In order for a radiologist to create reports that are meaningful to facial reconstructive surgeons, an understanding of the principles that guide surgical management and the hardware employed is imperative. This article is intended to promote efficient and salient reporting by illustrating surgical approaches and rationale. Hardware selection can be inferred and a defined set of potential complications anticipated when assessing the adequacy of surgical reconstruction on postoperative computed tomography for midface, internal orbital, and mandible fractures.
Key points
- •
Nasofrontal duct obstruction leads to suppurative complications, including mucopyocele development, osteomyelitis, and plate infection, which ultimately may result in intracranial and/or intraorbital spread. Patency is assessed best on sagittal images.
- •
Patients who have undergone obliteration or cranialization require periodic imaging surveillance to screen for developing mucopyocele.
- •
Small changes in the axis of rotation about the ZSS should be described on postoperative imaging. A small degree of rotation can lead to large changes in orbital volume and result in enophthalmos.
- •
Orbital floor implants should bridge the entire fracture defect. Any space that persists between fracture ledges may lead to postoperative entrapment and should be described objectively.
- •
Nonunion frequently accompanies osteomyelitis. In the mandible, this results from a combination of micromotion and the spread of infection from disrupted gingiva between incompletely mobilized tooth-bearing fragment surfaces.
Introduction
A recent analysis found that in 2017, more than 7.5 million new cases of facial fractures were diagnosed worldwide. Fractures, such as isolated nasal pyramidal disruptions, small adult orbital floor blowouts, mildly displaced or angulated mandibular condyle fractures, and nondisplaced midface fractures, can be mechanically stable, have no cosmetically noticeable result, or have no long-term adverse effect on facial function and can be managed nonoperatively. Others may require open repair with titanium hardware to optimally restore premorbid function and aesthetics. Postoperative computed tomography (CT) scans commonly are performed and are useful in establishing a postoperative baseline and identifying complications that may require reoperation or revision. In order for a radiologist to create reports that are meaningful to facial reconstructive surgeons, an understanding of the principles that guide surgical management and the hardware employed is imperative. This article is intended to promote efficient and salient reporting by illustrating surgeons’ rationale for their approach. Hardware selection can be inferred and a defined set of potential complications anticipated when assessing the adequacy of surgical reconstruction on postoperative CT for midface, internal orbital, and mandible fractures.
Naso-orbito-ethmoidal fractures
Surgically Relevant Anatomic Considerations
Naso-orbito-ethmoidal (NOE) fractures are characterized by a single or comminuted central fragment resulting from fractures along at least 4 of the following 5 cardinal tracts: the lateral nose and piriform aperture, the nasomaxillary buttress (NMB), the inferior orbital rim and floor, the medial orbital wall, and the frontomaxillary suture , ( Fig. 1 ).

The central fragment serves as the insertion site of the anterior and posterior limbs of the medial canthal tendon (MCT), a support structure arising from the confluence of the upper and lower tarsal plates of the eyelids and orbicularis oculi. , Inadequate stabilization of the MCT can result in telecanthus (blunting of the medial palpebral fissure), hypertelorism (widening of the interpupillary and intercanthal distances), and enophthalmos. The MCT may be functionally or truly avulsed secondary to lateral displacement of the central fragment or comminution at the MCT insertion sites on the lacrimal crest.
Instability of the MCT (confirmed clinically through the application of pressure to the lower eyelid) largely determines the management. , Other considerations include the postreduction patency of the nasofrontal duct (NFD) and nasolacrimal duct (NLD), postreduction bone loss, posterior frontal sinus wall displacement, and depression of the frontal sinus wall—the last is important from a cosmetic standpoint. ,
Surgical Goals and Approach
Surgical management goals of NOE fractures include restoring preinjury canthal position, globe and anterior sinus wall position, nasal projection, and mucociliary clearance.
The method of fixation is based on an initial assessment of Markowitz-Manson grade at CT and evaluation of the internal orbit. Stepwise small plate fixation is applied through cosmetically favorable incisions until the MCT is immobilized intraoperatively. Internal orbital disruptions are discussed later.
A fracture resulting in a single central fragment (Markowitz-Manson grade I injury) may be stable intraoperatively, requiring no fixation, such as with greenstick or hinged fractures about a single intact cardinal line. A single plate can stabilize a mobile noncomminuted central fragment, which indirectly stabilizes an intact MCT. Using cosmetically favored incisions, a low-profile miniplate may be placed along the NMB or inferior orbital rim through the gingivobuccal sulcus or subconjunctival lower lid incisions, respectively ( Fig. 2 ). Subconjunctival incisions can be complicated by lid lag or entropion; thus, an NMB plate may be preferred for single-plate fixation. With persistent mobility on palpation, the fragment is plated at both locations, a technique often used with slightly comminuted grade II injuries. Plating across the frontomaxillary suture may be required if the fracture through the central fragment results in the creation of an upper and lower fragment. Nasofrontal suture plating is used to restore anterior nasal projection.

