Resc rate (%)
5-year survey (%)
Local rec
10–30
30–45
Liver meta
40–50
35–45
Lung meta
20–30
40–50
24.2 Significance of C-Ion Radiotherapy
Improvements in tumor response and control have been sought through efforts to overcome the radioresistance of the hypoxic tumor cells identifiable in rectal cancers. These aspects might give high-LET particles a particular advantage, independent of whether this is due to a lower oxygen enhancement ratio (OER) or other intrinsic factors. Therefore, high-LET particle radiotherapy such as carbon ion or neutron radiotherapy may possess an advantage in the treatment of radioresistant and hypoxic, recurrent tumors. Twenty patients with recurrent rectal cancer were treated using the neutron generator in Munster by combined neutron radiotherapy [3].
The radiation schedule most often used for palliation involved giving 40 Gy photon and 10 Gy neutron doses (14 MeV). Initiation of pain relief appeared to occur faster with neutrons than with photons alone. Pain relief was achieved in 11–15 patients (73 %), and the probability for a pain-free period was 46 % at 9 months. It remains to be proven if a higher degree of pain relief, longer period of absence of pain, and length of progression-free period are improved with neutrons in comparison to photons. The incidence of acute toxicity was 30 % and late toxicity 10 %, with all reported toxicity occurring in the skin. A higher neutron dose may give better results, but its utility is potentially limited by well-recognized local radiation side effects. In contrast to neutrons, where escalation to tumoricidal doses is limited by potential normal tissue complications, carbon ion therapy offers the potential for an increase in biologically effective dose delivery in the target tissue relative to normal tissues through its superior dosimetric and radiobiological properties [4].
24.3 Clinical Trial in Recurrent Rectal Cancer at NIRS
The first clinical trial of the C-ion RT at the National Institute of Radiological Sciences (NIRS) for the recurrent rectal cancer was started in 2000. It was a phase I/II dose-searching study and the dose was escalated from the starting dose of 67.2 to 73.6 GyE in 16 fractions. A total of 38 patients were treated and the results indicated that the C-ion RT could be a sufficiently safe and effective treatment for the recurrent rectal cancer. This study was finished in 2004 and the second trial with the recommended dose determined by the first trial was initiated immediately. One hundred and fifty-two patients were treated in the second study until 2004 and the satisfactory results could be obtained as well. In November 2003 the approval of the Japanese government for the advanced medicine was given to the C-ion RT at the NIRS, and after the end of the second trial, the recurrent rectal cancer was added to the indication of the advanced medicine.
24.4 Methods of Carbon Ion Radiation Therapy at NIRS
24.4.1 Patient Immobilization
The patient needs to be immobilized for the C-ion RT as well as other tumor sites. The C-ion RT at the most heavy-ion therapy facilities is performed with fixed beam directions of vertical, horizontal, or 45-degree oblique. On the other hand, the recurrent tumor of the rectal cancer locates anywhere in the pelvis, at the presacral region, iliac lymph node, or mesenteric lymph node, and therefore the proper direction of the carbon ion beam is varied. Moreover, more than two ports are usually necessary to obtain satisfactory dose distribution in terms of avoidance of high dose to the bowels and the skin. Consequently, rather complicated immobilization is an everyday occurrence.
At the NIRS, it could be realized by using relatively thick low-temperature thermoplastic (Shellfitter; Keraray Co., Ltd., Osaka, Japan), sufficient amount of customized cradle (Moldcare; Alcare, Tokyo, Japan), and rotatable couch on the treatment bed.
Management of the respiratory motion is also essential in the most case of the recurrent rectal cancer (see Chaps. 4, 5, 6, 7, 8, and 9 Motion Management). There are plenty of methods for motion management. At the NIRS, synchronization with respiration is adopted at both CT acquisition and every session of the C-ion RT irrespective of direction of the beam. Although the influence of the respiratory motion on the session with the vertical beam is less than that with horizontal beam in the treatment of pelvic tumor, that is, mainly difference in the length of air gap, it is desirable to irradiate the tumor with similar condition to dose calculation using CT images taken at the expiratory phase.
24.4.2 Target Delineation
A set of 2.5–5.0-mm-thick CT images throughout the pelvis was taken for treatment planning, with the patient placed in immobilizing devices and with respiratory gating.
Clinical target volume (CTV) was determined by setting the margin 5 mm outside the GTV and included the regional lymph nodes (LN). The LN areas that should be considered the target volume include the internal iliac, the external iliac, and the presacral node. The dose constraints of the maximum dose for the intestine and bladder were 30 GyE in 9 fractions and 60 GyE in16 fractions, respectively. Prophylactic nodal areas of risk are usually treated to 37.8–41.4 GyE in 9 fractions of 4.2–4.6 GyE before irradiation field is reduced in size. The target volume includes the primary tumor, adjacent lymph nodes, and presacral region. Target volumes are based on known pattern of local recurrence in locally recurrent rectal cancer. MRI and methionine PET are useful to distinguish the tumor from postoperative fibrosis and the bowels.
