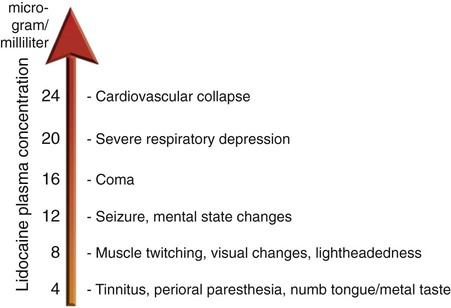
Chapter 19 Ali Albayati and Andres Krauthamer As the need for interventional radiologic procedures continues to grow, there is increased interest in better periprocedural pain control. Interventional radiology (IR) plays a significant role in pain management, both therapeutically (for chronic pain) and supplementally (for pain caused by intervention). Pain management is essential as IR practice becomes more invasive, readily available, and widely offered1 to individuals at “high risk” for both operative procedures and anesthesia. One of the most noticeable changes in medical management is the migration toward more outpatient procedures, which has increased interest in providing sedation and analgesia modalities suitable to the outpatient setting, such as intraprocedural moderate sedation or monitored anesthesia care.2 Some of the vascular surgical procedures for instance, can be performed with a combination of locoregional techniques and intravenous (IV) conscious sedation.3 As a result, interventional radiologists and anesthesiologists face a variety of new challenges in ensuring the safety and comfort of their patients. Pain management is also important because it reduces patient discomfort and anxiety. The interventionalist should obtain a proper history and physical examination and should discuss the procedure and pain management plan with all parties involved, including the patient and the nurse team member assigned to that particular procedure. Preprocedural consultation with an anesthesiologist is essential when there are ongoing or expected risk factors in terms of the patient’s age, clinical status, unstable vital signs, complex intervention, or the potential for significant periprocedural pain. A point of caution is that during complex procedures, it is possible that numerous doses of intraprocedural analgesics and sedatives will be required to overcome stress and pain; this may result in deeper than intended postprocedure sedation after elimination of the procedure’s painful stimuli. This can be avoided by adequate planning and communication with other disciplines. While a more active role for anesthesiologists in IR is being sought, the availability of anesthesia personnel to cover these procedures varies greatly among institutions.4 There is considerable overlap among the types of analgesia and/or sedation currently available. The determination of which is best is based on the type of procedure being performed, patient clinical status, patient preference, interventionalist preference, and availability of an anesthesiologist. The American Society of Anesthesiologists (ASA) Task Force on Sedation and Analgesia by Non-Anesthesiologists has developed practice guidelines5 that define sedation and analgesia as a continuum that ranges from minimal sedation through general anesthesia (Table 19-1). Anesthesiologists recognize this continuum and thus are generally able to develop an anesthetic plan that meets the changing needs of the interventionalist. There are four main options of locoregional anesthesia and sedation available to the interventional patient: TABLE 19-1 Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/Analgesia Adapted from American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 2002;96:1004–17. 1. Local anesthesia is indicated for minor procedures and includes infiltration of a local anesthetic to the region of planned procedure; there is no associated sedation. The patient will be fully awake. A subtype of this option is therapeutic (e.g., to eliminate a patient’s chronic pain). A local anesthetic may be mixed with steroid and injected into a degenerative joint. 2. Sedation is indicated for most interventional radiology procedures and is coadministered with local anesthesia. There two main subtypes of sedation for this option: • Moderate “conscious” sedation will produce a state of decreased awareness with maintained protective reflexes. It is usually administered by the IR critical care nurse. The most frequently used combination of medications for moderate sedation is midazolam with fentanyl. • Monitored anesthesia care (MAC) is a deeper sedation administered by the anesthesiologist. Propofol is generally the first choice of anesthesiologists for MAC sedation. According to the ASA, MAC is differentiated from “moderate sedation” because it is provided by an individual trained to proceed to general anesthesia if necessary.6 Moderate sedation has no such requirement, and deeper levels of sedation or progression to general anesthesia are never the goal. 3. Regional anesthesia includes administration of local anesthetic to block main nerve trunks. There are two subtypes: • Segmental anesthesia (i.e., epidural anesthesia) is frequently provided by the anesthesiologist. • Nerve block can be an effective therapeutic technique. It is used to ameliorate chronic radicular pain when injected at the intervertebral foramina to block exiting spinal nerves. 