Endoscopic sinus surgery is a minimally invasive option for the treatment of several nonneoplastic indications, particularly for medically refractory sinusitis and polyposis. Numerous interventions can be performed through endoscopic sinus surgery, many of which may be performed together during the same procedure. There are also a variety of complications that can result from endoscopic sinus surgery. Radiological imaging plays an important role in the evaluation of patients after endoscopic sinus surgery. Thus, it is important to be familiar with the expected and complicated imaging findings associated with endoscopic sinus surgery, which are reviewed in this article.
Key points
- •
Postoperative sinonasal diagnostic imaging techniques and protocols are reviewed.
- •
The different types of endoscopic sinus surgery techniques are described and the corresponding expected postoperative findings are presented.
- •
Complications resulting from endoscopic sinus surgery are summarized and selected examples of diagnostic imaging are presented.
Introduction
Endoscopic sinus surgery is a minimally invasive option for the treatment of several nonneoplastic indications, particularly for medically refractory sinusitis and polyposis. Numerous interventions can be performed through endoscopic sinus surgery ( Box 1 ), many of which may be performed together during the same procedure. There are also a variety of complications that can result from endoscopic sinus surgery ( Box 2 ). Radiological imaging plays an important role in the evaluation of patients after endoscopic sinus surgery. Thus, it is important to be familiar with the expected and complicated imaging findings associated with endoscopic sinus surgery, which are reviewed in this article.
Uncinectomy/uncinotomy
Inferior and middle meatus antrostomy/fenestration
Ethmoidectomy (anterior and/or posterior)
Turbinectomy/turbinate medialization
Frontal sinusotomy
Sphenoidotomy/sphenoid drill-out/marsupialization
Polypectomy
Sinus stenting
Mucocele drainage
Sinonasal debridement
Balloon sinuplasty
Turbinate reduction/turbinoplasty
Septoplasty/septorhinoplasty
Approach for ophthalmic procedures, such as orbital wall decompression, and anterior skull base cerebrospinal fluid (CSF) leak repair
Brain parenchymal injury and intracranial hemorrhage
Encephalocele and CSF leakage
Intracranial infection
Gossypiboma
Vascular injury (pseudoaneurysm)
Ophthalmic injury (intraorbital hemorrhage, extraocular muscle injury, optic nerve transection, nasolacrimal system disruption)
Periorbital lipogranuloma
Recurrent rhinosinusitis and polyposis
Retained septations
Neo-osteogenesis
Adhesions
Mucus recirculation phenomenon
Mucocele
Nasal septal perforation
Empty nose syndrome
Postoperative imaging techniques and protocols
The main radiological imaging modalities available for evaluating patients following endoscopic sinus surgery include computed tomography (CT), MR imaging, and angiography. High-resolution CT with multiplanar reconstructions is invaluable for a detailed depiction of the changes in bony anatomy and the presence of implants after surgery and can provide an overview of the extent of sinonasal opacification. CT can also be useful for screening orbital and intracranial complications. The administration of intravenous contrast with sinus CT is generally unnecessary, but can be helpful in cases of suspected orbital, facial, or intracranial infection. MR imaging often serves a complementary role to CT for optimal soft tissue characterization, particularly for delineating certain intracranial complications and further elucidating nonspecific findings on CT that are otherwise not readily amenable to endoscopic examination. Angiography, either in the form of CT angiography (CTA), MR angiography (MRA), or catheter angiography, is indicated for the evaluation of vascular complications. Notably, catheter angiography can serve as both a diagnostic and therapeutic modality in certain cases of postoperative hemorrhage. Fluoroscopy is mainly limited to guiding and verifying the completion of certain endoscopic procedures, such as balloon sinuplasty. Additional guidance for determining the appropriate imaging modalities can be found in the American College of Radiology Appropriateness Criteria for sinonasal disease. Protocol details for sinonasal CT and MR imaging techniques in adults are listed in Table 1 .
| Modality | Parameters |
|---|---|
| CT | Helical acquisition with 0.6-mm collimation at 200 mAs and 120 kVp in axial plane with 1-mm axial, coronal, and sagittal reformatted images using bone algorithm, and 3-mm axial, coronal, and sagittal reformatted images using soft tissue algorithm |
| MR imaging |
|
Types of surgery and imaging findings
Ostiomeatal Unit Endoscopic Sinus Surgery
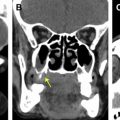
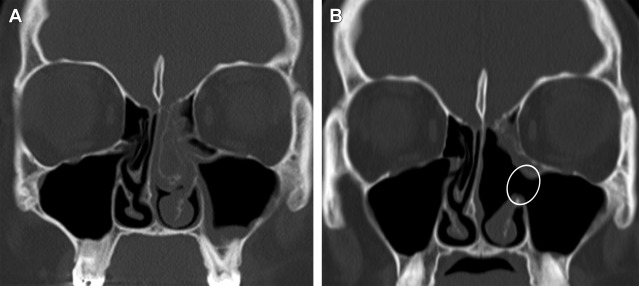
The goal in treating an obstructed ostiomeatal unit via endoscopic surgery is to improve mucociliary clearance by removing anatomic obstacles. The procedure most typically involves uncinectomy and middle meatal antrostomy, which creates a wide neoinfundibulum that is best delineated on coronal CT images ( Fig. 1 ). Variable degrees of ethmoidectomy and middle turbinectomy may also be performed, depending on the extent of disease; for example, medial deviation of the lamina papyracea with or without posterior repositioning of the globe frequently occurs after ethmoidectomy because of the loss of buttressing effects ordinarily provided by the ethmoid septations. The medial bowing of the lamina papyracea can be observed on postoperative CT and is generally on the order of a 1-mm to 3-mm decrease in the interorbital distance ( Fig. 2 ). Another less commonly implemented option for treating patients with ostiomeatal unit complex diseases is inferior antrostomy, which provides an alternate drainage pathway and can be useful in cases of severe disease that cannot be addressed through the usual uncinectomy and middle meatal antrostomy. This procedure results in a defect in the inferior nasoantral wall that can mimic a secondary ostium ( Fig. 3 ).


