The aim of imaging in the follow-up of asymptomatic patients treated for sinonasal neoplasms is to detect submucosal relapsing lesions. The challenge is to discriminate recurrent tissue within the changes resulting from unpredictable healing of tissue after surgery and radiotherapy. Scar, inflammation, and recurrence can be better separated with a multisequence MR imaging approach. The choice of the field of view should take into account the risk of in-field intracranial recurrences, craniofacial bone metastases, and perineural spread. Fluorodeoxyglucose-PET has a role in assessing distant metastasis. Its usefulness in local and regional surveillance has yet to be established.
Key points
- •
A proper imaging protocol and correct interpretation of post-treatment imaging findings rely on knowledge of the most frequently used surgical and radiation therapy techniques and principles of oncological resection.
- •
MR is superior to CT in detecting recurrences because of a higher capability in discriminating tissues and post-treatment changes, related to a multisequence analysis. Most acute complications are the domain of CT.
- •
In-field intracranial recurrences and craniofacial bone metastases are possible when the primary tumor invades the dura and with aggressive histologies. Perineural spread along cranial nerves and branches has to be carefully scrutinized, particularly in the case of adenoid cystic carcinoma and squamous cell carcinoma.
Introduction
Sinonasal neoplasms are characterized by great histologic heterogeneity, reflecting the number of different tissues in this area. As a result, a large variety of benign and malignant neoplasms may arise from the mucosa lining the sinonasal cavities or from submucosal structures. Numerous types of treatment have been developed to address different oncological conditions. For example, benign neoplasms are treated solely by surgical resection, whereas most malignant neoplasms require multimodal therapy.
Diverse surgical techniques have been devised to adequately treat neoplasms with a great variability in biological aggressiveness. The invasiveness of surgical approaches are at 2 ends of the spectrum: open surgical techniques and endoscopic surgery. A minimally invasive surgical approach, namely endoscopic surgery, was originally adopted only for inflammatory conditions. In the last 2 decades it has been used initially for benign tumors, then as a complement to, and more recently as an alternative to open surgery in selected malignant neoplasms.
Parallel progress in radiation therapy techniques has been attained over the last 2 decades, mostly with the introduction of intensity-modulated radiation therapy, volumetric modulated arc therapy, and advances in particle radiation therapy.
It follows that tailoring specific post-therapy imaging protocols is crucial to overcome the combination of different histologies with characteristic patterns of spread or relapse and different treatment techniques. In addition, post-treatment imaging is required in distinct clinical settings, from the immediate postsurgical intracranial complications to follow-up after chemotherapy and radiotherapy (RT).
A practical imaging strategy for dealing with such challenges is to resolve the diverse clinical scenarios into a given number of key factors.
The first factor deals with the expected imaging changes: that is, knowledge of which imaging findings should normally be present after surgery for benign or malignant neoplasm, or after RT. The second factor entails knowledge of the specific model of growth of those benign and malignant neoplasms that may result in characteristic patterns of recurrence, such as perineural spread for adenoid cystic carcinoma. The third factor involves detailed information about the type of surgical resection/reconstruction, relevant intraoperative findings, and pathologic data that could point to areas at higher risk for recurrence.
This information is useful not only to select the proper imaging protocol but also to increase the accuracy in interpreting imaging findings. The availability of previous studies and careful matching with current imaging and clinical findings is certainly crucial in minimizing the chance of missing relapsing neoplasms.
Imaging techniques
A comprehensive description of computed tomography (CT) and MR imaging techniques is beyond the purpose of this article. However, some critical technical aspects in post-treatment imaging are discussed here. CT is usually performed to exclude acute intracranial complications such as tension pneumocephalus, hemorrhage, skull base defects, abscess, or orbital complications. In cases of orbital or intracranial abscesses, contrast agent administration is indicated. Multiplanar reconstructions (MPR) on coronal and sagittal planes with both bone and soft tissue windows should be part of the imaging protocol.
During follow-up, MR imaging is superior to CT in detecting recurrent/persistent disease, depicting its spatial extent, and identifying complications such as cerebrospinal fluid (CSF) leak, neuritis, and white-matter necrosis.
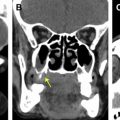
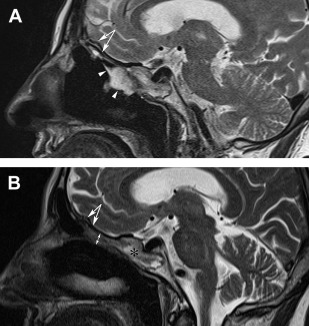
T2 sequences provide the best signal discrimination ( Fig. 1 ). In our protocols, they are the first sequences acquired on at least the axial and coronal planes. They represent conceptual shelves for inserting information provided by subsequent sequences. T1 sequences are used to assess the extent of medullary bone abnormalities and as a baseline for contrast-enhanced sequences. For example, this combination helps to identify collections of dehydrated entrapped fluid (hyperintense on T1) that could otherwise mimic enhancement in postcontrast images. Both T2 and T1 sequences should be acquired with thin slices (3 mm or less) and high in-plane resolution (512 × 256 or more). Time-sparing (parallel imaging) and motion-reduction (PROPELLER/BLADE) techniques are usually not needed, but they may be useful in uncooperative patients. In our experience, fat-saturated T2 sequences are not useful and they should not be used in lieu of standard T2 sequences. In fat-suppressed T2 sequences, most of the anatomic information is lost and the range of signals is narrowed and altered. In addition, inefficient fat suppression may simulate focal abnormalities.
Diffusion-weighted imaging (DWI) has become one of the most promising and appealing techniques in recent years. The main strength of DWI in the field of oncology is its capability of discriminating tumor from inflammation. For this reason, DWI seems to fit the purpose of post-treatment imaging; that is, to properly separate expected post-treatment inflammatory changes from recurrences. A high signal in high b value (b1000) images and a low signal on apparent diffusion coefficient (ADC) maps suggests recurrence, whereas a high ADC indicates inflammation. However, the technique is hampered by important limitations: DWI is affected by susceptibility artifacts, especially in areas rich in bone-fat-air interfaces such as the sinonasal tract; a high b1000 signal in the brain may mask recurrences in the skull base; metallic clips may hinder proper fat saturation in adjacent areas, especially in adipose flaps, resulting in misleading interpretations. In addition, the simple rule high b1000 + low ADC = tumor; high ADC = inflammation is not valid for all histologies (eg, in intestinal-type adenocarcinoma, high mucinous content reduces the b1000 signal and raises the ADC value).
Enhanced three-dimensional fat-saturated gradient-echo T1 sequences (VIBE) are able to depict areas of enhancement with high isotropic resolution. Fat saturation increases the consistency of enhancement within fat-containing tissues (eg, the medullary bone). Furthermore, high spatial resolution and multiplanar reconstructions provide optimal assessment of both perineural spread and the spatial relationship of neoplastic tissue with complex anatomic structures. Our advice is to acquire VIBE sequences early after Gd administration; intense and diffuse enhancement of inflammatory tissues occurs in delayed phases (ie, 3–4 minutes after contrast administration).
Postcontrast three-dimensional constructive interference in steady state (CISS) sequences may be used as additional sequences when the relationship between an enhancing neoplasm and the dura and/or cranial nerves needs to be precisely mapped ( Fig. 2 ).
Dynamic contrast-enhanced (DCE) MR imaging has been proposed by some investigators as a useful tool in inflammation/tumor discrimination. However, in our experience, integration of the aforementioned sequences is sufficient to optimally image treated patients within a reasonable time.
