Potential Role of Proton Therapy in the Management of Lymphoma
Nancy Price Mendenhall
Daniel Yeung
The radiation doses required to secure local control in lymphomas are in the range of 30 Gy to 40 Gy, modest in comparison to those required for local control in carcinomas or sarcomas.1, 2, 3 These doses have produced only a few immediate normal tissue toxicities, and have therefore been generally regarded as safe and tolerable. However, with increasing survivorship in lymphomas, late effects of radiation have emerged in tissues receiving doses previously regarded as below the threshold for normal tissue injury.4 In some cases, it appears that the injury is related to substantial cell loss in tissues receiving moderate radiation doses, whereas in other cases, the injury appears to be related to cell damage from low radiation doses manifested as second malignancies many years after the radiation exposure. Because of the perception of a high therapeutic ratio with radiation therapy in lymphomas, lymphomas have not been considered as a high priority for proton therapy. In addition, the wide variety of presentations and complex patterns of tumor involvement make the technical aspects of proton delivery for lymphomas challenging. Consequently, to date there is little experience in using proton therapy for lymphomas.
There have been several case reports of the use of protons in the management of lymphomas. Kirsch et al.5 from the Massachusetts General Hospital reported on proton treatment a young patient with Hodgkin’s disease involving the sacrum who was treated with combined modality chemoradiation. Protons were used in lieu of photons to minimize the radiation dose to the remainder of the pelvis in a female adolescent in an attempt to minimize the late effects of radiation therapy. The group from Loma Linda reported on the treatment a 53-year-old patient with a large B-cell lymphoma of the cavernous sinus with sphenoid sinus and clival extension, treated with partial resection, CHOP-R chemotherapy, and proton beam irradiation.6 Conformal protons were utilized to minimize the volume of normal brain receiving radiation. Conformal proton beam radiotherapy to a moderate dose proved valuable in this case because it minimized the volume of normal brain receiving low to moderate doses of radiation.
Probably the presentation offering the most potential for an increased therapeutic ratio with proton therapy is the large mediastinal mass in Hodgkin’s lymphoma, because of the well described late cardiopulmonary risks of radiation therapy7 for lymphoma that might be decreased with the use of protons.8 The emergence of increasing problems related to both high and low radiation doses to normal tissues in lymphoma survivors presents an opportunity for
improved outcomes accruing from the improved radiation dose distributions possible with proton therapy.
improved outcomes accruing from the improved radiation dose distributions possible with proton therapy.
LARGE MEDIASTINAL MASS IN HODGKIN’S LYMPHOMA
One of the most common presentations in Hodgkin’s lymphoma is that of mediastinal involvement, usually in conjunction with neck and or axillary involvement, in both men and women between the ages of 15 and 30. Involvement of the mediastinum has consistently been associated with a poor prognosis, likely because patients are asymptomatic and diagnosis is delayed until the disease is sufficiently extensive to produce B symptoms, airway or vascular compression, or pain. There is more of a consensus on the need for consolidative radiation therapy after chemotherapy in patients with large mediastinal masses than any other presentation.9 At the same time, mediastinal radiation in lymphomas is associated with most of the major toxicities which one would hope to avoid in lymphoma management. These toxicities include acute and late pulmonary toxicity related to both volume of lung exposed to radiation and dose,10 coronary artery disease, seemingly associated with radiation dose, valve dysfunction associated with radiation dose,11 second malignancies,12 particularly breast cancer, associated with the volume of breast and overall tissue exposed as well as the dose absorbed.
Even with radiation therapy, in-field recurrence is not uncommon. The causes for treatment failure after radiation therapy are not always clear, but include geographic miss related to unappreciated patterns of subtle spread, inconsistent dose delivery related to complexity of field shape, setup variability, and organ motion, and normal tissue constraints limiting prescribed dose. True radiation resistance is rare in Hodgkin’s lymphoma, so technologic solutions to target definition, delivery error, and prescription constraints offer significant promise for an improvement in the therapeutic ratio. If target definition and delivery errors can be addressed, then protons may offer significant promise in the management of mediastinal disease in the lymphomas.
TREATMENT OF MEDIASTINAL LYMPHOMA
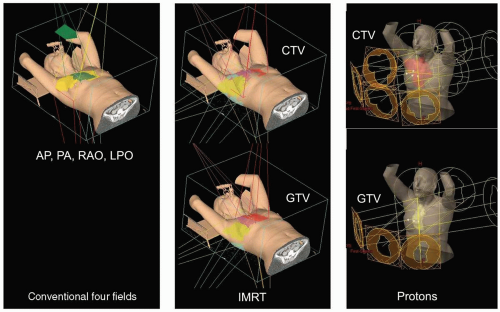
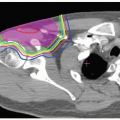
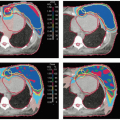
Figure 22.1 shows the treatment field arrangements for conventional, IMRT, and proton treatment plans designed to treat an involved field, including all areas of initial involvement, with the standard modification to reduce the lateral borders of the mediastinal field to cover only the residual postchemotherapy volume. A dose of 30 Gy was
prescribed to all areas of initial disease and a dose of 40 Gy to the area of residual mediastinal radiographic abnormality. Figure 22.2 shows the coronal and sagittal projections of the conventional, IMRT, and proton treatment plans. Figure 22.3 shows the axial treatment plans at three levels. Table 22.1 and Figure 22.4 show dose-volume histogram (DVH) comparisons of the three plans with respect to target coverage and normal tissue exposure; the proton plan offers significant decreases in dose to the coronary arteries, valves, lung, breast, and total body.
prescribed to all areas of initial disease and a dose of 40 Gy to the area of residual mediastinal radiographic abnormality. Figure 22.2 shows the coronal and sagittal projections of the conventional, IMRT, and proton treatment plans. Figure 22.3 shows the axial treatment plans at three levels. Table 22.1 and Figure 22.4 show dose-volume histogram (DVH) comparisons of the three plans with respect to target coverage and normal tissue exposure; the proton plan offers significant decreases in dose to the coronary arteries, valves, lung, breast, and total body.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree