Clinical PET/MR imaging is currently performed at a number of centers around the world as part of routine standard of care. This article focuses on issues and considerations for a clinical PET/MR imaging program, focusing on routine standard-of-care studies. Although local factors influence how clinical PET/MR imaging is implemented, the approaches and considerations described here intend to apply to most clinical programs. PET/MR imaging provides many more options than PET/computed tomography with diagnostic advantages for certain clinical applications but with added complexity. A recurring theme is matching the PET/MR imaging protocol to the clinical application to balance diagnostic accuracy with efficiency.
Key points
- •
PET/MR imaging is in routine clinical use at multiple sites in the United States, Europe, and Asia.
- •
Clinical PET/MR imaging protocols include whole-body (WB) PET/MR imaging, regional PET/MR imaging, and a combination of WB and regional PET/MR imaging.
- •
Most oncologic PET/MR imaging studies include WB standard-of-care PET as well as regional standard-of-care MR imaging.
- •
PET acquisition and MR imaging sequences should be tailored to the clinical question, to maximize efficiency, and minimize the overall image acquisition time.
Workflow, protocolling, reporting and billing
The workflow for clinical PET/MR imaging studies has similarities to PET/computed tomography (CT) and MR imaging studies but requires coordination at the scheduling, technologist, and interpreting physician levels, which may not exist initially. As few technologists, radiologist, and nuclear medicine physicians have trained in the era of PET/MR imaging, it is often necessary to have personnel with PET expertise to closely work with those with MR imaging expertise and to cross-train in the modality they are less familiar with. Many programs begin by performing crossover studies with patients undergoing clinical PET/CT studies then immediately afterward undergoing PET/MR imaging studies with the same radiopharmaceutical administration. An example of a clinical PET/MR imaging workflow is shown schematically in Fig. 1 .

There are some considerations with clinical PET/MR imaging studies that differ from PET/CT and MR imaging. Many PET/MR imaging studies involve standard-of-care PET and MR imaging studies that must be precertified. The need for precertification can slow the scheduling of PET/MR imaging studies compared with PET/CT or MR imaging studies, which in turn may be frustrating to referring physicians and patients. In some clinical practices, radiology schedulers perform the precertification, which can reduce the burden on the referring physician’s office. Another consideration is that some patients will not be able to complete the PET/MR imaging examination because of the length of the study and/or claustrophobia. Ideally, PET/CT would be available as a backup so that the PET radiopharmaceutical administration will not be wasted and expose the patient to radiation without providing diagnostic information.
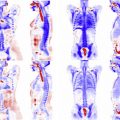
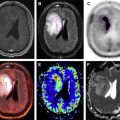
Most institutions select patients with standard-of-care indications for both PET and MR imaging for evaluation through PET/MR imaging studies. For oncology, the protocol often consists of a whole-body (WB) PET along with WB-MR imaging for staging and a regional diagnostic MR imaging examination for assessment of the primary tumor and/or regional nodal staging. As with PET/CT, the WB component is typically varied depending on the type and location of the tumor with typical WB coverage from skull base to midthigh (most solid tumors), skull vertex to midthigh (eg, head and neck cancers), skull vertex to knee (eg, multiple myeloma, some melanomas), or skull vertex to toes (eg, some melanomas and malignancies of the lower extremities). For brain and cardiac PET/MR imaging studies, both the PET and the MR imaging acquisitions are typically regional only without a WB component. This approach reduces the overall time required for patient imaging (1 session instead of 2), allows simultaneous review of both PET and MR imaging studies by the interpreting physicians, and can streamline the diagnostic imaging process. For some patients, PET/MR imaging is performed for standard-of-care PET indications without a diagnostic MR imaging component. A common reason to perform PET/MR imaging without a diagnostic MR imaging examination is for dose reduction in children and young adults by replacing WB CT with MR imaging for attenuation correction (AC) and anatomic localization.