4. General anesthesia is the deepest level of sedation and characterized by a state of unconsciousness, analgesia, anxiolysis, and amnesia. It is provided and maintained by the anesthesiologist and involves loss of response to painful stimuli and loss of the protective airway reflexes. The patient will not be able to recall procedural events. Because of advances in monitoring and pharmaceutical agents, anesthesiologists rarely hear the statement “the patient is too sick for anesthesia.” There are no defined contraindications for the patient to undergo some form of anesthesia. We are, however, occasionally presented with patients who are at such great risk for anesthetic morbidity and mortality that a careful discussion of the risk/benefit ratio of the proposed procedure should be undertaken before proceeding. Additionally, unless the procedure is emergent, all patients should be optimized medically before proceeding with elective procedures, including nothing-by-mouth status.5 Immediate access to resuscitation equipment and drugs should be available anywhere sedative or analgesic drugs are administered. There is a thorough summary of equipment and pharmaceutical agents that should be immediately accessible in the ASA Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists.5 If radiology is involved in the purchase of anesthesia equipment (e.g., anesthesia machines, monitoring equipment, infusion pumps), it is recommended that equipment be magnetic resonance imaging (MRI) compatible for maximum flexibility. Strong consideration should be given to the purchase and constant use of capnography to assess patient ventilation. Continuous capnography is an ASA standard for all patients undergoing general anesthesia and is generally used by anesthesiologists to assess ventilation in all MAC cases. Capnography has been shown to improve outcome when used for moderate sedation cases.7 In contrast, chest plethysmography, commonly used in interventional suites as a means of assessing respiration, can artifactually indicate ventilation when in fact the patient’s airway is obstructed and no gas exchange is occurring. Medical conditions consistently shown to increase perioperative risk include advanced age, emergent procedures,8 history of ischemic heart disease or congestive heart failure, renal insufficiency, and diabetes mellitus.9 One of the most consistent systems for predicting perioperative risk9 is the ASA Physical Status Classification System (Table e19-1). Not only is the ASA classification predictive of outcome, it is also straightforward, allows physicians and other team members to use a common terminology, and can be helpful in the preoperative categorization and preparation of patients. There are four important concepts regarding sedation and analgesia for interventional patients: 1. Any analgesic or sedative agent can produce a state of unresponsiveness given a large enough dose. Again, this is the concept of a continuum between minimal sedation and general anesthesia, and patients may intentionally or unintentionally progress along this continuum during the course of one anesthetic. 2. When analgesic and sedative agents are given in combination, their effects are synergistic. This is why, for example, patients may be given a single agent such as morphine for pain relief in an unmonitored setting. Administer the morphine with valium, however, and the patient is at increased risk for respiratory compromise and should be in a monitored setting. 3. There is huge variability in patient sensitivity to analgesics and sedatives. In postsurgical patients, there is up to a 10-fold difference in morphine dose required for postoperative analgesia.10 The elderly are particularly sensitive to all sedative/analgesic agents. Rather than have “fixed” dosage protocols for certain procedures, anesthetic agents should be titrated to obtain the desired level of sedation for each individual patient, and nursing protocols should be designed to accommodate this. 4. Deeply sedated patients may be adequately stimulated to continue ventilating during the interventional study. Close attention must be paid to these patients after the procedure, however, once the painful stimulus is removed. Patients may then be at increased risk for respiratory depression and apnea at a time when they may be less closely monitored. TABLE e19-1 American Society of Anesthesiologists Physical Classification System Local anesthetics reversibly interrupt neural conduction by blocking sodium channels located on internal neuronal membranes. This results in inhibition of sodium permeability necessary for action potential propagation and pain signal formation.11 All local anesthetics are subdivided clinically into two classes of drugs, the aminoesters and the aminoamides. The aminoesters have an ester linkage between the aromatic end and the intermediate chain. Ester-type local anesthetics undergo rapid metabolism through plasma pseudocholinesterase. These drugs include cocaine, procaine, benzocaine, and tetracaine. The aminoamides contain an amide linkage between the aromatic end and the intermediate chain. These drugs include lidocaine, bupivacaine, mepivacaine, prilocaine, and etidocaine. Amide-type local anesthetics undergo oxidative dealkylation via the hepatic cytochrome P450 enzyme system, as well as conjugation. As such, the clearance of lidocaine and bupivacaine is highly dependent on hepatic blood flow, extraction, and enzyme function. Caution with the use of large volumes is advised in patients with liver dysfunction.12 Adverse reactions associated with local anesthetics may arise from direct toxicity, reaction to an added vasoconstrictor or preservative, or allergic reaction. Toxicities result from high blood levels of local anesthetic, usually as a consequence of accidental intravascular injection, increased uptake from perivascular areas, or overdose. Common adverse reactions associated with local anesthetics include central nervous system toxicity, cardiovascular toxicity, neuronal toxicity, vasoconstrictor reactions, and allergic reactions.13 Prevention of such reactions is contingent on both appropriate dosage administration, clinical vigilance for early detection of toxic reactions, and prevention methods such as syringe aspiration for blood prior to injection of the anesthetic. Lidocaine (Lidocaine HCL [Hospira Inc., Lake Forest, Ill.]) was the first clinically used aminoamide local anesthetic, introduced into clinical practice by Nils Löfgren, a Swedish chemist. Lidocaine remains the most widely used agent because of its inherent potency, short latency, tissue penetration, and intermediate duration of action. Lidocaine concentration is expressed in percentage as grams per 100 mL (e.g., lidocaine 1% is 1 g/100 mL, which is 10 mg/mL). Available concentrations range from 0.5% to 5%. At concentrations of 0.5% to 1%, lidocaine provides local anesthesia with a duration of 1 to 2 hours. Lidocaine’s versatility is demonstrated by clinical application for almost any regional anesthetic application. It is effective in infiltration, providing topical anesthesia, a peripheral nerve block, and both epidural and spinal blocks. There is a spectrum of toxicities directly related to the lidocaine serum concentration (Fig. 19-1).1,14
Principles of Intraprocedural Analgesics and Sedatives
Techniques for Providing Analgesia and Sedation
Minimal Sedation (Anxiolysis)
Moderate Sedation/Analgesia (Conscious Sedation)
Deep Sedation/Analgesia
General Anesthesia
Responsiveness
Normal response to verbal stimulation
Purposeful response to verbal or tactile stimulation
Purposeful response after repeated or painful stimulation
Unarousable, even with painful stimulus
Airway
Unaffected
No intervention required
Intervention may be required
Intervention often required
Spontaneous ventilation
Unaffected
Adequate
May be inadequate
Frequently inadequate
Cardiovascular function
Unaffected
Usually maintained
Usually maintained
May be impaired

Contraindications to Analgesia and Sedation
Equipment
![]() Please visit www.expertconsult.com for a full discussion of this topic.
Please visit www.expertconsult.com for a full discussion of this topic.
Precautions for Providing Analgesia and Sedation
![]() Please visit www.expertconsult.com for a full discussion of this topic.
Please visit www.expertconsult.com for a full discussion of this topic.
Class
Description
I
A normal healthy patient
II
A patient with mild systemic disease
III
A patient with severe systemic disease
IV
A patient with severe systemic disease that is a constant threat to life
V
A moribund patient who is not expected to survive without the operation
VI
A declared brain-dead patient whose organs are being removed for donor purposes
Pharmacology of Analgesic and Sedative Agents Commonly Used in Interventional Radiology
Local Anesthetics
![]() For more information on the primary pharmacology of local anesthetics, please visit www.expertconsult.com.
For more information on the primary pharmacology of local anesthetics, please visit www.expertconsult.com.
Lidocaine
Principles of Intraprocedural Analgesics and Sedatives