Severely comminuted high-energy grade III injuries result in a true or functional MCT avulsion, requiring transnasal canthopexy ( Fig. 3 ). The reconstructive surgeon attaches a wire to the MCT and passes it through an intravenous cannula inserted via a posterior transnasal drillhole, typically made above and behind the posterior crest. The wire then is secured to a plate, screw, or mesh along the contralateral frontal bar. Medial canthopexy is associated with a high failure rate, resulting in late telecanthus and globe malposition. Overtightening is performed in anticipation of expected lateral drift over time. , ,

If the nasal support is inadequate due to severe collapse or comminution of the nasal bone-cartilage framework, a dorsal nasal strut graft may be required. This often is fashioned out of the outer table of the calvarium and affixed to the glabella to restore anteroposterior nasal projection and reduce telecanthus. ,
Severely comminuted fractures requiring canthopexy, reconstruction of the nasal pyramid, or repair of other subunits as part of a panfacial fracture pattern typically necessitate a coronal approach, which provides wider surgical access. In this approach, the facial soft tissues are reflected below the frontal bar following a cosmetically favorable behind-the-hairline incision. , The clinical rationale for the range of postoperative imaging findings after NOE fractures is summarized in Table 1 .
| Postoperative Imaging Finding: Naso-orbito-ethmoidal Fractures | Clinical Rationale |
|---|---|
| Single-plate and screw fixation | Grade I fracture, unstable |
| Plate and screw fixation along the frontomaxillary suture and NMB | Unstable MCT insertion, with bone intact at the insertion site (grade II fracture) |
| Medial canthopexy |
|
| Dorsal nasal strut graft | Severe collapse of the nasal bone-cartilage framework |
| Obliteration |
|
| Cranialization |
|
| Frontal sinus mesh | Anterior wall fracture with bone loss from the outer table of the frontal sinus |
Postoperative Assessment of Complications
Disruption and stenosis of the NLD and NFD, frontoethmoidal recess, and posterior walls of the frontal sinuses can lead to functional and septic complications. NFD patency is assessed intraoperatively by observing the passage of methylene blue dye from the frontal sinuses to the nares or pharynx, although passage may be obstructed due to mucosal swelling and nasal secretions.
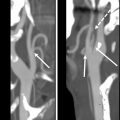
Postoperative CT assessment of the NFD is vital because obstruction eventually leads to development of mucopyocele with expansile bony remodeling, erosion, osteomyelitis, or plate infection. Orbital compartment syndrome or cellulitis may result from orbital spread, whereas intracranial extension results in meningitis, empyema, and brain abscess. Postreduction NFD continuity is assessed best on sagittal imaging ( Fig. 4 ). Discontinuity also is strongly suggested by posterior intrusion of the nasal dorsum and collapse of the anterior and middle ethmoid air cells on axial images. In ambiguous cases, serial CT over the first few weeks can be performed to assess for progressive aeration or filling of the frontal sinuses. ,

