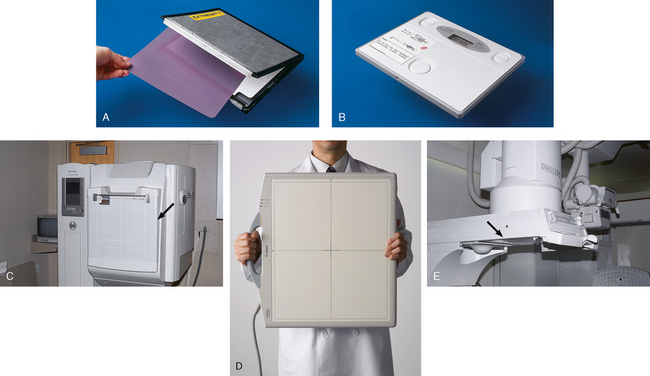
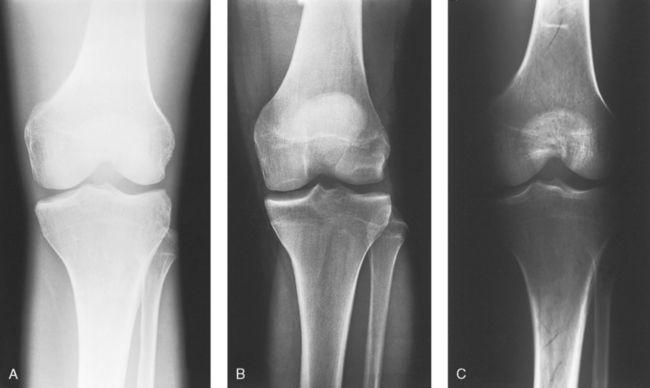
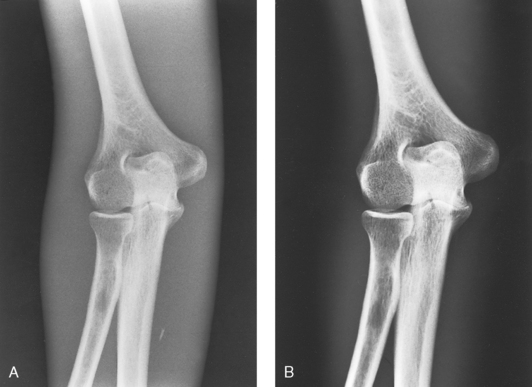
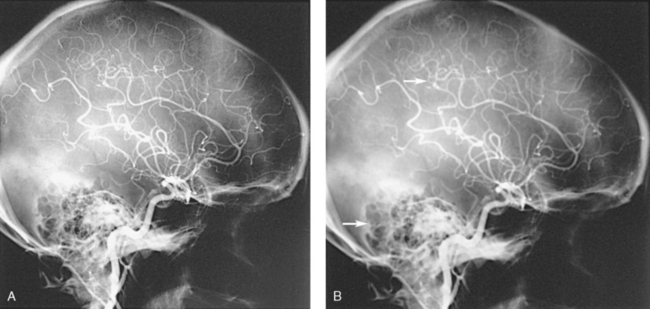
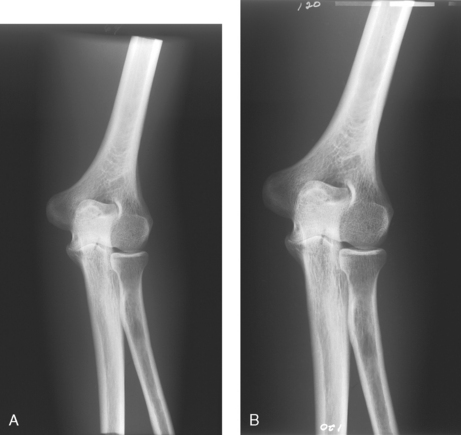
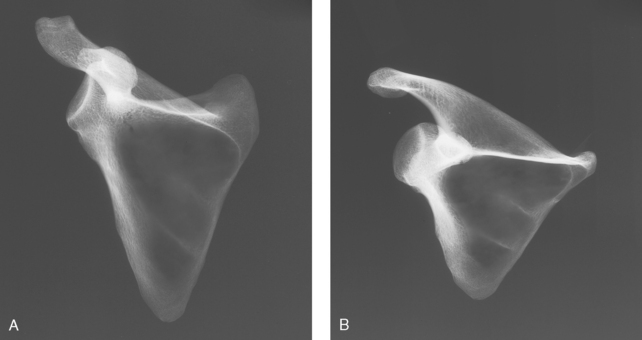
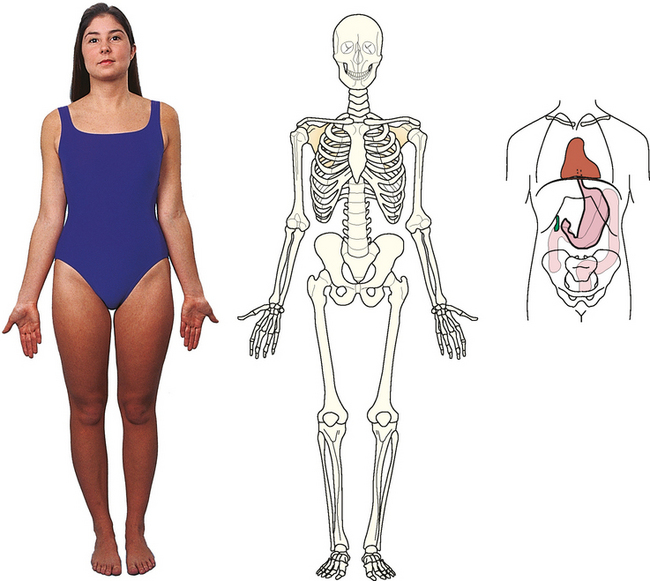
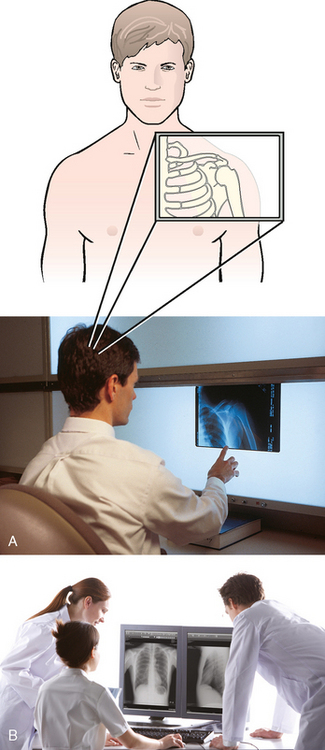
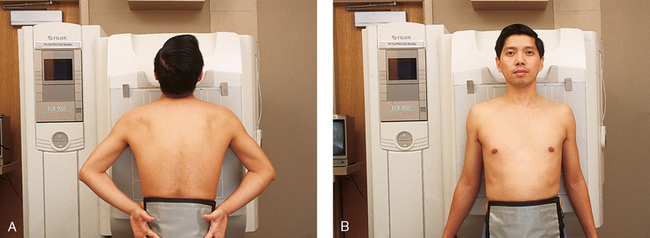
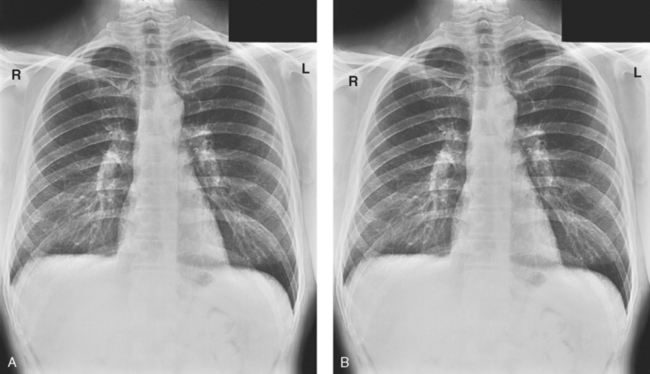
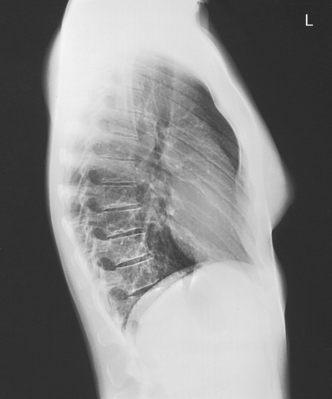
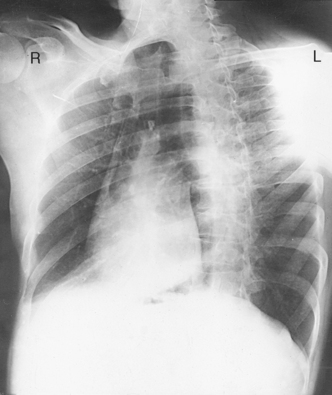
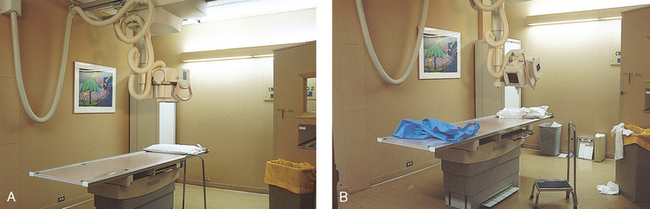
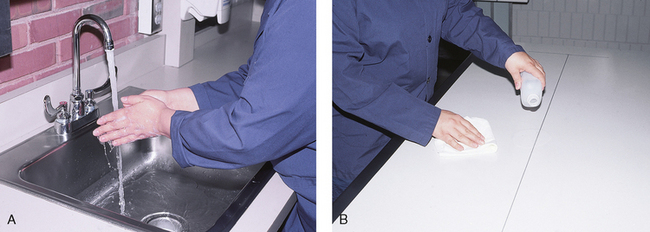
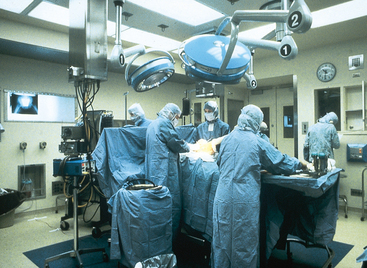
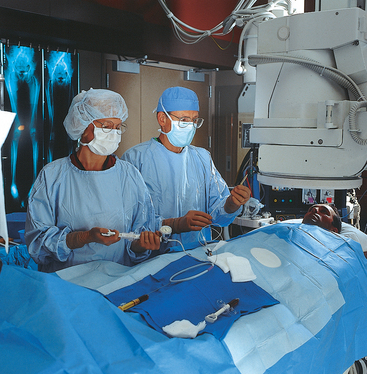
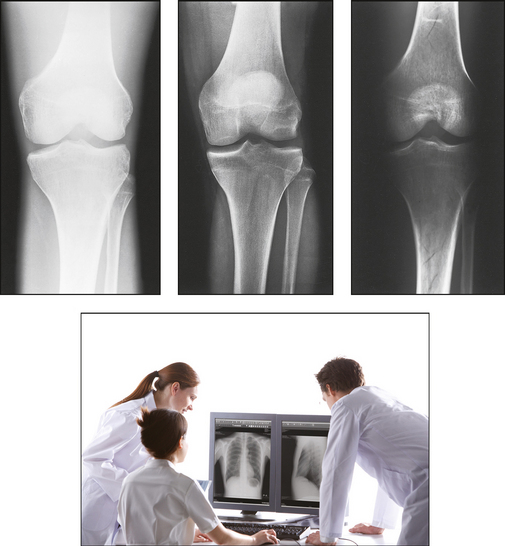
1 Ethics in radiologic technology Diagnosis and the radiographer Care of the radiographic examining room Centers for Disease Control and Prevention Minor surgical procedures in the radiology department Patient’s attire, ornaments, and surgical dressings English-metric conversion and film sizes Source–to–image receptor distance Foundation exposure techniques and charts Adaptation of exposure technique to patients Working effectively with obese patients The American Society of Radiologic Technologists (ASRT) developed the current code of ethics.1 The Canadian Association of Medical Radiation Technologists (CAMRT) has adopted a similar code of ethics.2 All radiographers should familiarize themselves with these codes. 1. The radiologic technologist conducts himself or herself in a professional manner, responds to patient needs, and supports colleagues and associates in providing quality patient care. 2. The radiologic technologist acts to advance the principal objective of the profession to provide services to humanity with full respect for the dignity of humankind. 3. The radiologic technologist delivers patient care and service unrestricted by concerns of personal attributes or the nature of the disease or illness, and without discrimination, regardless of gender, race, creed, religion, or socioeconomic status. 4. The radiologic technologist practices technology founded on theoretic knowledge and concepts, uses equipment and accessories consistent with the purpose for which they have been designed, and employs procedures and techniques appropriately. 5. The radiologic technologist assesses situations; exercises care, discretion, and judgment; assumes responsibility for professional decisions; and acts in the best interest of the patient. 6. The radiologic technologist acts as an agent through observation and communication to obtain pertinent information for the physician to aid in the diagnosis and treatment management of the patient. He or she recognizes that interpretation and diagnosis are outside the scope of practice for the profession. 