Frontal Sinusotomy and Stenting
Frontal sinusotomy is indicated when frontal sinus disease persists despite more conservative endoscopic approaches directed at the infundibulum and anterior ethmoid region. The Draf classification describes various types of endoscopic frontal sinusotomy based on the extent of surgical resection of the regional sinonasal skeleton ( Table 2 ). The postoperative status of the frontoethmoid recess is best delineated on sagittal and coronal CT images. For example, frontal sinus stenting is indicated if the neo-ostium measures less than 5 mm in width, and CT can be useful for verifying the position of the stents ( Fig. 4 ) and assessing surrounding anatomy if further surgery is contemplated.
| Category | Findings |
|---|---|
| Draf 1 | Simple drainage: complete resection of the anterior ethmoid cells and uncinate process surrounding the frontal recess to the frontal ostium |
| Draf 2 | Extended drainage: resection of the floor of the frontal sinus from the nasal septum medially to the lamina papyracea laterally (can be difficult to distinguish from Draf 1 on CT) |
| Draf 3 (modified Lothrop procedure) | Resection of the superior nasal septum and entire frontal sinus floor |

Sphenoidotomy
Endoscopic sphenoidotomy is commonly performed to address disease that involves the sphenoid sinus and can be achieved without or with ethmoidectomy and other endoscopic sinus surgery. The main approaches for accessing the sphenoid sinus include widening the natural ostium or creating a second opening through the posterior ethmoid sinuses. In either case, CT can show a widened communication between the sphenoid and ethmoid sinuses, which is most conspicuous on axial and sagittal reformatted images ( Fig. 5 ). Marsupialization is another option for treating chronically infected sphenoid sinus and consists of exteriorizing the affected sinus. Furthermore, sphenoid drill-out may also be performed for chronic sinusitis and can be considered as an intermediate procedure between sphenoidotomy and sphenoid marsupialization. Regardless of the technique that is implemented, the goal is improved aeration of the sphenoid sinus.

Balloon Sinuplasty
Balloon sinuplasty is a minimally invasive endoscopic treatment that involves dilating the paranasal ostia while minimizing mucosal damage. The inflated balloon delicately displaces, microfractures, and molds the bone surrounding the sinus outflow and may be used alone or in combination with conventional endoscopic surgery. Fluoroscopic imaging guidance can be used to visualize the position and expansion of the contrast-filled balloon, which appears radio-opaque ( Fig. 6 ).

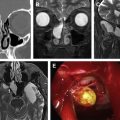
Mucocele Drainage
Endoscopic techniques can be effective for treating paranasal sinus mucocele, including those with orbital extension, thereby often obviating an trans-orbital approach. In addition to clearing the affected paranasal sinus contents of the mucocele, packing material, stents, or spacers are sometimes placed and may be observed on imaging obtained soon after surgery ( Fig. 7 ). Postoperative CT can be useful to evaluate for residual mucocele components and the status of the paranasal sinus walls, whereas MR imaging can be appropriate for delineating intracranial or intraorbital extension. Following successful mucocele drainage, remineralization of the affected paranasal sinus walls can be observed and associated proptosis can diminish.