Elevated risk of septic complications corresponds with frontal sinus posterior wall defect size on postoperative imaging following reduction. In obliteration, the intracranial cavity is effectively separated from the external environment by filling the frontal sinus with free fat and plugging of the NFD with bone chips, fascia, and fibrin glue , (see Fig. 4 ). A defect less than 25% of the posterior wall surface area on postoperative CT is believed to have a lower risk of complications, and obliteration may be performed in lieu of more aggressive management with cranialization. , In such cases, associated dural defects are repaired or allowed to heal through fibrosis. If defects from bone loss and displacement are large and comminuted, it becomes difficult to ensure all microscopic mucosal rests are removed, and cranialization is favored. This involves removal of the posterior wall and placement of a pericranial flap after frontal craniotomy , ( Fig. 5 ). Because obliteration and cranialization involve mucoperiosteal stripping, even with meticulous removal, any remaining rests of mucosa during this process can serve as nidi for future mucopyocele. , , Therefore, a relatively conservative management approach frequently is employed. Patients who have undergone obliteration and cranialization require some form of surveillance, such as yearly CT, to screen for developing mucopyocele. Over time, the brain gradually expands until the frontal lobes come to rest against the anterior table after cranialization.

Cosmetic management of the anterior frontal sinus wall
Depressed (and frequently comminuted) fractures of the anterior frontal sinus wall are elevated and plated for cosmetic reasons. These fractures commonly are reduced and fixed successfully with miniplates and 3-dimensional (3-D) matrix plates during surgical simplification , (see Fig. 5 ). Mesh is used in cases of severe bone loss either directly from injury, following gradual bone resorption after frontal craniotomy and cranioplasty or osteomyelitis. Repair of panfacial fractures often is staged using a top-down or bottom-up approach, using either the frontal bar (glabella and superior orbital rims) or mandible and occlusion as a template for restoring premorbid dimensions of the midface. , If simplification of the upper face has not yet been performed on an initial postoperative CT in a patient requiring staged surgery, fragments depressed more than 1 table width should be described on postoperative imaging. ,
The nasolacrimal duct
Postoperative CT assessment of the NLD does not have proved clinical value. The need for operative treatment of sequelae with dacryocystorhinostomy is based on persistence of symptoms (epiphora and recurrent dacryocystitis) beyond 6 months and confirmation with fluorescein dye or dacryocystogram. , If the NLD is reduced on postoperative CT, these sequelae may result from mucosal scarring and synechiae, which are not appreciable at CT. , This highlights the importance of recognizing both the strengths and limitations of postoperative imaging when communicating with facial reconstructive surgeons.
Zygomaticomaxillary complex fractures
Surgically Relevant Anatomic Considerations
The zygomaticomaxillary complex (ZMC) fracture fragment dissociates from the midface at 4 major points of failure: the zygomaticomaxillary buttress (ZMB), the zygomaticosphenoid suture (ZSS), frontozygomatic (FZ) suture, and zygomaticotemporal suture. , Because the lateral orbital floor almost always is involved, these fractures may be referred to orbitozygomatic fractures. The terms, malar fracture and tetrapod fracture , also sometimes are used. ,
The single most important feature of reduction quality on postoperative CT images is the status of the ZSS. , , , Telescoping or small changes in the axis of rotation of ZMC fractures about the ZSS lead to large increases in the bony orbital volume, potentially resulting in disfiguring enophthalmos. , Anatomic reduction of the ZSS along its entire oblique lateral orbital wall plane suggests anatomic reduction of the other aforementioned points of dissociation. The other involved sutures still should be assessed along with step-off at the orbital rim, particularly on coronal images. , Residual malar retrusion and offset about the ZMB on postoperative CT may result in poor aesthetic outcome, with asymmetric loss of lateral facial width and anterior projection.
Surgical Goals and Approach
The primary goals of ZMC fracture management are to restore premorbid facial symmetry and orbital configuration. , Repairs of the orbital floor may be performed with preformed (kit) implants following ZMC repair or may be performed as a staged surgery for several reasons. First, orbital surgery requires globe retraction and excellent visibility of the posterior orbit, which is limited in the presence of posttraumatic edema. , A 7-day to-14-day delay may be warranted to ensure correct orbital implant placement, particularly along the far-posterior palatine ledge. , Second, patient-specific laser sintered titanium implants created through 3-D printing techniques from the mirrored intact contralateral side usually are made at an outside facility and require time for interactive surgical preplanning between surgeons and vendor, manufacturing, and shipping.
Surgical approach is determined with the CT-based Zingg classification system and successive clinical assessment for fracture stability with each plate placement. , ,
Type A fractures involve a single limb of the zygoma (zygomatic arch—A1; lateral orbital wall—A2; and inferior orbital rim—A3). , Type A1 fractures typically exhibit a V-shaped depression of the zygomatic arch and are repaired for cosmetic and functional reasons because the arch can impinge on the mandibular coronoid process, limiting mouth opening and masticatory function. Commonly, a surgical hook or elevator is introduced into the infratemporal space through a posterior buccal incision. The fragments then snap back into anatomic alignment with surgical instrument pressure. , Open repair is risky because of the potential for facial nerve injury causing unilateral temporal hollowing. , , Types A2 and A3 fractures may be treated with observation or closed reduction if fragments are stable and cosmetically inapparent. If instability and/or visible deformity is present on examination, reduction and small plate fixation are performed through cosmetically favorable subconjunctival incisions for inferior rim fragments and brow or blepharoplasty incisions for lateral rim/wall reduction along the FZ suture , ( Fig. 6 ).

Zingg type B fractures are noncomminuted tetrapod fractures with a single liberated zygomatic fragment. Observation or closed reduction may be appropriate, especially in the elderly for whom the risks of surgery and anesthesia are elevated and the relative desirability of a perfect cosmetic result is lower. Follow-up CT in such patients may be performed to confirm stability following palpation; the lack of hardware should not be surprising.
When requiring internal fixation, 30% to 40% of type B fractures may be reduced and stabilized with a single plate. , , Fixation along the ZMB and FZ sutures are most common, utilizing intraoral and upper blepharoplasty incisions, respectively. , , ZMB plates are L-shaped and have a footplate for subapical fixation that avoids tooth roots. There is no convincing evidence that one single-plate fixation approach is better than another for isolated ZMC fractures. , Fixation at the second site is used if instability persists during intraoperative palpation , ( Fig. 7 ).

High-energy type C fractures with displacement and comminution are more likely to require fixation at a third site, in addition to orbital implant placement for concomitant large floor detects. Transconjunctival incisions have no external scar and are used for plating the inferior orbital rim in such cases. , The zygomatic arch rarely is plated except in the most unstable severely comminuted type C fractures that extend beyond the zygomaticotemporal buttress into the skull base. If stability cannot be achieved without zygomatic arch plating, access is achieved through coronal incisions and temporal muscle dissection , , ( Fig. 8 ). A summary of postoperative findings for ZMC fractures is listed in Table 2 .

| Postoperative Imaging Findings: Zygomaticomaxillary Complex Fractures | Clinical Rationale |
|---|---|
| Single-point fixation | Zingg type B fracture, stable after 1 fixation point. Preferred when feasible due to improved cosmesis. ZMB L-shaped plates commonly are used (protect tooth roots); FZ suture can also be used. Plate choice is surgeon-dependent.
|
| Two-point fixation | Zingg type B fracture, stable after 2-point fixation (typically, both ZMB and FZ suture plates) |
| Three-point fixation | Zingg type B or type C fracture, stable after 3-point fixation Inferior orbital rim fixation is performed only as part of a 3-point fixation if fracture remains unstable after 2-point fixation (stability ultimately determined in operating room based on continued mobility after successive plate placement). |
| Four-point fixation | Fixation along the ZMB, FZ, inferior orbital rim, and zygomatic arch Rare but requires coronal incision and temporalis dissection for ZA plate placement. Can cause unilateral temporal hollowing but approach may be unavoidable for high-energy comminuted fractures |
Postoperative Assessment of Reduction Quality and Complications
Changes in the bony orbital volume associated with misalignment about the ZSS can result in visible (greater than 2-mm) enophthalmos, which worsens following resolution of posttraumatic and postsurgical orbital edema. Revision often is necessary in such cases. If ZMC and internal orbital reconstruction are performed in stages, postoperative CT may reveal an orbital floor defect. , , Unlike pure internal orbital disruptions, the process of ZMC fracture reduction often results in shifting of orbital floor fracture fragments, causing an increase or decrease in size of the orbital floor defect, depending in part on the reduction maneuver used. , , Enophthalmos is the most common complication after both ZMC-related and pure orbital floor blowout fracture. The contribution of floor defects to enophthalmos is described later. The postoperative CT also should be examined for persistent internal rotation or malar retrusion that could result in postoperative malunion if uncorrected. , The soft tissues should be assessed for retrobulbar hematoma that could contribute to orbital compartment syndrome, evidenced by globe tenting from tension along the optic nerve. Treatment involves urgent lateral canthotomy at the bedside to relieve pressure.
Suppurative complications, including dehiscence, plate migration, osteomyelitis, and nonunion, are rare in the highly vascularized and immobile midface. The low infection rate also is related to gravity drainage of secretions away from the nondependent maxillary gingivobuccal sulcus. When infection occurs, this usually involves fixation hardware along the ZMB placed using an intraoral approach. ,
Orbital wall fractures
Surgically Relevant Anatomic Considerations
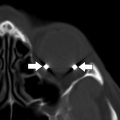
Although a detailed discussion of orbital anatomy is beyond the scope of this article, it is important to be aware of ledges and landmarks used as landing zones for orbital floor or combined floor and medial wall orbital implants. The junction of the lesser sphenoid wing with the orbital plate of the palatine bone forms a palatine ledge on which the implant rests posteriorly. The medial wall component of combined implants should ideally run in parallel and closely apposed to the intact portions of the lamina papyracea surrounding medial wall defects, coursing up toward the frontoethmoidal suture at the medial wall-roof junction ( Fig. 9 ).

Surgical Goals and Approach
Orbital floor and medial orbital wall fractures
Due to the potential for postoperative lid complications, including entropion or lid lag, surgery is considered only when the benefits of preventing enophthalmos outweigh the risks.
For every 1 mL of bony orbital volume change or tissue displacement beyond the orbital confines, 0.8 mm to 0.9 mm of enophthalmos results, , becoming noticeable when it exceeds 2 mm to 3 mm. Effective volume changes sufficient to cause visible enophthalmos occur with floor or medial wall surface area blowout of greater than 2 cm 2 , equating to approximately 25% to 50% floor or medial wall involvement. Collapse of the posterior junctional bulge can have a dramatic impact globe position, further magnifying the risk of clinically significant enophthalmos. CT guides decision making because the degree of enophthalmos is not evident clinically until edema has resolved and permanent soft-tissue architectural changes have begun to set in.
Blowout fractures are not self-reducing in adults, unlike in children, and extraocular muscle (EOM) incarceration and infarction is rare in adult patients. Entrapment of fibrofatty tissue within small (<3 mm) defects can cause EOM tethering in a small fraction of patients and may require orbital reconstruction if extraocular motility problems are confirmed with forced duction testing (the use of forceps to test for globe excursion following anesthetization of the sclera). , , ,
If surgery is necessary, prefabricated implants or 3-D–printed patient-specific implants (PSIs) reconstitute the frequently collapsed upward-sloping posterior bulge. There is growing evidence that PSIs provide the best aesthetic result.
Postoperative Assessment of Reduction Quality and Complications
Postoperative entrapment
Regardless of the type of implant used, ideally it should bridge the entire fracture defect and rest on all ledges on postoperative CT. Any space that persists between fracture ledges and the implant may result in herniation of EOMs or extraconal fibrofatty tissue, with potential for postoperative entrapment , , ( Fig. 10 ).