7. The radiologic technologist uses equipment and accessories; employs techniques and procedures; performs services in accordance with an accepted standard of practice; and demonstrates expertise in minimizing radiation exposure to the patient, self, and other members of the health care team. 8. The radiologic technologist practices ethical conduct appropriate to the profession and protects the patient’s right to quality radiologic technology care. 9. The radiologic technologist respects confidence entrusted in the course of professional practice, respects the patient’s right to privacy, and reveals confidential information only as required by law or to protect the welfare of the individual or the community. 10. The radiologic technologist continually strives to improve knowledge and skills by participating in educational and professional activities, sharing knowledge with colleagues, and investigating new and innovative aspects of professional practice. The code of ethics, adopted in June 1991, requires all members to do the following: • Provide service with dignity and respect to all people regardless of race, national or ethnic origin, color, gender, religion, age, type of illness, and mental or physical challenges. • Encourage the trust and confidence of the public through high standards of professional competence, conduct, and appearance. • Conduct all technical procedures with due regard to current radiation safety standards. • Practice only those procedures for which the necessary qualifications are held unless such procedures have been properly delegated by an appropriate medical authority and for which the technologist has received adequate training to an acceptable level of competence. • Practice only those disciplines of medical radiation technology for which he or she has been certified by the CAMRT and is currently competent. • Be mindful that patients must seek diagnostic information from their treating physician. In those instances where a discreet comment to the appropriate authority may assist diagnosis or treatment, the technologist may feel morally obliged to provide one. • Preserve and protect the confidentiality of any information, either medical or personal, acquired through professional contact with the patient. An exception may be appropriate when the disclosure of such information is necessary to the treatment of the patient or the safety of other patients and health care providers or is a legal requirement. • Cooperate with other health care providers. • Advance the art and science of medical radiation technology through ongoing professional development. • Recognize that the participation and support of our association is a professional responsibility. 1. Cassette with film: A device that contains special intensifying screens that glow when struck by x-rays and imprints the x-ray image on film. The use of a darkroom, where the film is developed in a processor, is required. Afterward the radiographic film image is ready for viewing on an illuminator (Fig. 1-1, A). 2. Image plate (IP): A device, used for computed radiography (CR), similar to a conventional intensifying screen. The IP is housed in a specially designed cassette that contains special phosphorus to store the x-ray image. The IP is a component of the new “digital” imaging systems. The cassette is inserted into a reader device, which scans the IP with a laser. The radiographic image is converted to digital format and is viewed on a computer monitor or printed on film (Fig. 1-1, B). 