Some recent studies have shown diagnostic usefulness of 18 F-fluorodeoxyglucose (FDG)-PET/CT for restaging patients treated for sinonasal malignant neoplasms. An important advantage of 18 F-FDG-PET/CT is that a whole-body scan allows for the detection of distant metastases and unexpected secondary cancers. As in CT and MR imaging, postsurgical and post-RT crusting and inflammation may cause mild to even high hypermetabolic activity in the absence of relapsing disease. Despite this, metabolic activity is useful to distinguish scar tissue from recurrences. A negative PET/CT study seems to be more predictive of the absence of disease as seen in the consistently high negative predictive values among all sites.
Expected imaging changes after surgery
After surgery for sinonasal neoplasms, post-treatment follow-up with imaging is mainly based on MR imaging with the aim of detecting residual/recurrent lesions, providing detailed mapping of known recurrences, and recognizing possible complications (ie, mucocele).
After surgery, most intranasal structures are usually resected. This fact facilitates endoscopic examination of the healed mucosal surfaces, although the development of adhesions or a peculiar anatomy may hamper an adequate survey of the frontal or sphenoid sinuses. Therefore, the specific domain of post-treatment imaging studies is the assessment of structures unreachable by endoscopy, namely intracranial and intraorbital structures, or to scrutinize other potential submucosal sites of recurrence.
Crucial to the understanding of postsurgical changes is that the oncologic principles for endoscopic resection of benign neoplasms differ from those required for malignant neoplasms. For example, for a benign neoplasm abutting the adjacent bony surface, subperiosteal dissection with drilling of the bone is generally sufficient to achieve oncologically adequate removal. On the contrary, as the aim of resection of malignant neoplasms is to achieve negative margins, not only the area of attachment but also eroded bone structures or those in contact with an aggressive malignant neoplasm have to be removed.
Generally, the removal of central structures of the naso-ethmoid complex does not require any reconstruction. When noncentral structures, such as sections of the skull base shell are resected along with variable sections of the dura mater, large defects in bones and meninges are created. There is the need to restore the seal between the intracranial compartment and the sinonasal cavities to avoid complications such as CSF leak, meningitis, and pneumocephalus ( Table 1 ). The techniques developed to close these defects differ from the techniques used for endoscopic CSF leak repair. Not only are the defects to be sealed larger but also the duraplasty could be included in the field of RT. Numerous nonvascularized and vascularized reconstructive techniques have been introduced; the choice is dictated by the site of the defect and the intraoperative CSF flow.
| Surgical Approach | Medial Wall of the Orbit | Anterior Skull Base | Skull Base Reconstruction | Orbital Content | Orbital Reconstruction |
|---|---|---|---|---|---|
| Endoscopic resection | Intact (lamina papyracea may be removed) | Intact | None | Intact | None |
| Endoscopic resection with transnasal craniectomy | Intact (lamina papyracea may be removed) | Removed (on 1 or both sides) | Autologous material (iliotibial tract of fascia lata) alone or in combination with pedicled flaps (nasoseptal flap, pericranium) | Intact | None |
| Cranio-endoscopic resection (endoscopic and subfrontal approach) | Intact (lamina papyracea may be removed) | Removed | Autologous material (iliotibial tract of fascia lata) or dural regeneration matrix in combination with pericranium | Intact | None |
| Craniofacial resection (transfacial and subfrontal approach) | Removed | Removed | Autologous material (iliotibial tract of fascia lata) or dural regeneration matrix in combination with pericranium | Removed when soft tissues are involved (orbit clearance) | Required when orbital clearance is performed Free flap (rectus abdominis, anterolateral thigh) with or without epithesis |
In most sinonasal neoplasms, the defect is located at the anterior skull base floor where the CSF flow is low. A triple layer of the iliotibial tract of fascia lata, that is, a free tissue graft, is among the most successful repair solutions. A pedicled tissue (nasoseptal flap, pericranium flap) may also be used to reinforce the duraplasty and offer an adequately vascularized barrier.