The PET protocol for simultaneous PET/MR imaging studies involves selecting the appropriate PET tracer for the indication as well as the region to be covered by PET (limited, skull base to midthigh, WB). Table 1 provides a list of the Food and Drug Administration (FDA)–approved PET tracers and their primary clinical applications. Most PET studies in the United States are for oncologic indications and use the glucose analogue 2-deoxy-2-[ 18 F]fluoro- d -glucose ([ 18 F]FDG). The MR imaging protocol for simultaneous PET/MR imaging involves the MR imaging sequences for the WB-PET/MR imaging portion of the study and/or the protocol for the regional MR imaging protocol. For PET/MR imaging studies that include a diagnostic MR imaging component, the protocol is typically based on the same protocol used for MR imaging–only examinations, although some sequences may be omitted or adapted to reduce the total amount of time required for the PET/MR imaging examination. Depending on the training of those involved, the PET protocolling may be done by nuclear medicine, whereas the MR imaging protocolling is typically done by the appropriate radiology subspecialty.
| PET Tracer | Primary Clinical Applications |
|---|---|
| [ 13 N]Ammonia | Myocardial perfusion |
| [ 11 C]Choline chloride | Detection and staging of recurrent prostate cancer |
| [ 18 F]FDG | Cancer diagnosis, staging and treatment response Neuroimaging for epilepsy and dementia Cardiac imaging for myocardial viability Inflammation and infection |
| [ 68 Ga]DOTATATE | Somatostatin-receptor positive tumors, especially neuroendocrine tumors |
| [ 18 F]Florbetaben | Detection of brain amyloid |
| [ 18 F]Florbetapir | Detection of brain amyloid |
| [ 18 F]Fluciclovine | Detection and staging of recurrent prostate cancer |
| [ 18 F]Flutemetamol | Detection of brain amyloid |
| [ 82 Rb]Rubidium chloride | Myocardial perfusion |
| Sodium [ 18 F]fluoride | Skeletal scintigraphy for osseous metastases |
The interpretation of PET/MR imaging requires fusion of PET with multiple MR imaging sequences, and several commercially available software packages are suitable for this purpose. However, some software packages that work well for PET/CT are not readily adapted to PET/MR imaging because of the need to fuse the PET images with mutli-planar, multi-sequence MR imaging acquisitions and to work with relatively large numbers of image series. Local practice pattern will determine how PET/MR imaging studies are interpreted. At some institutions, the PET portion of the study is read by nuclear medicine and the diagnostic MR imaging portion is read by the appropriate radiology subspecialty. This strategy can provide the highest level of subspecialty expertise for each component of the study but requires coordination and discussion before issuing the PET/MR imaging report. Alternatively, a single reader with appropriate training may read the entire study. The Society of Nuclear Medicine and Molecular Imaging and the American College of Radiology (ACR) are in the process of developing practice standards for interpreting PET/MR imaging studies and have issued guidelines for neuroimaging with PET/MR imaging.
Reporting of PET/MR imaging studies that include standard-of-care PET and diagnostic regional MR imaging can be reported separately or as a single integrated report. Some institutions use separate reports for the PET and MR imaging components to facilitate billing. When separate reporting is performed, the WB MR imaging findings are typically included with the PET report in a similar fashion to the CT portion of PET/CT studies. The findings should be harmonized if separate reports are issued, and the PET and MR imaging reports should cross-reference each other for clarity in the medical record and for the ordering physician. Billing in the United States is based on the appropriate PET-only Current Procedural Terminology ( CPT ) code (78811, 78112, 78813) and MR imaging CPT codes. Currently, no PET/MR imaging–specific CPT codes are available as there are for PET/CT. Although systematic data regarding billing and reimbursement for PET/MR imaging are not available, most centers performing clinical PET/MR imaging report similar reimbursement for PET/MR imaging as for their PET/CT and MR imaging studies.
Workflow, protocolling, reporting and billing
The workflow for clinical PET/MR imaging studies has similarities to PET/computed tomography (CT) and MR imaging studies but requires coordination at the scheduling, technologist, and interpreting physician levels, which may not exist initially. As few technologists, radiologist, and nuclear medicine physicians have trained in the era of PET/MR imaging, it is often necessary to have personnel with PET expertise to closely work with those with MR imaging expertise and to cross-train in the modality they are less familiar with. Many programs begin by performing crossover studies with patients undergoing clinical PET/CT studies then immediately afterward undergoing PET/MR imaging studies with the same radiopharmaceutical administration. An example of a clinical PET/MR imaging workflow is shown schematically in Fig. 1 .
There are some considerations with clinical PET/MR imaging studies that differ from PET/CT and MR imaging. Many PET/MR imaging studies involve standard-of-care PET and MR imaging studies that must be precertified. The need for precertification can slow the scheduling of PET/MR imaging studies compared with PET/CT or MR imaging studies, which in turn may be frustrating to referring physicians and patients. In some clinical practices, radiology schedulers perform the precertification, which can reduce the burden on the referring physician’s office. Another consideration is that some patients will not be able to complete the PET/MR imaging examination because of the length of the study and/or claustrophobia. Ideally, PET/CT would be available as a backup so that the PET radiopharmaceutical administration will not be wasted and expose the patient to radiation without providing diagnostic information.
Most institutions select patients with standard-of-care indications for both PET and MR imaging for evaluation through PET/MR imaging studies. For oncology, the protocol often consists of a whole-body (WB) PET along with WB-MR imaging for staging and a regional diagnostic MR imaging examination for assessment of the primary tumor and/or regional nodal staging. As with PET/CT, the WB component is typically varied depending on the type and location of the tumor with typical WB coverage from skull base to midthigh (most solid tumors), skull vertex to midthigh (eg, head and neck cancers), skull vertex to knee (eg, multiple myeloma, some melanomas), or skull vertex to toes (eg, some melanomas and malignancies of the lower extremities). For brain and cardiac PET/MR imaging studies, both the PET and the MR imaging acquisitions are typically regional only without a WB component. This approach reduces the overall time required for patient imaging (1 session instead of 2), allows simultaneous review of both PET and MR imaging studies by the interpreting physicians, and can streamline the diagnostic imaging process. For some patients, PET/MR imaging is performed for standard-of-care PET indications without a diagnostic MR imaging component. A common reason to perform PET/MR imaging without a diagnostic MR imaging examination is for dose reduction in children and young adults by replacing WB CT with MR imaging for attenuation correction (AC) and anatomic localization.
The PET protocol for simultaneous PET/MR imaging studies involves selecting the appropriate PET tracer for the indication as well as the region to be covered by PET (limited, skull base to midthigh, WB). Table 1 provides a list of the Food and Drug Administration (FDA)–approved PET tracers and their primary clinical applications. Most PET studies in the United States are for oncologic indications and use the glucose analogue 2-deoxy-2-[ 18 F]fluoro- d -glucose ([ 18 F]FDG). The MR imaging protocol for simultaneous PET/MR imaging involves the MR imaging sequences for the WB-PET/MR imaging portion of the study and/or the protocol for the regional MR imaging protocol. For PET/MR imaging studies that include a diagnostic MR imaging component, the protocol is typically based on the same protocol used for MR imaging–only examinations, although some sequences may be omitted or adapted to reduce the total amount of time required for the PET/MR imaging examination. Depending on the training of those involved, the PET protocolling may be done by nuclear medicine, whereas the MR imaging protocolling is typically done by the appropriate radiology subspecialty.
| PET Tracer | Primary Clinical Applications |
|---|---|
| [ 13 N]Ammonia | Myocardial perfusion |
| [ 11 C]Choline chloride | Detection and staging of recurrent prostate cancer |
| [ 18 F]FDG | Cancer diagnosis, staging and treatment response Neuroimaging for epilepsy and dementia Cardiac imaging for myocardial viability Inflammation and infection |
| [ 68 Ga]DOTATATE | Somatostatin-receptor positive tumors, especially neuroendocrine tumors |
| [ 18 F]Florbetaben | Detection of brain amyloid |
| [ 18 F]Florbetapir | Detection of brain amyloid |
| [ 18 F]Fluciclovine | Detection and staging of recurrent prostate cancer |
| [ 18 F]Flutemetamol | Detection of brain amyloid |
| [ 82 Rb]Rubidium chloride | Myocardial perfusion |
| Sodium [ 18 F]fluoride | Skeletal scintigraphy for osseous metastases |
The interpretation of PET/MR imaging requires fusion of PET with multiple MR imaging sequences, and several commercially available software packages are suitable for this purpose. However, some software packages that work well for PET/CT are not readily adapted to PET/MR imaging because of the need to fuse the PET images with mutli-planar, multi-sequence MR imaging acquisitions and to work with relatively large numbers of image series. Local practice pattern will determine how PET/MR imaging studies are interpreted. At some institutions, the PET portion of the study is read by nuclear medicine and the diagnostic MR imaging portion is read by the appropriate radiology subspecialty. This strategy can provide the highest level of subspecialty expertise for each component of the study but requires coordination and discussion before issuing the PET/MR imaging report. Alternatively, a single reader with appropriate training may read the entire study. The Society of Nuclear Medicine and Molecular Imaging and the American College of Radiology (ACR) are in the process of developing practice standards for interpreting PET/MR imaging studies and have issued guidelines for neuroimaging with PET/MR imaging.
Reporting of PET/MR imaging studies that include standard-of-care PET and diagnostic regional MR imaging can be reported separately or as a single integrated report. Some institutions use separate reports for the PET and MR imaging components to facilitate billing. When separate reporting is performed, the WB MR imaging findings are typically included with the PET report in a similar fashion to the CT portion of PET/CT studies. The findings should be harmonized if separate reports are issued, and the PET and MR imaging reports should cross-reference each other for clarity in the medical record and for the ordering physician. Billing in the United States is based on the appropriate PET-only Current Procedural Terminology ( CPT ) code (78811, 78112, 78813) and MR imaging CPT codes. Currently, no PET/MR imaging–specific CPT codes are available as there are for PET/CT. Although systematic data regarding billing and reimbursement for PET/MR imaging are not available, most centers performing clinical PET/MR imaging report similar reimbursement for PET/MR imaging as for their PET/CT and MR imaging studies.
MR imaging and radiation safety
The location and facilities housing a PET/MR imaging scanner should follow institutional and national guidelines regarding MR imaging and radiation safety, which includes adherence to the MR imaging zones I to IV to ensure patient safety. The waiting room for the PET/MR imaging scanner should follow guidelines to be an MR imaging zone I with patient prescreening taking place in MR imaging zone II. Patients undergoing PET/MR imaging should be routinely prescreened before entering MR imaging zones III and IV by appropriately qualified and trained personnel. Only patients deemed safe to undergo MR imaging should be allowed into zones III and IV, always with supervision by the technologists. Because personnel working in PET/CT centers may not be as familiar with MR imaging safety guidelines as MR imaging technologists, particular care should be taken to ensure the use of MR–compatible patient monitoring devices to avoid the risk of metallic projectiles in the PET/MR suite.
Implantable devices are a common issue in regard to MR imaging safety. At this time, all FDA-approved PET/MR imaging scanners operate at 3 Tesla (T). At the authors’ institution, patients are required to provide documentation of the exact model and make of any implantable devices or to have documentation available in their medical records. Once the specific device is identified, information from the manufacturer and from online resources, such as MRIsafety.com , is available to determine safety in a 3-T magnetic field. Implanted pacemakers and automatic implantable cardioverter-defibrillators (AICDs) are historically a general contraindication to MR imaging. However, a growing body of research has demonstrated safety of certain implanted cardiac devices in MR imaging scanners. In regard to PET/MR imaging, a major issue remains that implanted cardiac device safety is predominantly demonstrated in 1.5-T MR, and there may be insufficient evidence for some devices to support safety in a 3-T MR imaging scanner.
Several MR imaging and PET safety concerns remain unique to women, the most common relating to pregnancy and lactation. Although MR imaging has been deemed safe during pregnancy, the current “ACR Guidance Document on MR Safe Practices” states that MR imaging should only be considered in pregnant women if other imaging modalities without ionizing radiation will not provide appropriate clinical information, the information is likely to alter patient care, and the examination cannot be delayed until after pregnancy. It is the authors’ institutional policy to obtain informed consent from any patient undergoing MR imaging while pregnant regarding the theoretic risks and benefits of the MR imaging procedure. Additionally, the radiation risks during pregnancy and potential benefit from the PET study should be discussed with the referring physician and patients, and PET/MR imaging may be preferable for pregnant patients because of the lack of additional radiation dose from CT. For young women with intrauterine devices, standard prescreening protocols should be undertaken as described earlier.
Gadolinium-based contrast is generally considered a very safe contrast medium, with very few adverse reactions observed. However, the administration of gadolinium-based contrast media to patients with severe chronic renal disease (glomerular filtration rate <30), acute kidney injury, and pregnant patients is contraindicated. Standard institutional policies should be undertaken to screen for renal dysfunction in patients at high risk to minimize the risk of the development of nephrogenic systemic fibrosis. Several studies have demonstrated minimal excretion of gadolinium into breast milk, and the ACR “Manual on Contrast Media” deems MR imaging with gadolinium-based contrast safe for breastfeeding women without cessation of lactation for any period of time. However, it is often necessary to temporarily interrupt breastfeeding to limit the infant’s effective dose from the PET tracer to less than 1 mSv (100 mrem). The length of cessation will depend on the PET tracer and the amount of activity administered and should meet federal, state, and institutional regulations and policy.
A unique MR imaging safety concern to PET/MR imaging is the ability to shield and administer intravenous agents (radiopharmaceuticals and contrast) in an MR imaging–compatible fashion. Care should be undertaken so that all shielding material is MR imaging compatible, and there are reports of lead shielding moving under the influence of a strong magnetic field. Tungsten-based MR imaging–compatible syringe shields have been developed for use in the PET/MR imaging environment and are commercially available. Similarly, cardiac monitoring systems and automated injectors for PET radiopharmaceuticals must be MR imaging compatible. The areas for storing and handling PET radiopharmaceuticals should be configured in accordance with institutional, state, and national guidelines and does not differ from the setup used for a PET/CT suite. Standard technologist PET radiation safety protocols should be undertaken in accordance with state and national guidelines and also do not differ from PET/CT.
PET/MR imaging offers the advantage of performing the anatomic imaging portion of the examination without ionizing radiation. Although ionizing radiation from the radiopharmaceutical used for PET is inevitable, previous studies have demonstrated that up to 70% of the radiation dose of a PET/CT is due to the CT dose, although the CT dose can be lowered depending on the acquisition technique. The high sensitivity of current PET/MR imaging systems as well as the potential to acquire PET data for a longer period of time during MR imaging sequence acquisition have the potential to reduce the radiation dose to patients related to the radiopharmaceutical.
Whole-body PET/MR imaging acquisition
This section focuses on WB protocols designed for simultaneous PET/MR imaging, although many of the same considerations apply to sequential PET/MR imaging systems. The primary clinical use of WB PET/MR imaging is currently for cancer staging; thus, oncologic PET/MR imaging is the focus of this section. Other applications, such as evaluating for systemic infectious and inflammatory processes, are relevant as well but are less commonly performed in routine clinical practice. There is a lack of clear consensus among PET/MR imaging users regarding a core WB protocol, and no large studies comparing the diagnostic accuracy of different WB MR imaging protocols used with PET/MR imaging for specific clinical applications have been published.
Comparison of Whole-Body PET/MR Imaging and PET/Computed Tomography Protocols
There are several important differences between PET/CT and PET/MR for WB imaging. With PET/CT, typically a low-dose CT scan is acquired for anatomic localization and AC, followed by the PET acquisition. At some institutions, diagnostic CT examinations with intravenous contrast may be performed as well. The technologist must manipulate either the PET or CT field of view (FOV) to ensure proper alignment and adhesion regarding start/stop times and locations. A relatively new technology in PET/CT called continuous bed motion allows technologists to prescribe both FOV simultaneously and has the potential to decrease scan time and radiation dose. Because PET/CT is a sequential image acquisition, PET/CT motion artifacts and misregistration can occur. WB-PET/MR acquisition requires the technologist to accurately place body coils before beginning the study. Next, a WB localizer scan is needed for anatomic layout and PET bed placement. Finally, desired MR sequences are assigned to each PET bed. Each bed contains its own MRAC map scan as well as any additional MR imaging sequences in the protocol. An example of console settings for a WB PET/MR imaging study is shown in Fig. 2 .