3. Solid-state detectors: A flat panel thin-film transistor (TFT) detector or a charge-coupled device (CCD) used for direct digital radiography (DR). This type of digital imaging system is called “cassetteless” because it does not use a cassette or an IP. The flat panel detector or CCD built into the x-ray table or other device captures the x-ray image and converts it directly into digital format. The image is viewed on a computer monitor or printed on film (Fig. 1-1, C). This is the fastest processing system with images available in 6 seconds or less. The DR flat panel detector is a component of the new “digital” imaging systems. 4. Portable digital radiography: A portable, lightweight DR system that can be used for lateral and axial imaging of limbs and for trauma and bedside applications. Its 14 × 17 inches (35 × 43 cm) size is large enough for chest and abdomen images. The unit can be tethered to the computer via Ethernet, or the newest systems allow wireless transmission (Fig. 1-1, D). 5. Fluoroscopic screen: X-rays strike a fluoroscopic screen, where the image is formed and is transmitted to a television monitor via a camera. This is a “real-time” device in which the body part is viewed live on a television (Fig. 1-1, E). 1. Superimposition: The relationship of the anatomic superimposition to size, shape, position, and angulation must be reviewed. 2. Adjacent structures: Each anatomic structure must be compared with adjacent structures and reviewed to ensure that the structure is present and properly shown. 3. Optical density (OD): OD is known as degree of blackening when associated with radiographic film and as brightness when describing appearance on a digital display monitor. The OD must be within a “diagnostic range” to display all desired anatomic structures. Images with ODs outside the diagnostic range (too light or too dark) are primarily associated with screen-film radiography (Fig. 1-2), although they are possible with digital imaging. The primary controlling factor for screen-film OD is milliampere-second (mAs). For digital imaging, the OD of displayed images is primarily controlled by automatic rescaling, so mAs selection affects patient radiation dose and image noise. 4. Contrast: The contrast, or the difference in density between any two areas on a radiograph, must be sufficient to allow radiographic distinction of adjacent structures with different tissue densities. A wide range of contrast levels is produced among the various radiographic examinations performed (Fig. 1-3). A low-contrast image displays many density levels, and a high-contrast image displays few density levels. The primary controlling factor of radiographic contrast is kilovoltage peak (kVp). 