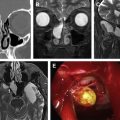
The expected imaging findings of a normal duraplasty are characterized by a multiple-layer sandwich of signals replacing the anterior skull base floor. On MR imaging, the duraplasty appears as a quite regular broad plaque 3 to 5 mm thick. When a triple layer of iliotibial tract is used, the inner layer is placed between the dura and the brain (intracranial intradural). Its size is cut to overlap the dural defect. The second and third layers are placed, respectively, between the dura and the bone (intracranial extradural) and on the intranasal surface of the bone (extracranial).
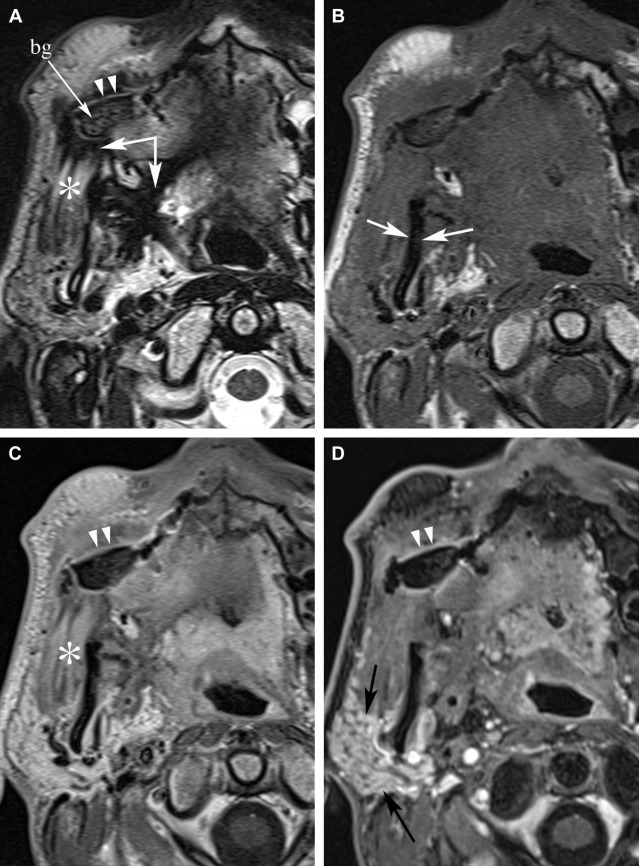
On sagittal T2 sequences, triple layer duraplasty has a variable inner signal initially but a continuous and regular intracranial surface ( Fig. 3 ). Changes in thickness and signal are observed as the graft gradually integrates. In a few months, the thickness is reduced by about 50%. Over time, the 2 nonenhancing underlay layers are progressively surrounded by 2 enhancing layers located on the intracranial and nasal sides, respectively. On the nasal side, the enhancement is a result of various phases of tissue reorganization along the neonasal cavity roof. There, the overlay layer undergoes progressive necrosis. Therefore, it is progressively replaced by in-growth of the adjacent nasal mucosa. Mucosal edema, thin and smooth polypoid changes, hyperplastic scar, or granulation tissue may account for a very variable enhancement. The enhancement present at the intracranial side of the duraplasty is probably the result of increased vascularization of the integrating fascial graft. The fat grafts, which may be added within duraplasty to fill dead spaces and properly dress the defect, progressively reabsorbs and nearly disappears at 1 year ( Fig. 4 ).
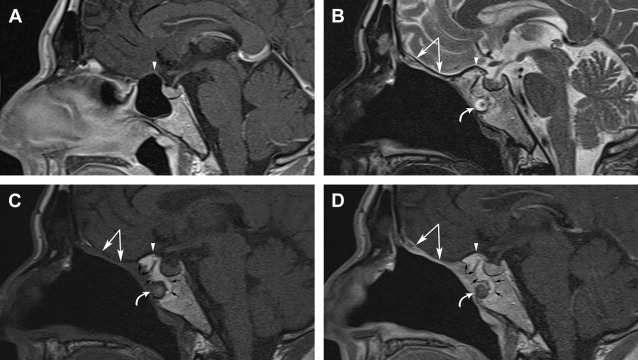
Two main points are better analyzed if the MR protocol includes sagittal and coronal T2 and corresponding enhanced T1 images. The first is that the fascia lata duraplasty can be disassembled into its singular tissue components, which show different signal intensities. This makes it easier to differentiate the duraplasty from recurrent disease. The second advantage is that the sagittal planes help to analyze the area behind the posterior wall of the frontal sinus, which is difficult to evaluate on coronal planes, because of bending. An effective solution is the use of high-resolution three-dimensional gradient-echo T1 sequences. The acquired volume can be reconstructed in several planes, thereby helping to scrutinize the whole duraplasty complex.