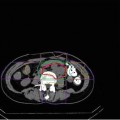
Planning target volume (PTV) is defined as the CTV plus at least 5 mm margin in all directions; however, the margins are modified if the critical organs, such as skin or bowels, exist near the tumor (Fig. 24.1).
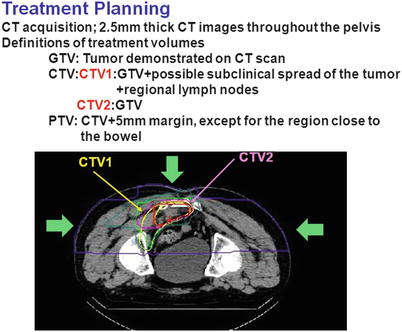
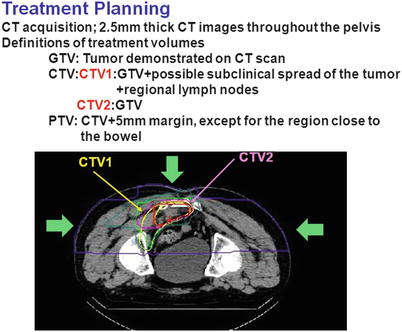
Fig. 24.1
The method of treatment planning for recurrent rectal cancer. Yellow line indicates the clinical target volume CTV) and red line indicates the planning target volume (PTV). The margins for the PTV is intentionally reduced to spare the bowels
24.4.3 Dose Prescription
The current recommended dose was 73.6 GyE/16 fractions as described above. One hundred percent of the prescribed dose is given at the maximum dose point of each portal. The treatment planning is performed so that the PTV is covered with at least 90 % of the prescribed dose. For this purpose, additional margins are necessary to determine the shape of collimator and compensation bolus. Figure 24.1 shows the representative dose distribution of current C-ion RT at the NIRS.
Major organs at risk (OAR) for this treatment are the bowels, sciatic nerve, urinary bladder, ureter, and skin. It is particularly important to spare the bowels from the high-dose area of the carbon ion beam. At the NIRS, dose constraints of the digestive tract are established based on the treatment results in the prostate, uterine cervical cancer, and the recurrent rectal cancer, where the maximum dose to the colon should not exceed 83 % of the prescribed dose. The sciatic nerve is also important OAR and the dose should be reduced as much as possible; however, control of the local tumor is much more important not only for the survival but also for the quality of life (QOL) of the patient. If the tumor is located close to the skin surface, the dose to the skin should also be taken into account. Selecting proper direction of the beam and using more than two ports are desirable, particularly in the treatment of big-sized lesion.
24.4.4 Field Positioning and Irradiation at NIRS
At the NIRS, the C-ion RT is carried out once a day, four fractions per week (from Tuesday to Friday). Verification of the field is carried out at every treatment session with a computer-aided online positioning system to maintain a positioning error of less than 2 mm. Fluoroscopic image is taken at the expiration phase of the patient respiration and compared with the reference images, such as the image taken at the preceded simulation or the digitally constructed radiograph (DRR). The C-ion RT is performed under respiration gating as described above, where the carbon ion beam is delivered only during the expiration phase.
24.5 Up-to-Date Results of the C-ion RT at NIRS
24.5.1 C-Ion Therapy for Patients with Pelvic Recurrence of Rectal Cancer
Between April 2001 and August 2012, 198 lesions at 189 patients were enrolled onto this study. Criteria for trial eligibility include confirmation of locally recurrent rectal cancers without distant metastases based on CT, MRI, and PET findings. The dose was determined as 67.2 GyE and escalated to 70.4 and 73.6 GyE. The predominant sites of relapse were 75 presacral, 77 lymph nodes, 28 perineal, and 9 anastomosis.
Ten patients received radiation dose at 67.2 GyE, 18(+3) at 70.4 GyE, and 161(+6) at 73.6 GyE. All toxicities in the 198 lesions at 189 patients were relatively few and mild in these patients. No grade 3–5 acute toxicity was observed. The local control rates in 197 lesions are 94 % at 3 years and 89 % at 5 years. Local control rates at 5 year were 97 % at 73.6 GyE. In terms of symptomatic response within 3 months after treatment, pain improved in 97 % of the symptomatic cases. The 3- and 5-year overall survival rates in 188 patients were 72 % and 47 %, respectively. Survival rates at 5 years were 20 % at 67.2 GyE, 24 % at 70.4 GyE, and 51 % at 73.6 GyE. In the literature, the reported 5-year survival rates for locally recurrent rectal cancer treated with conventional radiation and with resection were 0–40 % (Table 24.2) and 20–40 % (Table 24.3), respectively. Most of our patients were inoperable, so our results seem to be better than surgery.
Table 24.2
The results on the radiation therapy of locally recurrent rectal cancer reported by other studies
Study and reference | Year | Number | Rad dose(Gy) | Survival rate | Local control (%) | |
|---|---|---|---|---|---|---|
2 years (%) | 5 years (%) | |||||
Lybeert et al. [5] | 1992 | 76 | 6–66 | 61 (1 year) | 3 | 28 (3 years) |