5. Recorded detail: The recorded detail, or the ability to visualize small structures, must be sufficient to show clearly the desired anatomic part (Fig. 1-4). Recorded detail is primarily controlled by the following: 6. Magnification: The magnification of the body part must be evaluated, taking into account the controlling factors of object–to–image receptor distance (OID), or how far the body part is from the IR, and source–to–image receptor distance (SID), or how far the x-ray tube is from the IR. All radiographs yield some degree of magnification because all body parts are threedimensional (Fig. 1-5). 7. Shape distortion: The shape distortion of the body part must be analyzed, and the following primary controlling factors must be studied: An example of shape distortion is when a bone is projected longer or shorter than it actually is. Distortion is the misrepresentation of the size or shape of any anatomic structure (Fig. 1-6). Radiographs are usually oriented on the display device so that the person looking at the image sees the body part placed in the anatomic position. The anatomic position refers to the patient standing erect with the face and eyes directed forward, arms extended by the sides with the palms of the hands facing forward, heels together, and toes pointing anteriorly (Fig. 1-7). When the radiograph is displayed in this manner, the patient’s left side is on the viewer’s right side and vice versa (Fig. 1-8). Medical professionals always describe the body, a body part, or a body movement as though it were in the anatomic position. Fig. 1-9, A, illustrates the anterior (front) aspect of the patient’s chest placed closest to the IR for a posteroanterior (PA) projection. Fig. 1-9, B, illustrates the posterior (back) aspect of the patient’s chest placed closest to the IR for an anteroposterior (AP) projection. Regardless of whether the anterior or posterior body surface is closest to the IR, the radiograph is usually placed in the anatomic position (Fig. 1-10). (Positioning terminology is fully described in Chapter 3.) Exceptions to these guidelines include the hands, fingers, wrists, feet, and toes. Hand, finger, and wrist radiographs are routinely displayed with the digits (fingers) pointed to the ceiling. Foot and toe radiographs are also placed on the illuminator with the toes pointing to the ceiling. Hand, finger, wrist, toe, and foot radiographs are viewed from the perspective of the x-ray tube, or exactly as the anatomy was projected onto the IR (Figs. 1-11 and 1-12). This perspective means that the individual looking at the radiograph is in the same position as the x-ray tube. Lateral radiographs are obtained with the patient’s right or left side placed against the IR. The patient is generally placed on the illuminator in the same orientation as though the viewer were looking at the patient from the perspective of the x-ray tube at the side where the x-rays first enter the patient—exactly like radiographs of the hands, wrists, feet, and toes. Another way to describe this is to display the radiograph so that the side of the patient closest to the IR during the procedure is also the side in the image closest to the illuminator. A patient positioned for a left lateral chest radiograph is depicted in Fig. 1-13. The resulting left lateral chest radiograph is placed on the illuminator as shown in Fig. 1-14. A right lateral chest position and its accompanying radiograph would be positioned and displayed the opposite of that shown in Figs. 1-13 and 1-14. Oblique radiographs are obtained when the patient’s body is rotated so that the projection obtained is not frontal, posterior, or lateral (Fig. 1-15). These radiographs are viewed with the patient’s anatomy placed in the anatomic position (Fig. 1-16). Fig. 1-15 A patient placed in left anterior oblique (LAO) position for PA oblique projection of chest. • Normal anatomy and normal anatomic variations so that the patient can be accurately positioned • The radiographic characteristics of numerous common abnormalities When the physician does not see the patient, the radiographer is responsible for obtaining the necessary clinical history and observing any apparent abnormality that might affect the radiographic result (Fig. 1-17). Examples include noting jaundice or swelling, body surface masses possibly casting a density that could be mistaken for internal changes, tattoos that contain ferrous pigment, surface scars that may be visible radiographically, and some decorative or ornamental clothing. The physician should give specific instructions about what information is necessary if the radiographer assumes this responsibility. The radiographic room should be prepared for the examination before the patient arrives. The room should look clean and organized—not disarranged from the previous examination (Fig. 1-18). Fresh linens should be put on the table and pillow, and accessories needed during the examination should be placed nearby. Performing these preexamination steps requires only a few minutes but creates a positive, lasting impression on the patient; not performing these steps beforehand leaves a negative impression. Handwashing is the easiest and most convenient method of preventing the spread of microorganisms (Fig. 1-19, A). Radiographers should wash their hands before and after working with each patient. Hands must always be washed, without exception, in the following specific situations: • After examining patients with known communicable diseases • After coming in contact with blood or body fluids • Before beginning invasive procedures When the examination is finished, the contaminated linen should be folded with the clean side out and returned to the patient’s room with the patient. There the linen receives the special attention given to linen used for isolation unit patients or is disposed of according to the established policy of the institution. All radiographic tables must be cleaned after patients have touched it with their bare skin and after patients with communicable diseases have been on the table (Fig. 1-19, B). For the protection of health care workers, the U.S. Centers for Disease Control and Prevention (CDC)1 has issued recommendations for handling blood and other body fluids. According to the CDC, all human blood and certain body fluids should be treated as if they contain pathogenic microorganisms (Box 1-1). These precautions should apply to all contacts involving patients. Health care workers should wear gloves whenever they come into contact with blood, mucous membranes, wounds, and any surface or body fluid containing blood. For any procedure in which blood or other body fluids may be sprayed or splashed, the radiographer should wear a mask, protective eyewear (e.g., eye shields, goggles), and a gown. Health care workers must be cautious to prevent needle stick injuries. Needles should never be recapped, bent, broken, or clipped. Instead, they should be placed in a puncture-proof container and properly discarded (Fig. 1-20). After checking the room setup, the radiographer should thoroughly wipe the x-ray equipment with a damp (not soaked) cloth before taking it into the OR. The radiographer moves the mobile machine, or C-arm unit, to the free side of the operating table—the side opposite the surgeon, scrub nurse, and sterile layout (Fig. 1-21). The machine should be maneuvered into a general position that makes the final adjustments easy when the surgeon is ready to proceed with the examination. The radiographer should make the necessary arrangements with the OR supervisor when performing work that requires the use of a tunnel or other special equipment. When an IR is being prepared for the patient, any tunnel or grid should be placed on the table with the tray opening to the side of the table opposite the sterile field. With the cooperation of the surgeon and OR supervisor, a system can be developed for performing radiographic examinations accurately and quickly without moving the patient or endangering the sterile field (Fig. 1-22). Procedures that require a rigid aseptic technique, such as cystography, intravenous urography, spinal punctures, angiography, and angiocardiography, are performed in the radiology department (Fig. 1-23). Although the physician needs the assistance of a nurse in certain procedures, the radiographer can make the necessary preparations and provide assistance in many procedures. Patient motion plays a large role in radiography (Fig. 1-24). Because motion is the result of muscle action, the radiographer needs to have some knowledge about the functions of various muscles. The radiographer should use this knowledge to eliminate or control motion for the exposure time necessary to complete a satisfactory examination. The three types of muscular tissue that affect motion are the following:
PRELIMINARY STEPS IN RADIOGRAPHY
Ethics in Radiologic Technology
AMERICAN SOCIETY OF RADIOLOGIC TECHNOLOGISTS CODE OF ETHICS
CANADIAN ASSOCIATION OF MEDICAL RADIATION TECHNOLOGISTS CODE OF ETHICS
Image Receptor
Radiograph
ANATOMIC POSITION
Posteroanterior and anteroposterior radiographs
Lateral radiographs
Oblique radiographs

Clinical History
Care of the Radiographic Examining Room
Standard Precautions
Centers for Disease Control and Prevention
Operating Room
Minor Surgical Procedures in the Radiology Department
Motion and Its Control
PRELIMINARY STEPS IN RADIOGRAPHY