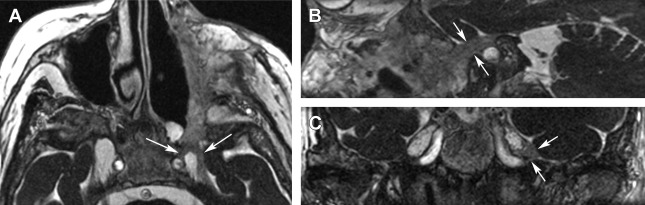
The nasoseptal flap is a mucoperiosteal-mucoperichondrial flap harvested from the nasal septum with the vascular pedicle arising from the nasoseptal branch of the sphenopalatine artery. Because of the posterior location of the artery, the flap is more frequently used to close defects in the sphenoid, nasopharyngeal, and clival regions. The nasoseptal flap is less frequently used for anterior skull base reconstruction because the defect may be large or the rotation angle of the pedicle unfavorable. Moreover, this mucoperiosteal flap cannot be used in the presence of malignancies involving the nasal septum. When the flap covers defects of the sphenoid sinus posterior wall and roof, it usually assumes a C-shaped configuration. On MR imaging, the flap appears as a T2 isointense thick tissue layer, showing full-thickness enhancement, different from the thin peripheral enhancement of the adjacent T2 hyperintense mucosa.
A second noncentral bony structure that can be removed by both endoscopic and open surgery is the lateral wall of the nasal cavity, comprising the medial wall of the orbit and the maxillary sinus. Reconstruction of the orbital medial wall is not generally necessary. That is, the orbital content is well separated from the nasal cavity by 2 protecting layers: the thick orbital periostium adherent to the bony wall and the thin fascial layer (periorbital fascia) surrounding the periocular fat.
No reconstruction is needed after resection of the medial portion of the orbital floor or the medial maxillary sinus wall with open or endoscopic medial maxillectomy ( Table 2 ). Orbit floor reconstruction, required whenever more than half of the floor is removed, may be performed by different techniques, with either autologous (ie, fascia lata, coronoid process) and/or synthetic material (titanium mesh).
| Surgical Approach | Alveolar Process – Hard Palate | Palate Reconstruction | Medial Maxillary Sinus Wall | Ethmoid and Other Maxillary Sinus Walls | Orbital Floor | Orbital Content and Reconstruction | PPF Content |
|---|---|---|---|---|---|---|---|
| Inferior maxillectomy | Removed | Prosthetic obturator; Bichat fat tissue; free flap (forearm) | Intact | Intact | Intact | Intact; no reconstruction | Intact |
| Endoscopic medial maxillectomy | Intact | None | Removed | Ethmoidectomy is commonly required; in general, the other walls of the maxillary sinus are preserved | Intact | Intact; no reconstruction | Intact |
| Subtotal maxillectomy | Removed | Free flap (iliac crest, scapula), or Pedicled flap (temporalis muscle) | Removed | Removed | Intact or partial removal (medial portion) | Intact; no reconstruction | Removed |
| Radical maxillectomy with or without orbit clearance | Removed | Free flap (iliac crest, scapula, rectus abdominis) | Removed | Removed | Removed (+/− orbit content) | Orbital floor reconstruction by autologous (fascia lata, coronoid process) or synthetic (titanium mesh) material Orbital content reconstruction by free flap (scapula, iliac crest, rectus abdominis) with or without epithesis | Removed |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree