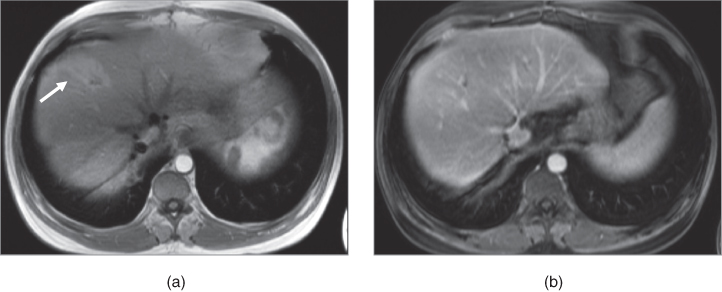
Figure 15.7 Transverse postgadolinium T1-weighted hepatic arterial dominant phase 2D-GE (a), fat-suppressed hepatic venous phase 3D-GE (b) images show mild focal segmental bile duct dilatation with transient early increased enhancement (arrow) at segment VIII in a patient with liver transplantation. These findings may develop secondary to mild ascending cholangitis and clinical correlation is required as focal bile duct dilatation with mild inflammation (without infection) secondary to postsurgical changes/bile duct ischemia may also be associated with early transient increased enhancement. The presence of bile duct wall enhancement in the later phases is suggestive of more prominent inflammation/infection.
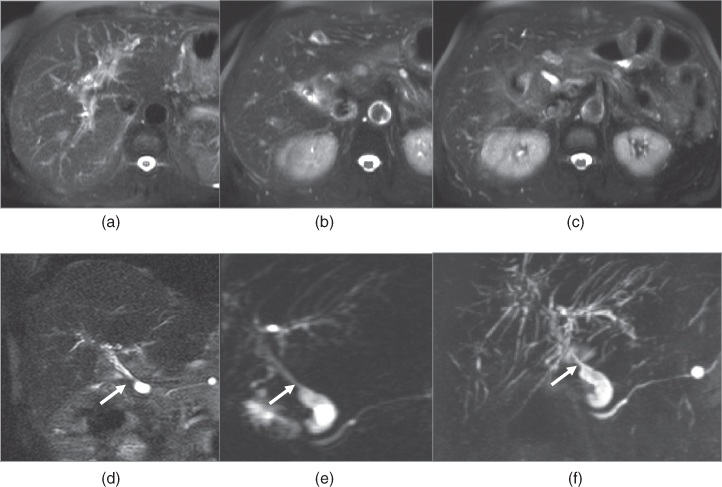
Figure 15.8 Transverse T2-weighted fat-suppressed SS-ETSE (a–c), coronal T2-weighted fat-suppressed SS-ETSE, single shot coronal thick slab heavily T2-weighted MRCP and reconstructed 3D MIP image of thin slab heavily T2-weighted MRCP images show prominent ischemic changes of the intrahepatic biliary ducts. The intrahepatic biliary ducts demonstrate multiple diffuse strictures and dilatations on the 3D reconstructed image (f). Mild edema is seen along the central intrahepatic bile ducts. The common bile duct also appears diffusely thin, which again may develop secondary to ischemic changes and a moderate stricture is also seen at the anastomosis line (arrows; d–f). Note that a small cyst is also seen at the pancreatic tail.
Radiation therapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree